Background
Constrictive pericarditis occurs when a thickened fibrotic pericardium, of whatever cause, impedes normal diastolic filling. [1] This usually involves the parietal pericardium, although it can involve the visceral pericardium (see Constrictive-Effusive Pericarditis). Acute and subacute forms of pericarditis (which may or may not be symptomatic) may deposit fibrin, which, in turn, can evoke a pericardial effusion. This often leads to pericardial inflammation, chronic fibrotic scarring, calcification, and restricted cardiac filling. [2]
Constrictive pericarditis symptoms overlap those of diseases as diverse as myocardial infarction (MI), aortic dissection, pneumonia, influenza, and connective tissue disorders. This overlap can confuse the most skilled diagnostician. An increased suspicion of constriction helps move constrictive pericarditis to the top of a lengthy differential diagnosis list and facilitates correct diagnosis and timely therapy.
The classic diagnostic conundrum associated with constrictive pericarditis is the difficulty distinguishing this condition from restrictive cardiomyopathy (see Restrictive Cardiomyopathy) and other syndromes associated with elevated right-sided pressure that all share similar symptoms, physical findings, and hemodynamics.
Although obtaining a careful history and performing a physical examination remain the cornerstones of evaluation, technologic advances have facilitated diagnosis, particularly with the appropriate use of Doppler echocardiography, high-resolution computed tomography (CT), magnetic resonance imaging (MRI), and invasive hemodynamic measurement.
Pericardiectomy is the predominant definitive treatment. Hemodynamic and symptomatic improvements are rapid. Medical management, such as careful observation or symptomatic treatment, has been suggested in less severe cases; however, this option is controversial. The underlying disease usually determines the prognosis. Poorer prognoses are associated with malignancy and New York Heart Association (NYHA) class III or IV heart failure symptoms.
Pathophysiology
The normal pericardium is composed of 2 layers: the tough fibrous parietal pericardium and the smooth visceral pericardium. Usually, approximately 50 mL of fluid (plasma ultrafiltrate) is present in the intrapericardial space to minimize friction during cardiac motion. [3]
Acute and subacute forms of pericarditis (which may or may not be symptomatic) may deposit fibrin, which, in turn, can evoke a pericardial effusion. This often leads to pericardial organization, chronic fibrotic scarring, and calcification, most often involving the parietal pericardium (see Constrictive-Effusive Pericarditis for visceral pericardial disease). [4]
In constrictive pericarditis, the easily distensible, thin parietal and visceral pericardial linings become inflamed, thickened, and fused. Because of these changes, the potential space between the linings is obliterated, and the ventricle loses distensibility. Venous return to the heart becomes limited, and ventricular filling is reduced, with associated inability to maintain adequate preload. Filling pressures of the heart tend to become equal in both the ventricles and the atria.
Since the myocardium is unaffected, early ventricular filling during the first third of diastole is unimpeded. After early diastole, the stiff pericardium affects flow and hemodynamics. Accordingly, the ventricular pressure initially decreases rapidly (producing a steep y descent on right atrial pressure waveform tracings) and then increases abruptly to a level that is sustained until systole (the “dip-and-plateau waveform” or “square root sign” seen on right or left ventricular pressure waveform tracings). [5]
The preservation of myocardial function in early diastole aids in distinguishing constrictive pericarditis from restrictive cardiomyopathy. Systolic function is rarely affected until late in the course of the disease, presumably secondary to infiltrative processes that affect the myocardium, atrophy, or scarring or fibrosis of the myocardium from the overlying adjacent pericardial disease.
Experimental models indicated that a change in volume-elasticity curves (see the image below) was the fundamental pathophysiologic change associated with the disease. During development of the constriction, right and left ventricular diastolic pressure increased, and stroke volume decreased. A small increase in volume resulted in a considerable increase in end-diastolic pressure.
