Practice Essentials
In 1630 a Dutch physician, Jacobus Bonitus, observed in Java, "a very troublesome affliction, ...called by the inhabitants Beri-beri (which means sheep), those, whom this same disease attacks, with their knees shaking and the legs raised up, walk like sheep."
In the last 100 years, the cause of beriberi was determined to be deficiency of thiamine (vitamin B1), a water-soluble and heat-labile vitamin required for carbohydrate metabolism. [1] Thiamine is essential for most vertebrates and some microorganisms. Beriberi has 2 main forms in humans, depending on the system of maximum involvement. Wet (edematous) beriberi is a cardiovascular dysfunction that is usually chronic but may have an acute presentation. Dry beriberi is a multifocal peripheral and/or central neurologic dysfunction, which includes Wernicke encephalopathy and Korsakoff syndrome. Often times, patients present with involvement of both systems.
How a single vitamin deficiency can have such diverse patterns of presentation is not fully understood, but genetic differences in the 3 enzymes that use thiamine are likely to play a large role. Other potential explanations include the coexistence of other vitamin or dietary deficiencies; simultaneous comorbidities, stressors, or both; and variations in tissue stores or turnover of the vitamin. During an Israeli outbreak of beriberi in late 2003, 600-1000 infants consumed a thiamine-deficient formula, yet only a small number manifested clinical manifestations.
Although the thresholds and prevalence varies in both developed and underdeveloped countries, beriberi is presently found in situations outside of the normal protective measures of modern society. Also, unusual physiologic conditions in which beriberi could have been predicted have been documented. Finally, chance circumstances in which thiamine deficiency is fully unanticipated have also been recognized. Dietary thiamine deficiency can be caused by an overall poor nutritional intake, by dietary customs that rely heavily on inadequate food sources (eg, milled rice), and, rarely, by consuming foods that contain thiaminases or antithiamine compounds. [2]
Because its husk is an important source of thiamine, changes in rice processing may contribute to a higher rate of thiamine deficiency unless this risk factor is recognized. A cohort at particularly high risk are alcoholics who have poor nutrition and because alcohol also impairs thiamine absorption. A newly appreciated cohort of individuals with thiamine deficiency are patients who have had bariatric surgery. [3]
In 1998, the Institute of Medicine of the National Academies published the recommended dietary intake of thiamine and other B vitamins for males and females (from infants to the elderly). [4] Also, a comprehensive monograph on beriberi was commissioned by the World Health Organization; it recommends that the term beriberi be replaced by thiamine deficiency. [5]
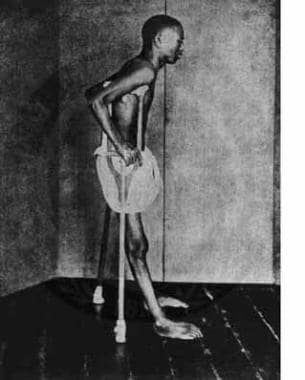
For more information regarding the cardiovascular and neurologic manifestations encountered in adult patients, see the Medscape Reference article Beriberi (Thiamine Deficiency). See the image below.
Pathophysiology
Beriberi is caused by thiamine deficiency, which can be the result of different physiologic, dietary, and environmental factors. Frequently, more than one risk factor is present.
Thiamine mainly functions as thiamine pyrophosphate (TPP), which serves as a prosthetic group or cofactor for three enzymes essential to carbohydrate and energy metabolism. These enzymes all use thiamine's thiazole ring to activate and transfer a 2-carbon unit (aldehyde). The products of these reactions all provide precursors for other synthetic pathways and also provide substrates that yield energy for the cell. Thus, deficiency can lead to interruption in production of energy that is needed to maintain function in various tissues. The three enzymes that employ TPP as a cofactor are pyruvate dehydrogenase, which catalyzes decarboxylation of pyruvate to acetyl co; alpha ketoglutarate dehydrogenase, which catalyzes the decarboxylation of ketoglutarate; and the transketolation reaction in the pentose phosphate pathway.
