Background
Peptic ulcer disease can involve the stomach or duodenum. Gastric and duodenal ulcers usually cannot be differentiated based on history alone, although some findings may be suggestive (see DDx). Epigastric pain is the most common symptom of both gastric and duodenal ulcers, characterized by a gnawing or burning sensation and that occurs after meals—classically, shortly after meals with gastric ulcers and 2-3 hours afterward with duodenal ulcers.
In uncomplicated peptic ulcer disease, the clinical findings are few and nonspecific. “Alarm features" that warrant prompt gastroenterology referral [1] include bleeding, anemia, early satiety, unexplained weight loss, progressive dysphagia or odynophagia, recurrent vomiting, and a family history of gastrointestinal (GI) cancer. Patients with perforated peptic ulcer disease usually present with a sudden onset of severe, sharp abdominal pain. (See Presentation.)
In most patients with uncomplicated peptic ulcer disease, routine laboratory tests usually are not helpful; instead, documentation of peptic ulcer disease depends on radiographic and endoscopic confirmation. Testing for H pylori infection is essential in all patients with peptic ulcers. Rapid urease tests are considered the endoscopic diagnostic test of choice. Of the noninvasive tests, fecal antigen testing is more accurate than antibody testing and is less expensive than urea breath tests but either is reasonable. A fasting serum gastrin level should be obtained in certain cases to screen for Zollinger-Ellison syndrome. (See Workup.)
Upper GI endoscopy is the preferred diagnostic test in the evaluation of patients with suspected peptic ulcer disease. Endoscopy provides an opportunity to visualize the ulcer, to determine the presence and degree of active bleeding, and to attempt hemostasis by direct measures, if required. Perform endoscopy early in patients older than 45-50 years and in patients with associated so-called alarm features.
Most patients with peptic ulcer disease are treated successfully with cure of H pylori infection and/or avoidance of nonsteroidal anti-inflammatory drugs (NSAIDs), along with the appropriate use of antisecretory therapy. In the United States, the recommended primary therapy for H pylori infection is proton pump inhibitor (PPI)–based triple therapy. [1] These regimens result in a cure of infection and ulcer healing in approximately 85-90% of cases. [2] Ulcers can recur in the absence of successful H pylori eradication. (See Treatment.)
In patients with NSAID-associated peptic ulcers, discontinuation of NSAIDs is paramount, if it is clinically feasible. For patients who must continue with their NSAIDs, proton pump inhibitor (PPI) maintenance is recommended to prevent recurrences even after eradication of H pylori. [3, 4] Prophylactic regimens that have been shown to dramatically reduce the risk of NSAID-induced gastric and duodenal ulcers include the use of a prostaglandin analog or a PPI. Maintenance therapy with antisecretory medications (eg, H2 blockers, PPIs) for 1 year is indicated in high-risk patients. (See Medication.)
The indications for urgent surgery include failure to achieve hemostasis endoscopically, recurrent bleeding despite endoscopic attempts at achieving hemostasis (many advocate surgery after two failed endoscopic attempts), and perforation.
Patients with gastric ulcers are also at risk of developing gastric malignancy.
Anatomy
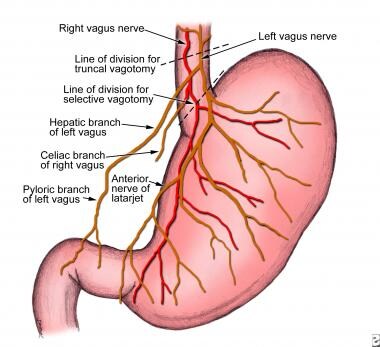
Because many surgical procedures for peptic ulcer disease entail some type of vagotomy, a discussion concerning the vagal innervation of the abdominal viscera is appropriate (see image below). The left (anterior) and the right (posterior) branches of the vagus nerve descend along either side of the distal esophagus. As they enter the lower thoracic cavity, they can communicate with each other through several cross-branches that comprise the esophageal plexus. However, below this plexus, the two vagal trunks again become separate and distinct before the anterior trunk branches to form the hepatic, pyloric, and anterior gastric (also termed the anterior nerve of Latarjet) branches. The posterior trunk branches to form the posterior gastric branch (also termed the posterior nerve of Latarjet) and the celiac branch.
