Practice Essentials
The broad category of thyroiditis includes the following inflammatory diseases of the thyroid gland: (1) acute suppurative thyroiditis, which is due to bacterial infection; (2) subacute thyroiditis, which results from a viral infection of the gland; and (3) chronic thyroiditis, which is usually autoimmune in nature. In childhood, chronic thyroiditis is the most common of these 3 types. The second form of thyroiditis, Riedel struma, is rare in children. Secondary thyroiditis may be due to the administration of amiodarone to treat cardiac arrhythmias or the administration of interferon-alpha to treat viral diseases. Laboratory studies are important in the workup of thyroiditis, while thyroid ultrasonography is useful in revealing abscess formation in patients with acute thyroiditis. Moreover, acute thyroiditis requires immediate parenteral antibiotic therapy before abscess formation begins.
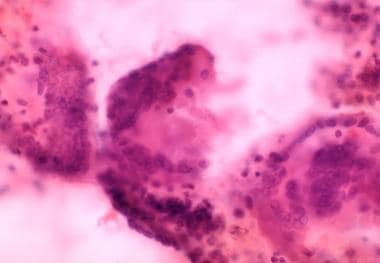 Three multinuclear, giant cell granulomas observed in a fine-needle aspiration biopsy of the thyroid; from a patient with thyrotoxicosis from lymphocytic or subacute granulomatous thyroiditis.
Three multinuclear, giant cell granulomas observed in a fine-needle aspiration biopsy of the thyroid; from a patient with thyrotoxicosis from lymphocytic or subacute granulomatous thyroiditis.
Signs and symptoms of thyroiditis
Characteristics of acute thyroiditis include the following
-
The patient may have a fever of 38-40°C
-
Acute illness may be evident
-
Neck tenderness is present, and the swollen thyroid gland is tender; the swelling and tenderness may be unilateral; erythemas develop over the gland, and regional lymphadenopathy may develop as the disease progresses; abscess formation may occur
Characteristics of subacute thyroiditis include the following:
-
The patient may have signs of systemic illness, such as low-grade fever and weakness
-
Signs of hyperthyroidism, including increased pulse rate, widened pulse pressure, fidgeting, tremor, nervousness, tongue fasciculations, brisk reflexes (possibly with clonus), weight loss, and warm, moist skin, may be present
-
The thyroid gland may be enlarged and tender, with tenderness exacerbated by neck extension
Characteristics of chronic autoimmune thyroiditis include the following:
-
Initially, an enlarged, lumpy, bumpy, and nontender thyroid is often present; the gland may not be enlarged, particularly in children who have profound hypothyroidism
-
Signs of hypothyroidism include slow growth rate; weight gain; slow pulse; cold, dry skin; coarse hair and facial features; edema; and delayed relaxation of the deep tendon reflexes
-
Signs of hyperthyroidism are occasionally present early in the disease
Diagnosis of thyroiditis
Laboratory test results vary according to the type of thyroiditis, as follows:
-
Acute thyroiditis - Laboratory abnormalities in acute thyroiditis reflect the acute systemic illness; findings include leukocytosis with a left shift and an increased sedimentation rate; thyroid function test results are within the reference range
-
Subacute thyroiditis - Initially, the thyroid-stimulating hormone (TSH) level is suppressed, and the free thyroxine (T4) level is increased; as the disorder progresses, transient or sometimes permanent hypothyroidism may develop
-
Chronic thyroiditis - TSH levels are increased in children with subclinical and overt hypothyroidism; free T4 levels are within the reference range in the former and low in the latter; in children with hyperthyroidism, TSH levels are suppressed; many children have normal thyroid function and normal TSH levels; antithyroid peroxidase (antithyrocellular, antimicrosomal) antibody levels elevated above the reference range are the most sensitive indicator of thyroid autoimmunity
Radioactive iodine thyroid scanning is helpful in patients with hyperthyroidism who are thought to have subacute thyroiditis, because the extremely low uptake is consistent with the thyrocellular destruction in progress. Thyroid ultrasonography is useful in revealing abscess formation in patients with acute thyroiditis.
In patients with acute thyroiditis, fine-needle aspiration can be used to obtain material for culture, enabling appropriate antibiotic therapy.