Pyruvate dehydrogenase is the last step in the catabolism of glucose for energy, glycolysis, and yields acetyl CoA, which enters into the Krebs cycle. Acetyl Co-A is also used to synthesize acetylcholine, an important neurotransmitter. Alpha ketoglutarate dehydrogenase is another essential part of the Krebs cycle, which yields greater amounts of ATP (energy) and additional neurotransmitters (GABA and glutamate). Transketolase activity is an essential step in the hexose monophosphate shunt. This cycle generates nicotinamide adenine dinucleotide phosphate (NADPH) formation that is required for intramitochondrial electron transport and generation of nucleic acid precursors. [6, 7]
Impaired energy production, increased manufacturing of free radicals, decreases in neurotransmitters, and possible N-methyl-D-aspartate (NMDA) receptor–mediated toxicity have been hypothesized to yield the neuronal injury seen in dry beriberi. The exact biochemical defect responsible for the clinical manifestations of cardiac (wet) beriberi or its acute form, Shoshin beriberi (from the Japanese, meaning "sudden collapse"), is not yet fully elucidated. [8] Cardiac dysfunction may simply be compromised by myocardial tissue edema and energy depletion.
Thiamine is not widely distributed in high concentrations; consequently, many foods are now routinely fortified with it. Rich natural sources include whole grains, lean pork, peas, spinach, and legumes. Very little thiamine is present in fats, oils, and refined sugars. It is destroyed by heat, pasteurization, and ionizing radiation. Freezing does not affect the bioavailability of thiamine; however, it is insoluble in alcohol. The risk of beriberi increases in individuals who consume a diet high in thiaminase rich foods (eg, raw freshwater fish or shellfish, ferns), a diet high in antithiamine factors (eg, tea, coffee, betel nuts), or both.
Deficiency of thiamine affects the cardiovascular, muscular, nervous, and GI systems. The body stores of thiamine are minimal, and the duration of thiamine reserves is unknown. In one study, deficiency was detected after approximately 6 weeks without thiamine. In another study of healthy young men who consumed less than 0.2 mg of thiamine daily, urinary excretion of thiamine stopped within 18 days. Case studies have suggested that fatal deficiency can develop in as little as 3 weeks without thiamine intake.
Despite the widespread fortification of many foods and infant formulas with thiamine, clinicians must remain aware of the signs and symptoms of beriberi, a life-threatening, but rapidly reversible, condition.
Epidemiology
United States statistics
The incidence of beriberi is unknown. Although all of the following published cohorts were not based on American patients, they could have occurred within the United States.
Although the vast majority of clinical cases are encountered in individuals with alcoholism, beriberi outbreaks have been described in other poorly nourished cohorts. East Asian immigrants who maintain their typical diet are particularly vulnerable.
Beriberi has been described in patients with GI diseases that include malnutrition, malabsorption syndromes (eg, human immunodeficiency virus [HIV] enteropathy [9] ), and hyperemesis gravidarum. [7] It has also been reported in hypermetabolic conditions such as lymphoma.
In the late 1980s, a shortage of multivitamin infusion occurred in the United States due to reduced production. [9] As a result, numerous patients dependent on total parenteral nutrition (TPN) developed beriberi, which was rapidly reversed by intravenous thiamine. Ironically, thiamine was readily available despite the multivitamin shortage.
One review cited more than 100 reports that described dry beriberi following bariatric surgery. [4] Stringent criteria summarized 84 cases that included 2 or more of the following: mental status changes, eye movement abnormalities, cerebellar dysfunction, and dietary deficiency. Gastric bypass or a restrictive procedure was performed in 80 cases (95%). Admission occurred within 6 months of surgery in 79 cases (94%). Frequent vomiting was a risk factor in 76 cases (90%) and had lasted for a median of 21 days at admission. Intravenous glucose administration without thiamine was a risk factor in 15 cases (18%). Brain MRI identified characteristic lesions in 14 cases (47%). Incomplete recovery was observed in 41 cases (49%); memory deficits and gait difficulties were frequent sequela. As suggested by the authors, surgeons, emergency room physicians, and health care providers need to be aware of the possibility of beriberi in patients who have experienced prolonged emesis after gastric bypass surgery.
In late 2003, a beriberi outbreak was seen among normal Israeli infants. [10, 11] The cause of the deficiency was a manufacturing omission of thiamine in a brand of soy-based formula exclusively marketed in Israel. Tragically, 2 of the earliest-affected infants died before the etiology was recognized. MRI findings of this cohort are summarized below. Follow-up neurodevelopment studies were conducted on 20 of these infants; learning disabilities were reported, including delayed language development compared with infants fed other sources of milk and matched for age, sex, and maternal education.