The parietal cell mass of the stomach is segmentally innervated by the terminal branches from each of the anterior and posterior gastric branches. These terminal branches are divided during highly selective vagotomy. The gallbladder is innervated from efferent branches of the hepatic division of the anterior trunk. Consequently, transection of the anterior vagus trunk (performed during truncal vagotomy) can result in a dilated gallbladder with inhibited contractility and subsequent cholelithiasis. The celiac branch of the posterior vagus innervates the entire midgut (with the exception of the gallbladder). Thus, division of the posterior trunk during truncal vagotomy may contribute to postoperative ileus.
Pathophysiology
Peptic ulcers are defects in the gastric or duodenal mucosa that extend through the muscularis mucosa. The epithelial cells of the stomach and duodenum secrete mucus in response to irritation of the epithelial lining and as a result of cholinergic stimulation. The superficial portion of the gastric and duodenal mucosa exists in the form of a gel layer, which is impermeable to acid and pepsin. Other gastric and duodenal cells secrete bicarbonate, which aids in buffering acid that lies near the mucosa. Prostaglandins of the E type (PGE) have an important protective role, because PGE increases the production of both bicarbonate and the mucous layer.
In the event of acid and pepsin entering the epithelial cells, additional mechanisms are in place to reduce injury. Within the epithelial cells, ion pumps in the basolateral cell membrane help to regulate intracellular pH by removing excess hydrogen ions. Through the process of restitution, healthy cells migrate to the site of injury. Mucosal blood flow removes acid that diffuses through the injured mucosa and provides bicarbonate to the surface epithelial cells.
Under normal conditions, a physiologic balance exists between gastric acid secretion and gastroduodenal mucosal defense. Mucosal injury and, thus, peptic ulcer occur when the balance between the aggressive factors and the defensive mechanisms is disrupted. Aggressive factors, such as nonsteroidal anti-inflammatory drugs (NSAIDs), H pylori infection, alcohol, bile salts, acid, and pepsin, can alter the mucosal defense by allowing the back diffusion of hydrogen ions and subsequent epithelial cell injury. The defensive mechanisms include tight intercellular junctions, mucus, bicarbonate, mucosal blood flow, cellular restitution, and epithelial renewal.
The gram-negative spirochete H pylori was first linked to gastritis in 1983. Since then, further study of H pylori has revealed that it is a major part of the triad, which includes acid and pepsin, that contributes to primary peptic ulcer disease. The unique microbiologic characteristics of this organism, such as urease production, allows it to alkalinize its microenvironment and survive for years in the hostile acidic environment of the stomach, where it causes mucosal inflammation and, in some individuals, worsens the severity of peptic ulcer disease.
When H pylori colonizes the gastric mucosa, inflammation usually results. The causal association between H pylori gastritis and duodenal ulceration is now well established in the adult and pediatric literature. In patients infected with H pylori, high levels of gastrin and pepsinogen and reduced levels of somatostatin have been measured. In infected patients, exposure of the duodenum to acid is increased. Virulence factors produced by H pylori, including urease, catalase, vacuolating cytotoxin, and lipopolysaccharide, are well described.
