Background
Pulmonary artery sling is a rare defect created by anomalous origin of the left pulmonary artery from the posterior aspect of the right pulmonary artery. The anomalous left pulmonary artery courses over the right mainstem bronchus and then from right to left, posterior to the trachea or carina and anterior to the esophagus, to reach the hilum of the left lung. This compresses the lower trachea and right mainstem bronchus, producing upper airway symptoms. Compression caused by the sling can produce obstructive emphysema, atelectasis of the right and left lungs, or both. Thus, early recognition and diagnosis of pulmonary artery sling, and of stridor in a young infant, are crucial.
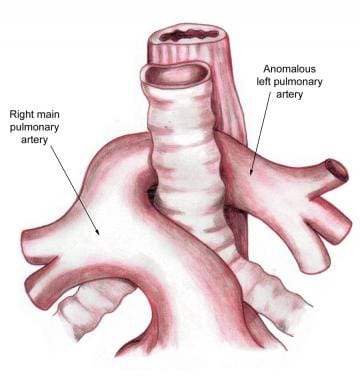
An example of pulmonary artery sling is shown in the illustration below.
Associated tracheobronchial abnormalities may occur, especially complete tracheal rings and tracheomalacia. Hypoplasia and stenosis of tracheal segments occur and can potentiate the airway obstruction. Congenital heart defects are found in 50% of pulmonary artery sling cases, most commonly atrial septal defect, patent ductus arteriosus, ventricular septal defect, and left superior vena cava.
Other organ system abnormalities may occur. These include imperforate anus, Hirschsprung disease, biliary atresia, and genitourinary defects. Abnormalities of ovaries, vertebrae, thyroid gland, and pulmonary parenchyma have been reported.
The specific etiology of the pulmonary artery sling is unknown.
Pathophysiology
As the left pulmonary artery passes posteriorly and caudally to the right main-stem bronchus and to the left behind the trachea, tracheal and bronchial compression occurs. The course of the anomalous left pulmonary artery to the right of the trachea produces deviation of the lower trachea to the left with resulting compression of the right mainstem bronchus and lower trachea. This results in airway obstruction that primarily affects the right lung, although compression of the lower trachea and left mainstem bronchus can result in bilateral obstruction.
Other abnormalities in the arterial supply to one or both lungs can be seen in association with this abnormality. On occasion, the anomalous pulmonary artery may supply only the left upper lobe with normal pulmonary arterial supply to the left lower lobe. In addition, partial anomalous supply of the right upper lobe of the lung from the anomalous left pulmonary artery has been described.
Epidemiology
Owing to the relative rarity of this condition, the true incidence and frequency of pulmonary artery sling in the United States and globally is not known. A retrospective study showed a hospital-based prevalence of 0.14% for left pulmonary artery sling among Chinese patients with congenital heart disease. [1]
Race-, sex-, and age-related demographics
No racial or sex predilection is known.
Symptoms, including respiratory distress manifested by stridor, recurrent pneumonia, wheezing, and cyanosis, typically occur within the first month of life. Dysphagia is rare, but obstructive apnea may occur. These patients tend to be more symptomatic and to present even earlier than those with a vascular ring due to a double aortic arch.
Prognosis
With early diagnosis and surgical correction, the prognosis is good. [2] Surgical mortality is increased by coexisting tracheal or bronchial stenosis.
Surgical survivors may be free of significant symptoms at long-term follow-up; however, because many demonstrate some persistent airway obstruction, they should be closely observed for both airway as well as pulmonary artery complications.
Morbidity/mortality
In severely affected infants, death can occur in the early months of life. Survival is unlikely without surgical intervention. Mortality varies and has been reported to be relatively high in previous studies. The major contributor to postoperative mortality is the high frequency of bronchial and tracheal abnormalities in this group of patients. Early, aggressive intervention may minimize the mortality caused by these associated lesions. [3]
Morbidity includes frequent episodes of stridor and respiratory distress with or without wheezing and cyanosis. Recurrent pneumonia can occur.
Complications
Because of associated tracheomalacia, tracheal stenosis, and/or bronchial stenosis, postoperative symptoms of airway obstruction are common. Left pulmonary artery stenosis may occur and can be progressive.
Patient Education
Parents should be educated about issues with regard to airway obstruction and tracheobronchial toilet. Patients in the immediate postoperative period still may be at risk during respiratory illnesses because of increased secretions. Over time, with healing and improvement of the tracheomalacia/tracheal stenosis, these symptoms should improve.
No preventive measures are known.
-
Slide tracheoplasty and left PA sling repair. Procedure performed by Giles Peek MD, FRCS, CTh, FFICM, The Children’s Hospital at Montefiore, Bronx, NY. Video courtesy of Montefiore.
-
Aberrant left pulmonary artery or pulmonary artery sling.