Practice Essentials
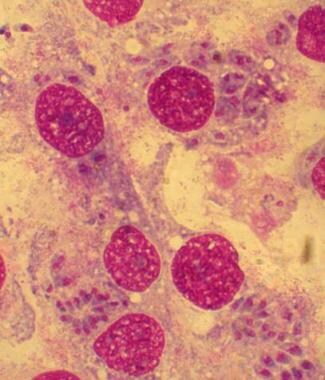
Pediatric toxoplasmosis can be acute or chronic and congenital or postnatally acquired. Toxoplasmosis refers to a symptomatic infection by Toxoplasma gondii, a widely distributed protozoan that usually causes an asymptomatic infection in the healthy host. [1] (See the image below.)
Apart from toxoplasmosis in immunocompromised individuals, congenital toxoplasmosis is the most serious manifestation of infection, resulting from the vertical transmission of T gondii transplacentally from a parasitemic mother to her offspring. The severity of disease depends on the gestational age at transmission. Ophthalmologic and neurologic disabilities are the most important consequences of infection and can be present even when the congenital infection is asymptomatic.
The fetus, newborn, and young infant with congenital toxoplasmosis are at risk of infection-associated complications, particularly retinal disease that can occur into adulthood. Hosts who are immunocompromised, especially those with defects in cellular immunity such as AIDS, are also at increased risk for severe disease.
Congenital toxoplasmosis is a preventable disease. Prepregnancy screening accompanied by serial titers and appropriate counseling in women with initial negative titers may minimize cases. [2] A study conducted in Romania, where screening for toxoplasmosis is included in the first antenatal visit, found that 29.12% of 27,169 pregnant women tested positive for IgG antibodies. Although the women with negative anti-Toxoplasma IgG antibodies (70.88%) were at risk for infection during pregnancy, only 0.9% of them returned for rescreening. [3]
Etiology
Congenital disease is passed transplacentally from the newly infected mother to the fetus during pregnancy. Other syndromes may result from newly acquired infection or reactivation of latent infection. Ingestion of meat or other foods containing cysts or oocysts present in cat feces can cause infection. Thus, individuals who live in poor sanitary conditions and those who eat raw or poorly cooked meat are at an increased risk of acquiring Toxoplasma infection. Infection can also be transmitted by blood transfusion or organ transplantation. [4]
Hosts who are immunocompromised, especially those with defects in cellular immunity such as AIDS, are also at increased risk for severe disease.
Life cycle of T gondii
T gondii is a ubiquitous obligate intracellular protozoan that infects animals and humans. It has an intestinal and an extraintestinal cycle in cats but only an extraintestinal cycle in other hosts, including herbivores, omnivores, and carnivores. T gondii exists in 3 forms: bradyzoites, tachyzoites, and sporozoites.
Bradyzoites are slowly multiplying organisms contained in tissue cysts, usually localized to muscle (skeletal and cardiac) and brain. They live in their host cells for months to years. Once ingested, gastric enzymes degrade the cyst wall, liberating viable bradyzoites.
Tachyzoites are rapidly dividing organisms found in tissues during the acute phase of infection. The tachyzoites are the forms responsible for tissue destruction. Multiplication continues until either cyst formation or host cell destruction occurs. After cell death, the free tachyzoites invade other cells and resume rapid multiplication.
Sporozoites (oocysts) result from the parasite's sexual cycle, which takes place in the epithelial cells of the cat intestine. When eliminated by the cat, these cysts must first undergo sporulation to become infectious, a process that takes 2-3 days in temperate climates and longer in cold climates. Therefore, the risk of infection is minimized if cat litter boxes are cleaned daily. Cats shed 1-100 million oocysts after the first infection, but, because of immunity, reinfection is rarely followed by reshedding of oocysts. Passive antibody transference to newborn kittens does not prevent shedding of oocysts.
Horizontal transmission
Human horizontal infection occurs from ingesting food contaminated with oocysts or poorly cooked food containing tissue cysts (bradyzoites). Although experimental attempts to transmit tachyzoites by arthropods were negative, cockroaches and flies are believed to be able to transport oocysts to water and food. Because parasitemia can persist up to a year in healthy persons, blood transfusion is a potential source of infection.
Once the individual is infected, the organism persists as tissue cysts for life. The degree of organ involvement varies considerably among patients but mostly depends on the immune status of the host. Fetuses and immunocompromised patients are most severely affected.