Most patients with duodenal ulcers have impaired duodenal bicarbonate secretion, which has also proven to be caused by H pylori because its eradication reverses the defect. [5] The combination of increased gastric acid secretion and reduced duodenal bicarbonate secretion lowers the pH in the duodenum, which promotes the development of gastric metaplasia (ie, the presence of gastric epithelium in the first portion of the duodenum). H pylori infection in areas of gastric metaplasia induces duodenitis and enhances the susceptibility to acid injury, thereby predisposing to duodenal ulcers. Duodenal colonization by H pylori was found to be a highly significant predictor of subsequent development of duodenal ulcers in one study that followed 181 patients with endoscopy-negative, nonulcer dyspepsia. [6]
Etiology
Peptic ulcer disease may be due to any of the following:
-
H pylori infection
-
Drugs
-
Lifestyle factors
-
Severe physiologic stress
-
Hypersecretory states (uncommon)
-
Genetic factors
H pylori infection
H pylori infection and nonsteroidal anti-inflammatory drug (NSAID) use account for most cases of peptic ulcer disease. The rate of H pylori infection for duodenal ulcers in the United States is less than 75% for patients who do not use NSAIDs. Excluding patients who used NSAIDs, 61% of duodenal ulcers and 63% of gastric ulcers were positive for H pylori in one study. These rates were lower in whites than in nonwhites. Prevalence of H pylori infection in complicated ulcers (ie, bleeding, perforation) is significantly lower than that found in uncomplicated ulcer disease.
Drugs
NSAID use is a common cause of peptic ulcer disease. These drugs disrupt the mucosal permeability barrier, rendering the mucosa vulnerable to injury. As many as 30% of adults taking NSAIDs have GI adverse effects. Factors associated with an increased risk of duodenal ulcers in the setting of NSAID use include history of previous peptic ulcer disease, older age, female sex, high doses or combinations of NSAIDs, long-term NSAID use, concomitant use of anticoagulants, and severe comorbid illnesses.
A long-term prospective study found that patients with arthritis who were older than 65 years who regularly took low-dose aspirin were at an increased risk for dyspepsia severe enough to necessitate the discontinuation of NSAIDs. [7] This suggests that better management of NSAID use should be discussed with older patients in order to reduce NSAID-associated upper GI events.
A UK retrospective study of patients newly initiated on low-dose aspirin for secondary prevention of cardiovascular events identified risk factors for uncomplicated peptic ulcer disease in these patients that included the following [8] :
-
Previous history of peptic ulcer disease
-
Current use of NSAIDs, oral steroid agents, or acid suppressive agents
-
Tobacco use
-
Stress
-
Depression
-
Anemia
-
Social deprivation (comprises four census variables used in the Townsend deprivation index [9] : households that lack a car, are overcrowded, not owner-occupied, and have unemployed persons)
Although the idea was initially controversial, most evidence now supports the assertion that H pylori and NSAIDs are synergistic with respect to the development of peptic ulcer disease. A meta-analysis found that H pylori eradication in NSAID-naive users before the initiation of NSAIDs was associated with a decrease in peptic ulcers. [10]
Although the prevalence of NSAID gastropathy in children is unknown, it seems to be increasing, especially in children with chronic arthritis treated with NSAIDs. Case reports have demonstrated gastric ulceration from low-dose ibuprofen in children, even after just 1 or 2 doses. [11]
Corticosteroids alone do not increase the risk for peptic ulcer disease; however, they can potentiate ulcer risk in patients who use NSAIDs concurrently.
The risk of upper GI tract bleeding may be increased in users of the diuretic spironolactone [12] or serotonin reuptake inhibitors with moderate to high affinity for serotonin transporter. [13]
Lifestyle factors
Evidence that tobacco use is a risk factor for duodenal ulcers is not conclusive. Support for a pathogenic role for smoking comes from the finding that smoking may accelerate gastric emptying and decrease pancreatic bicarbonate production. However, studies have produced contradictory findings. In one prospective study of more than 47,000 men with duodenal ulcers, smoking did not emerge as a risk factor. [14] However, smoking in the setting of H pylori infection may increase the risk of relapse of peptic ulcer disease. [15] Smoking is harmful to the gastroduodenal mucosa, and H pylori infiltration is denser in the gastric antrum of smokers. [16]
Ethanol is known to cause gastric mucosal irritation and nonspecific gastritis. Evidence that consumption of alcohol is a risk factor for duodenal ulcer is inconclusive. A prospective study of more than 47,000 men with duodenal ulcer did not find an association between alcohol intake and duodenal ulcer. [14]
Little evidence suggests that caffeine intake is associated with an increased risk of duodenal ulcers.