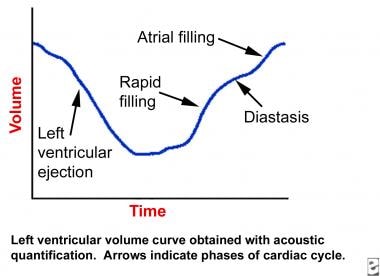 Constrictive Pericarditis. The image depicts a left ventricular volume curve in constrictive pericarditis.
Constrictive Pericarditis. The image depicts a left ventricular volume curve in constrictive pericarditis.
Symptoms consistent with congestive heart failure (CHF), especially right-sided heart failure, develop as a result of the inability of the heart to increase stroke volume. [6] Over time, cardiac output gradually becomes inadequate (see the Cardiac Output calculator), at first with exercise and then at rest.
The clinical symptoms and classic hemodynamic findings of constrictive pericarditis can be explained by the early rapid diastolic filling and elevation, with eventual equalization of the diastolic pressures in all of the cardiac chambers. This restricts late diastolic filling, leading to venous engorgement and decreased cardiac output, all secondary to a confining pericardium.
Etiology
Chronic constrictive pericarditis is a disease that has multiple possible causes and is associated with variable clinical findings, depending on its severity. It develops insidiously, and in many cases, no etiology is ever determined. In some patients (approximately 10%), an antecedent acute pericarditis is present. Other cases of constriction are postulated to have been preceded by a subclinical, or occult, form of pericarditis.
All forms of pericarditis may eventually lead to pericardial constriction. They may be broadly classified into common, less common, and rare forms. The top 3 causes of constrictive pericarditis are idiopathic (presumably viral), cardiothoracic surgery, and radiation therapy, which, according to one study, are responsible for 46%, 37%, and 9% of cases of constrictive pericarditis, respectively (in patients who underwent surgical therapy of their constriction). [7]
Common forms
Idiopathic
In many cases, particularly in developed countries, no antecedent diagnosis can be found. These cases are termed idiopathic. Reports by many authors indicate that a high percentage of idiopathic cases of constrictive pericarditis may be related to previously recognized or unrecognized viral pericarditis (see below).
Infection (bacterial and viral)
Tuberculosis is the leading cause of constrictive pericarditis in developing nations but represents only a minority of causes in the United States and other developed countries.
Bacterial infections that lead to purulent pericarditis are also declining in frequency. In the past, purulent pericarditis associated with pneumococcal pneumonia was the most common presentation of a bacterial source. However, the widespread use of antibiotics has drastically changed the frequency and spectrum of purulent pericarditis such that the most common presentation now occurs following cardiac surgery. It should be noted that the progression from acute pericarditis to constrictive pericarditis can occur more rapidly after bacterial pericarditis (eg, ≤6 months in some cases).
An increasing number of gram-positive organisms, including multiple resistant strains of staphylococci, may be isolated. Group A and B streptococci and gram-negative rods (eg, Pseudomonas species, Escherichia coli, and Klebsiella species) have also been documented.
Although the absolute number of tuberculous and bacterial pericarditis cases are decreasing, it must be recognized that these processes remain closely associated with constrictive pericarditis. A prospective analysis determined that the incidence of constrictive pericarditis was 0.76 cases per 1,000 person-years after acute idiopathic/viral pericarditis but 31.7 cases per 1,000 person-years for acute tuberculous pericarditis and 52.7 cases per 1,000 person-years for purulent pericarditis. [8]
Viral pathogens that can cause constrictive pericarditis include coxsackievirus, hepatitis, adenovirus, and echovirus. [9]
Radiation
The long-term effects of thoracic and mediastinal radiation therapy (as used in the treatment of hematologic, breast, and other malignancies) are increasingly being realized. The common features of radiation-induced cardiac complications stem from microcirculation injury with endothelial damage, capillary rupture, and platelet adhesion. This sets up an inflammatory response, which may either resolve or organize to form adhesions between the visceral pericardium and the parietal pericardium. This cascade potentially leads to constriction.