Management
Medical care in thyroiditis includes the following:
-
Acute thyroiditis - Acute thyroiditis requires immediate parenteral antibiotic therapy before abscess formation begins; for initial antibiotic therapy, administer penicillin or ampicillin to cover gram-positive cocci and the anaerobes that are the usual causes of the disease
-
Subacute thyroiditis - Subacute thyroiditis is self-limiting; therefore, the goals of treatment are to relieve discomfort and control abnormal thyroid function
-
Chronic autoimmune thyroiditis - Treatment for chronic autoimmune thyroiditis depends on the results of the thyroid function tests; patients with overt hypothyroidism who have high TSH and low free T4 levels require treatment with levothyroxine; the treatment of subclinical hypothyroidism in patients with elevated TSH and normal free T4 levels is controversial; these children may enter a remission phase and may not have permanent hypothyroidism (this appears to be a minority of subjects); most pediatric endocrinologists recommend treatment of subclinical hypothyroidism during childhood to ensure normal growth and development; if thyroxine administration may not be permanently required, treatment may be stopped once the patient has completed pubertal development, and thyroid function then can be reassessed
In acute thyroiditis, surgery may be necessary to drain the abscess and to correct the developmental abnormality responsible for the condition.
Pathophysiology
Acute suppurative thyroiditis is rare in childhood because the thyroid is remarkably resistant to hematogenously spread infection. Most cases of acute thyroiditis involve the left lobe of the thyroid and are associated with a developmental abnormality of thyroid migration and the persistence of a pyriform sinus from the pharynx to the thyroid capsule. The usual organisms responsible include Staphylococcus aureus, Streptococcus hemolyticus, and pneumococcus. Other aerobic or anaerobic bacteria may also be involved.
Subacute thyroiditis is generally thought to be due to viral processes and usually follows a prodromal viral illness. Various viral illnesses may precede the disease, including mumps, measles, influenza, infectious mononucleosis, adenoviral or Coxsackievirus infections, myocarditis, or the common cold. Other illnesses or situations associated with subacute thyroiditis include catscratch fever, sarcoidosis, Q fever, malaria, emotional crisis, or dental work. The disease is more common in individuals with human leukocyte antigen (HLA)–Bw35.
Because chronic thyroiditis in children is usually due to an autoimmune process, it is HLA-associated, similar to other autoimmune endocrine diseases. The specific alleles in the atrophic and goitrous forms of the disease vary. The histologic disease picture varies, but lymphocytic thyroid infiltration is the hallmark of the disease and frequently obliterates much of the normal thyroid tissue. Follicular thyroid cells may be small or hyperplastic. The degree of fibrosis among patients also widely varies. Children usually have hyperplasia with minimal fibrosis. The blood contains autoantibodies to thyroid peroxidase and, frequently, autoantibodies to thyroglobulin. Autoimmune thyroiditis is also frequently part of the polyglandular autoimmune syndromes.
Covid-19
A case study by Brancatella et al suggested that in some patients, subacute thyroiditis may arise from coronavirus disease 2019 (COVID-19). The report involved a woman aged 18 years who was found to have no thyroid disease before then testing positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). About three weeks later, she tested negative for the virus, but, a few days after that, presented with symptoms of subacute thyroiditis, which was subsequently diagnosed. The timing of the thyroiditis, the investigators believe, points to a COVID-19 origin, particularly in light of the fact that subacute thyroiditis is commonly thought to develop in response to viral infection or a postviral inflammatory reaction in persons with a genetic predisposition. [1, 2]
Additional research has continued to point to the development of a condition resembling subacute thyroiditis in persons with COVID-19. This includes an Italian study that found that among 85 patients with COVID-19 admitted to high-intensity-care units (HICUs), up to 13 (15%) were thyrotoxic, compared with just 1% of HICU patients from pre-pandemic 2019 who were studied in the report. [3, 4] However subacute thyroiditis following COVID-19 has not been reported in the pediatric age group, with the youngest reported case being age 18 years. [1, 5]
Further investigation indicates that subacute thyroiditis may persist months later in patients in whom the thyroid gland becomes inflamed during acute COVID-19 illness, even after normalization of thyroid function. In addition, the effects of SARS-CoV-2 on thyroid function appear to be multifactorial, with the thyroiditis being atypical in that no neck pain seems to be involved and more men than women appear to be affected. In addition, patients who were examined exhibited low TSH and free triiodothyronine (T3) levels, while free T4 levels were normal or elevated. [6]