Severe physiologic stress
Stressful conditions that may cause peptic ulcer disease include burns, central nervous system (CNS) trauma, surgery, and severe medical illness. Serious systemic illness, sepsis, hypotension, respiratory failure, and multiple traumatic injuries increase the risk for secondary (stress) ulceration.
Cushing ulcers are associated with a brain tumor or injury and typically are single, deep ulcers that are prone to perforation. They are associated with high gastric acid output and are located in the duodenum or stomach. Extensive burns are associated with Curling ulcers.
Stress ulceration and upper-gastrointestinal (GI) hemorrhage are complications that are increasingly encountered in critically ill children in the intensive care setting. Severe illness and a decreased gastric pH are related to an increased risk of gastric ulceration and hemorrhage.
Hypersecretory states (uncommon)
The following are among hypersecretory states that may, uncommonly, cause peptic ulcer disease:
-
Gastrinoma (Zollinger-Ellison syndrome) or multiple endocrine neoplasia type I (MEN-I)
-
Antral G cell hyperplasia
-
Systemic mastocytosis
-
Basophilic leukemias
-
Cystic fibrosis
-
Short bowel syndrome
-
Hyperparathyroidism
Physiologic factors
In up to one third of patients with duodenal ulcers, basal acid output (BAO) and maximal acid output (MAO) are increased. In one study, increased BAO was associated with an odds ratio [OR] of up to 3.5, and increased MAO was associated with an OR of up to 7 for the development of duodenal ulcers. Individuals at especially high risk are those with a BAO greater than 15 mEq/h. The increased BAO may reflect the fact that in a significant proportion of patients with duodenal ulcers, the parietal cell mass is increased to nearly twice that of the reference range. [17]
In addition to the increased gastric and duodenal acidity observed in some patients with duodenal ulcers, accelerated gastric emptying is often present. This acceleration leads to a high acid load delivered to the first part of the duodenum, where 95% of all duodenal ulcers are located. Acidification of the duodenum leads to gastric metaplasia, which indicates replacement of duodenal villous cells with cells that share morphologic and secretory characteristics of the gastric epithelium. Gastric metaplasia may create an environment that is well suited to colonization by H pylori.
Seasonal changes and climate extremes may also affect gastric mucosa and cause damage to the gastric mucosa and its barrier function. [18] In extreme cold climate, Yuan et al noted significantly lower expression of heat shock protein 70 (HSP70) as well as decreased mucosal thickness in the gastric antrum of patients with peptic ulcer disease who were at high risk of bleeding compared to those at low risk of bleeding.
Moreover, compared to extreme hot climate, extreme cold climate was associated with significantly lower levels of occludin, HSP70, nitric oxide synthase (NOS), and epidermal growth factor receptor (EGFR), but no statistically significant differences in these protein expression levels were found between patients at high and low risk of bleeding. [18] The investigators also did not note any significant differences found in the rates of H pylori infection and pH levels of gastric juices between patients at high bleeding risk and those at low bleeding risk. [18]
Genetics
More than 20% of patients have a family history of duodenal ulcers, compared with only 5-10% in the control groups. In addition, weak associations have been observed between duodenal ulcers and blood type O. Furthermore, patients who do not secrete ABO antigens in their saliva and gastric juices are known to be at higher risk. The reason for these apparent genetic associations is unclear.
A rare genetic association exists between familial hyperpepsinogenemia type I (a genetic phenotype leading to enhanced secretion of pepsin) and duodenal ulcers. However, H pylori can increase pepsin secretion, and a retrospective analysis of the sera of one family studied before the discovery of H pylori revealed that their high pepsin levels were more likely related to H pylori infection.