Generally, radiation-induced constrictive pericarditis presents 5-10 years after radiation therapy and is more likely to present with an associated pericardial effusion. In a study by Bertog, the median time between radiation and pericardiectomy was 11 years, with a broad range of 2-30 years. These findings were consistent with those of other previous studies. [7]
Cardiac surgery
Any operative or invasive procedure in which the pericardium is opened, manipulated, or damaged may invoke an inflammatory response, leading to constrictive pericarditis (postpericardiotomy syndrome). The most common example is constrictive pericarditis in the setting of previous coronary artery bypass grafting (CABG) when only part of the pericardium is resected.
Less common forms
Infection (fungal)
Fungal infections are an uncommon source of constrictive pericarditis in patients who are immunocompetent. Nocardia species can be causative organisms, especially in endemic areas such as the Ohio Valley. Aspergillus, Candida, and Coccidioides species are important pathogens in patients infected with HIV and in other immunocompromised hosts.
Neoplasms
Malignant involvement may also manifest as pericardial effusion (with or without tamponade) or as an encased heart with thickening of both visceral and parietal layers, resulting in constrictive physiology. Although many types of neoplasms have been reported, breast and lung carcinomas and lymphomas are the metastatic malignancies most commonly associated with constrictive pericarditis. Other malignancies that involve the pericardium with relative frequency include melanoma and mesothelioma.
Uremia
Uremia with long-term hemodialysis can lead to constrictive pericarditis and is usually associated with a pericardial effusion.
Connective tissue disorders
Autoimmune disorders that involve the pericardium are not unusual, typically manifesting as a small pericardial effusion or as an episode of acute pericarditis. Chronic pericardial involvement is less common but can occur in patients with rheumatoid arthritis, usually associated with the presence of subcutaneous nodules. Systemic lupus erythematosus (SLE) and scleroderma also may lead to constrictive pericarditis; in the latter case, the prognosis is poor.
Drugs
Procainamide and hydralazine have been reported to cause constrictive pericarditis through a drug-induced lupuslike syndrome. Methysergide therapy also has been implicated as a cause of constrictive pericarditis.
Trauma
Blunt and penetrating injuries to the chest wall have been reported to cause constrictive pericarditis, presumably through an inflammatory mechanism. Trauma-induced constrictive pericarditis is generally uncommon.
Myocardial infarction
Post-MI constrictive pericarditis has been reported. The patient typically has a history of Dressler syndrome or hemopericardium after thrombolytic therapy.
Rare forms
Constrictive pericarditis after implantation of an epicardial pacemaker or automated implantable cardiac defibrillator is a rare but reported phenomenon.
Mulibrey nanism is an autosomal recessive disorder characterized by multiple abnormalities, including dwarfism, constrictive pericarditis, abnormal fundi, and fibrous dysplasia of the long bones.
In rare instances, constrictive pericarditis may occur after sclerotherapy for esophageal varices.
Chylopericardium is a rare cause of constrictive pericarditis.
Epidemiology
As with many diseases that once were predominantly infectious in origin, the clinical spectrum of constrictive pericarditis has changed. Approximately 9% of patients with acute pericarditis from any cause go on to develop constrictive physiology. [9] The true frequency is dependent on the incidence of the specific causes of pericarditis, but given that acute pericarditis is clinically diagnosed in only 1 in 1000 hospital admissions, the frequency of a diagnosis of constrictive pericarditis is likely to be less than 1 in 10,000 admissions.
In a 2019 report of annual trends of patients admitted to US hospitals with constrictive pericarditis from 2005 to 2014, investigators found a stable prevalence of 9-10 cases per million. [10]
In the developing world, infectious etiologies remain more prominent (tuberculosis has the highest total incidence).
Age-, sex-, and race-related demographics
Although pediatric data are lacking for epidemiologic analysis, it is clear that the condition is rare in adults and even more rare in children. In all age groups, prevalence is increased among patients who are hospitalized and among patients who have undergone cardiac surgery. Cases have been reported in persons aged 8-70 years. Predilection is likely reflective of the underlying disease. Historical studies suggest a median age of 45 years, whereas more recent studies suggest a median age of 61 years (possibly reflecting ongoing demographic changes).