Vertical transmission
Vertical transmission is the cause of congenital toxoplasmosis. The infection can occur in utero or during a vaginal delivery. Transmission by breastfeeding has not been demonstrated. In general, only primary infection during pregnancy results in congenital toxoplasmosis. Thus, it is exceedingly rare for a woman to deliver a second child with congenital toxoplasmosis unless she is immunocompromised, usually from acquired immunodeficiency syndrome (AIDS). [5]
Infections that occur within 6 months prior to conception may result in transplacental transmission. Intrauterine exposure can result in an uninfected infant or infection that ranges from being asymptomatic to causing stillbirth. Approximately 30% of exposed fetuses acquire the infection, but most of the infants are asymptomatic.
The severity of infection in the fetus depends on the gestational age at the time of transmission. In general, earlier infection is more severe but less frequent. As a consequence, 85% of live infants with congenital infection appear normal at birth. Very early infections (ie, occurring in the first trimester) may result in fetal death in utero or in a newborn with severe central nervous system (CNS) involvement, such as cerebral calcifications and hydrocephalus.
Epidemiology
Occurrence in the United States
It is estimated that about 1 billion individuals worldwide are infected with T gondii. The highest rates of toxoplasmosis are in Europe, Central America, Brazil, and Central Africa.
The frequency of congenital toxoplasmosis depends on the incidence of primary infection in women of childbearing age. The earlier a woman acquires a primary infection, the less likely she is to transmit the parasite to her offspring. Prevalence increases with age. In New York, antibody prevalence was 16% in women aged 15-19 years, 27% in women aged 20-24 years, 33% in women aged 25-29 years, 40% in women aged 30-34 years, and 50% in women older than 35 years.
In addition, positive antibody titers were reported in 30% in women of childbearing age in Birmingham (1983), 12% in Chicago (1987), 14% in Massachusetts (1998), 3.3% in Denver (1986), 30% in Los Angeles (1993), 12% in Texas (1993), and 13% in New Hampshire (1998). Rates in women of childbearing age in Palo Alto, California, dropped from 27% in 1964 to 10% in 1987.
The prevalence of congenital toxoplasmosis ranges from 1 case per 1000 live births to 1 case per 10,000 live births, [6] and this prevalence can be indirectly estimated from the incidence rate of primary infection during pregnancy by multiplying the number of mothers who acquire infection during pregnancy by the transmission rate of the parasite to the fetus. On the basis of data from the National Health and Nutrition Examination Survey from 1989-1994, the incidence of primary infection for seronegative pregnant women was 0.27%. This indicates that, with 4 million births per year and an overall transmission rate of 33%, approximately 3500 infected children are born in the United States every year. [7] The rate likely varies by region.
Direct estimates of congenital infection may be derived by measuring anti-Toxoplasma immunoglobulin M (IgM) in newborn sera. However, this may underestimate the true incidence, because infants with toxoplasmosis may not have demonstrable IgM in up to 20% of cases. In Alabama, the incidence was 0.1 per 1000 births. Health care workers in Massachusetts began screening sera of newborns in 1986. From 1986-1998, a total of 99 cases were detected (incidence of 1 in 10,000 births) in Massachusetts, but at least 6 cases were missed by the screening.
International occurrence
Worldwide, the reported incidence of congenital toxoplasmosis is decreasing. The prevalence of positive antibody titers among pregnant women is often higher outside the United States. Rates of positive antibody titers internationally include the following:
-
Central African Republic - 81%
-
Tanzania - 48%
-
Zambia - 23%
-
Argentina - 53-58%
-
Austria - 36%
-
Belgium - 46%
-
Chile - 59%
-
Colombia - 60%
-
Ethiopia - More than 75%
-
France - 52%
-
Guatemala - 46%
The estimated incidence of congenital toxoplasmosis is 6 per 1000 births in France, 2 per 1000 births in Poland, 7-10 per 1000 births in Colombia, and 3 per 1000 births in Slovenia.
Age-related demographics
Incidence of T gondii antibodies increases with increasing age. The seroconversion rate in women of childbearing age is 0.8% per year. The risk of transplacental transmission is greatest during the third trimester of pregnancy.
Prognosis
Relapse often occurs in patients with immunocompromise if treatment is stopped. Treatment may prevent the development of untoward sequelae in symptomatic and asymptomatic infants with congenital toxoplasmosis.
Seizure disorder or focal neurologic deficits may occur in CNS toxoplasmosis. Partial or complete blindness may occur with ocular toxoplasmosis. Multiple complications may occur with congenital toxoplasmosis, including intellectual disability, hydrocephalus, seizures, deafness, and blindness. [8]
Fetuses and immunocompromised individuals are at particularly high risk for severe sequelae and even death. Newborns with acute congenital toxoplasmosis often die in the first month of life. Infection acquired postnatally is usually much less severe. [9]
Patient Education
Explain toxoplasmosis prevention methods, such as protecting children's play areas from cat litter, to parents. Mothers who are infected with T gondii must be completely informed of potential consequences to their fetus.
-
Toxoplasma gondii trophozoites in tissue culture.