Additional etiologic factors
Any of the following may be associated with peptic ulcer disease:
-
Allergic gastritis and eosinophilic gastritis
-
Cytomegalovirus infection
-
Uremic gastropathy
-
Henoch-Schönlein gastritis
-
Corrosive gastropathy
-
Bile gastropathy
-
Autoimmune disease
-
Other granulomatous gastritides (eg, sarcoidosis, histiocytosis X, tuberculosis)
-
Phlegmonous gastritis and emphysematous gastritis
-
Other infections, including Epstein-Barr virus, HIV, Helicobacter heilmannii, herpes simplex, influenza, syphilis, Candida albicans, histoplasmosis, mucormycosis, and anisakiasis
-
Chemotherapeutic agents, such as 5-fluorouracil (5-FU), methotrexate (MTX), and cyclophosphamide
-
Local radiation resulting in mucosal damage, which may lead to the development of duodenal ulcers
-
Use of crack cocaine, which causes localized vasoconstriction, resulting in reduced blood flow and possibly leading to mucosal damage
Epidemiology
The global incidence and prevalence of peptic ulcer disease, along with the associated rates of hospitalizations and mortality, have been in decline over the past couple of decades, attributed in part to the complex changes in the risk factors for peptic ulcer disease, including reductions in the prevalence of H pylori infection, the widespread use of antisecretory agents and nonsteroidal anti-inflammatory drugs (NSAIDs), and an aging population. [19]
United States statistics
In the United States, peptic ulcer disease affects approximately 4.6 million people annually, with an estimated 10% of the US population having evidence of a duodenal ulcer at some time. [20] H pylori infection accounts for 90% of duodenal ulcers and 70%-90% of gastric ulcers. [21] The proportion of people with H pylori infection and peptic ulcer disease increases steadily with age.
Overall, the incidence of duodenal ulcers has been decreasing over the past 3-4 decades. Although the rate of simple gastric ulcer is in decline, the incidence of complicated gastric ulcer and hospitalization has remained stable, partly due to the concomitant use of aspirin in an aging population.
The prevalence of peptic ulcer disease has shifted from predominance in males to similar occurrences in males and females. The lifetime prevalence is approximately 11%-14% in men and 8-11% in women. [20] Age trends for ulcer occurrence reveal declining rates in younger men, particularly for duodenal ulcer, and increasing rates in older women.
In a systematic search of PubMed, EMBASE, and the Cochrane library, the annual incidence rates of peptic ulcer disease were found to be 0.10-0.19% for physician-diagnosed peptic ulcer disease and 0.03-0.17% when based on hospitalization data. [22] The 1-year prevalence based on physician diagnosis was 0.12-1.50% and that based on hospitalization data was 0.10-0.19%. The majority of studies reported a decrease in the incidence or prevalence of peptic ulcer disease over time. [22]
International statistics
The frequency of peptic ulcer disease in other countries is variable and is determined primarily by association with the major causes of peptic ulcer disease: H pylori and NSAIDs. [23] A 2018 systematic MEDLINE and PubMed review found Spain had the highest annual incidence of all peptic ulcer disease (141.8/100,000 persons), whereas the United Kingdom had the lowest (23.9/100,000 persons). [24] When perforated peptic ulcer disease was assessed, South Korea had the highest annual incidence (4.4/100,000 persons) and the United Kingdom, again, had the lowest (2.2/100,000 persons). [24]
Prognosis
When the underlying cause of peptic ulcer disease is addressed, the prognosis is excellent. Most patients are treated successfully with the eradication of H pylori infection, avoidance of nonsteroidal anti-inflammatory agents (NSAIDs), and the appropriate use of antisecretory therapy. Eradication of H pylori infection changes the natural history of the disease, with a decrease in the ulcer recurrence rate from 60% to 90% to approximately 10% to 20%. However, this is a higher recurrence rate than previously reported, suggesting an increased number of ulcers not caused by H pylori infection.