There appears to be a male predominance, with some studies report a male-to-female ratio of 3:1. No racial predilection exists for this disorder.
Between 2005 and 2014, patients with constrictive pericarditis who underwent pericardiectomy were younger, more likely to be male, and had fewer comorbidities than those who received medical management. [10]
Prognosis
Because constrictive pericarditis is rare, prognostic data are relatively scant. It is a potentially curable disease if diagnosed early, but it is potentially fatal if overlooked. Undiagnosed patients can have a 90% mortality. [1]
The prognosis is also dependent on the disease severity. [1] One study showed postpericardiectomy survival rates of 71% and 52% at 5 and 10 years, respectively. The long-term prognosis with medical therapy alone is poor. Life expectancy is reduced in untreated children and in patients with relatively acute onset of symptoms.
Prognostic factors that affect outcome
Better outcomes in constrictive pericarditis is associated with an increased medial mitral annulus early diastolic velocity (e'). [11]
Separately, in a 2021 study that analyzed the preoperative model for end-stage liver disease (MELD) (n = 175) and MELD-XI (exclude international normalized ratio) score (n = 226) as predictors of outcomes in patients undergoing pericardiectomy for constrictive pericarditis, investigators found an 8.7% 90-day mortality, with higher MELD and MELD-XI scores associated with higher postoperative morbidity and mortality. [12] Both scores were also associated with an increased incidence of renal failure and higher levels of chest-tube intubation and transfusion. In addition, MELD-XI score was associated with prolonged intubated and longer intensive care unit and hospital stays. [12]
Mortality
Between 2005 and 2014, in-hospital mortality for patients with constrictive pericarditis was 7.3% for those who underwent pericardiectomy and 6.8% for those who received medical management. [10]
Long-term survival after pericardiectomy depends on the underlying cause. [1] Of common causes, idiopathic constrictive pericarditis has the best prognosis (88% survival at 7 years), followed by constriction due to cardiac surgery (66% at 7 years). The worst postpericardiectomy prognosis occurs in postradiation constrictive pericarditis (27% survival at 7 years), probably as a reflection of confounding comorbidities. Occasionally, the etiology of the constriction may cause coincident myocardial dysfunction.
With surgical treatment, the long-term outcomes of patients with constrictive pericarditis have been shown to be independently less favorable with advanced age, poor renal function, abnormal left ventricular systolic function, high pulmonary artery systolic pressure, lower serum sodium level, worsening NYHA classification, and, as noted above, radiation therapy as the cause of the constrictive pericarditis. [7, 13] The degree of pericardial calcification has shown no effect on survival.
Morbidity
Failure of conventional medical therapy for heart failure often follows an extensive diagnostic workup, leading to the final diagnosis of constrictive pericarditis. Decline in function is a result of decreased cardiac output (see the Cardiac Output calculator) with symptoms of heart failure, along with morbidity stemming from chronic systemic venous congestion.
Multisystem failure can develop into an end-stage of illness when global tissue hypoxia leads to worsening metabolic acidemia.
-
Constrictive Pericarditis. These images are anteroposterior and lateral chest radiographs from a patient with tuberculous constrictive pericarditis (arrows denote marked pericardial calcification).
-
Constrictive Pericarditis. This right atrial pressure tracing shows marked y descents (arrows) in a patient with constrictive pericarditis.
-
Constrictive Pericarditis. The simultaneous right and left ventricular pressure tracings shows diastolic equalization of pressures in both ventricles in a patient with constrictive pericarditis.
-
Constrictive Pericarditis. The magnetic resonance image shows constrictive pericarditis in 13-year-old patient with an otherwise structurally normal heart. Infectious workup was negative. (Image courtesy of Tal Geva, MD.)
-
Constrictive Pericarditis. The image depicts a left ventricular volume curve in constrictive pericarditis.