An intriguing hypothesis that has recently been published by several groups links subclinical or unrecognized thiamine deficiency to adult congestive heart failure. Diuretics were found to result in increased thiamine excretion and to predispose to a relative deficient state. In a study from Toronto, one third of adults hospitalized with congestive heart failure had thiamine deficiency, compared with 12% of controls. [12]
International statistics
The prevalence of beriberi is much higher in East Asian countries because of the consumption of milled rice. [13] Thiamine is contained in the outer coat of rice, and polishing destroys it. In the same countries, the custom of eating raw fish further increases the potential for deficiency.
Breastfed infants whose mothers have thiamine deficiency develop an infantile form of beriberi. [14]
The same socioeconomic factors that yield beriberi in the West do so with much greater prevalence in East Asia. A study done in Indonesia revealed the prevalence of thiamine deficiency among low-income families to be as high as 66%. [15] A study conducted in a group of Karen women from a refugee camp on the Thailand-Burma border revealed that up to 58% of these women were thiamine deficient 3 months postpartum, despite what appeared to be adequate dietary thiamine supplements. [16]
A study in Cambodia reported that 27% of reproductive-age women and 15% of children aged 6 months to 5 years had thiamine deficiency; the highest prevalence of deficiency (38%) was among infants aged 6-12 months. In Myanmar, a survey showed that beriberi was the second leading cause of death among infants and children aged younger than 5 years. [13]
Outbreaks have been described in prisons, [17] drug rehabilitation centers, [18] rural, agrarian communities, and in ships kept out at sea too long.
A study by Ibrahim et al in Qatar found that risk factors for thiamine deficiency among adolescents who had undergone bariatric surgery included poor oral intake (90%), nausea and vomiting (80%), and nonadherence to multivitamin supplementation (71%). [19]
A familial form of thiamine deficiency with mitochondrial myopathy has been described in Japan. [20, 21]
A report from Brazil described an outbreak of dry beriberi that lasted from 2006-2007 and included more than 1000 cases and 30 deaths. Most individuals were male laborers who were working in a region of the country where traditional agriculture was replaced to accommodate logging and mining industry. The Brazilian ministry of health points out that the previous outbreak in the country, around the turn of the century, occurred in conjunction with the expansion of the rubber industry in the Amazon. This experience suggests that when local factors disturb the established social, economic, or agricultural balance, the potential for beriberi increases, and that those with poor nutrition, especially those who also abuse alcohol, represent the most vulnerable targets.
Race-, sex-, and age-related demographics
The prevalence is highest in cultures that depend on a high proportion of their calories from foods that have poor thiamine content, such as milled rice.
Beriberi can affect both genders, although alcoholism (a major risk factor) is more prevalent in males.
Beriberi is predominantly observed in adults and infants aged 1-4 months (infantile beriberi).
Prognosis
In patients with wet beriberi, the following improvement is observed in the first 6-24 hours after thiamine administration:
-
Cyanosis disappears.
-
The heart rate reduces.
-
The respiratory rate reduces.
-
Diuresis and reduction in heart size may be apparent within 1-2 days.
In patients with dry beriberi, the complete resolution of the peripheral neurologic symptoms can take weeks to months.
In patients with Wernicke encephalopathy, the ocular symptoms resolve within hours to days, and the confusional state subsides in days to weeks.
Korsakoff syndrome resolves over months, and residual deficits are often reported.
Infantile beriberi may lead to learning deficits in childhood and beyond.
Morbidity/mortality
Mortality is rare and is usually restricted to wet beriberi (cardiac) that goes undiagnosed for too long and, hence, can not be treated. Morbidity is also rare and is usually seen in dry beriberi (neurologic) that is treated so late in the course of the illness that some residual neurologic deficits remain. In both situations, the timely recognition of the signs and symptoms of beriberi can result in thiamine replacement, which rapidly reverses the cardiovascular and neurologic dysfunction.
Complications
Complications include the following:
-
GI complaints, including constipation and colicky abdominal pain
-
Muscle wasting
-
Vision or hearing impairment
-
Complete paralysis
-
Ataxia
-
Profound loss of recent memory with active imagination
-
Delirium
-
Death
Patient Education
Population at risk must be educated regarding the diversification of diet, the incorporation of foods high in thiamine, proper food preparation (shorter cooking time for vegetables, reduction in amount of rice washing prior to cooking), the value of whole grains, avoidance of alcohol, and thiamine supplementation, if that is necessary to maintain thiamine status.
-
Beriberi.