With regard to NSAID-related ulcers, the incidence of perforation is approximately 0.3% per patient year, and the incidence of obstruction is approximately 0.1% per patient year. Combining both duodenal ulcers and gastric ulcers, the rate of any complication in all age groups combined is approximately 1-2% per ulcer per year.
The mortality rate for peptic ulcer disease, which has decreased modestly in the last few decades, is approximately 1 death per 100,000 cases. If one considers all patients with duodenal ulcers, the mortality rate due to ulcer hemorrhage is approximately 5%. [20] Over the last 20 years, the mortality rate in the setting of ulcer hemorrhage has not changed appreciably despite the advent of histamine-2 receptor antagonists (H2RAs) and proton pump inhibitors (PPIs). However, evidence from meta-analyses and other studies has shown a decreased mortality rate from bleeding peptic ulcers when intravenous PPIs are used after successful endoscopic therapy. [25, 26, 27, 28]
Emergency operations for peptic ulcer perforation carry a mortality risk of 6-30%. [29, 30] Factors associated with higher mortality in this setting include the following:
-
Shock at the time of admission
-
Renal insufficiency
-
Delaying the initiation of surgery for more than 12 hours after presentation
-
Concurrent medical illness (eg, cardiovascular disease, diabetes mellitus)
-
Age older than 70 years
-
Cirrhosis
-
Immunocompromised state
-
Location of ulcer (mortality associated with perforated gastric ulcer is twice that associated with perforated duodenal ulcer)
In a retrospective population-based study (2001-2014) that evaluated long-term mortality in 234 patients who underwent surgery for perforated peptic ulcer, mortality was 15.2% at 30 days, 19.2% at 90 days, 22.6% at 1 year, and 24.8% at 2 years. [31] When the 30-day mortality data were excluded, 36% of patients died during a median follow-up of 57 months. Independent factors associated with an increased risk of long-term mortality included age older than 60 years and the presence of comorbidities such as active malignancy, hypoalbuminemia, pulmonary disease, cardiovascular disease, and severe postoperative complications during the initial stay. [31]
Patient Education
Patients with peptic ulcer disease should be warned about known or potentially injurious drugs and agents. Some examples are as follows:
-
Nonsteroidal anti-inflammatory drugs (NSAIDs)
-
Aspirin
-
Alcohol
-
Tobacco
-
Caffeine (eg, coffee, tea, colas)
Obesity has been shown to have an association with peptic ulcer disease, and patients should be counseled regarding benefits of weight loss. Stress reduction counseling might be helpful in individual cases but is not needed routinely.
For patient education resources, see Digestive Disorders Center as well as Peptic Ulcer, Heartburn, and GERD and Heartburn Medications.
-
Peptic ulcer disease. Vagal innervation of the stomach.
-
Peptic ulcer disease. Gastric ulcer with a punched-out ulcer base and whitish fibrinoid exudates.
-
Peptic ulcer disease. Gastric ulcer (lesser curvature) with a punched-out ulcer base with a whitish exudate.
-
Peptic ulcer disease. Gastric cancer. Note the irregular heaped-up overhanging margins.
-
Peptic ulcer disease. Gastric cancer with an ulcerated mass.
-
Peptic ulcer disease. Gross pathology specimen of a gastric ulcer.
-
Peptic ulcer disease. Gastric cancer with an ulcerated mass.
-
Peptic ulcer disease. Endoscopic view of an ulcer (at the upper center) in the wall of the duodenum, the first part of the small intestine. This ulcer is an open sore. Image courtesy of Science Source | Gastrolab.
-
Peptic ulcer disease. Duodenal ulcer in a 65-year-old man with osteoarthritis who presented with hematemesis and melena. The patient took naproxen on a daily basis.