There may also be an association between COVID-19 vaccination and the development of subacute thyroiditis, including with regard to mRNA and non-mRNA vaccines. However, a study by Ippolito et al indicates that the subacute thyroiditis cases are primarily of mild to moderate severity, with the investigators stating that most of these can be treated via symptomatic therapy or a short course of steroids. Therefore, according to the report, the vaccination/thyroiditis association “should not raise any concern regarding the need to be vaccinated, since the risks of COVID-19 undoubtedly outweigh the risks of the vaccination." The study did not report any instances of subacute thyroiditis following vaccination in patients younger than 18 years. [7]
Ippolito and colleagues also mention the possibility that in persons who receive an mRNA COVID-19 vaccine, the likelihood of developing subacute thyroiditis may be greater in those who have a previous history of thyroid disease. They found that out of the 51 patients in their study who developed subacute thyroiditis, approximately 12% (all of whom had been given an mRNA vaccine) had thyroid disease history; however, they indicate that further research is needed to support this contention. [7]
Epidemiology
Frequency
United States
Studies in the United States and Western Europe report a prevalence of 1.2% in individuals aged 11-18 years. Approximately 25% of adults with type 1 diabetes have thyroiditis, about one half of whom have hypothyroidism. Approximately 10% of children with type 1 diabetes have antithyroid antibodies. Thirteen of 121 children with vitiligo were also found to have subsequent evidence of autoimmune thyroiditis. [8] Similarly, a Korean study, by Bae et al, indicated that persons with vitiligo have an odds ratio for the autoimmune disease Hashimoto thyroiditis of 1.609. [9]
The disease is also more common in children with Down syndrome or Turner syndrome. However, a study by Vassilatou et al indicated that the risk of autoimmune thyroiditis is not increased in psoriatic patients with or without psoriatic arthritis, finding the prevalence of autoimmune thyroiditis to be 20.2% in psoriatic patients (n = 114) and 19.6% in controls (n = 286). [10] This contrasts with a study by Kiguradze et al, which reported an odds ratio of 2.49 for Hashimoto thyroiditis in persons with psoriasis. [11]
Acute suppurative thyroiditis is rare in Western nations. Subacute thyroiditis is rare in childhood.
International
The prevalence of chronic autoimmune thyroiditis varies depending on screening procedures. A Greek study showed a prevalence of thyroid antibodies as high as 12.5% in some areas. Few data are available regarding the incidence of the various forms of thyroiditis in the non-Western world. Acute thyroiditis is more common in geographic areas where antibiotic use is less prevalent.
Mortality/Morbidity
Long-term morbidity or mortality from thyroiditis is uncommon. Patients with autoimmune thyroiditis frequently develop hypothyroidism and require lifelong treatment. Patients with subacute thyroiditis may briefly have hyperthyroidism but usually regain normal thyroid function. Patients with acute thyroiditis generally maintain normal thyroid function.
A retrospective study by Ieni et al found that one third of patients with papillary thyroid cancer had chronic lymphocytic thyroiditis and that the thyroiditis patients tended to have more favorable characteristics with regard to their cancer. The investigators reported that in the patients with thyroiditis, tumors were smaller on average than in the other patients (9.39 mm vs 12 mm, respectively), and the lymph node metastasis rate was lower (12.5% vs 21.96%, respectively), while the tumor-node-metastasis (TNM) stage was prognostically better. The thyroiditis patients also tended to be younger. [12]
Similarly, a retrospective study by Pilli et al found that at a mean follow-up of 6.28 years, subsequent to treatment of papillary thyroid cancer with thyroidectomy and radioiodine remnant ablation, patients whose cancer was concurrent with chronic lymphocytic thyroiditis had a higher cure rate (91.8%) than did nonthyroiditis patients (76.3%). [13]
A prospective study by Zhao et al indicated that in patients with subacute thyroiditis, the early maximum thyroid-stimulating hormone (TSH) value (cutoff 7.83 mIU/L within 3 months of onset of subacute thyroiditis) predicts the development of hypothyroidism 2 years after the disease’s onset. [14]
Sex
The pediatric male-to-female ratio for autoimmune thyroiditis ranges from 1:2 to 1:6. This is low when compared with the 90% female predominance in adults. [15, 16, 17]
Prognosis
Acute thyroiditis
Recovery is usually complete, and thyroid function returns to normal.
Subacute thyroiditis
This self-limiting disease may last 2-7 months.
Chronic autoimmune thyroiditis
Permanent hypothyroidism is the main complication. Approximately 20% of children with subclinical hypothyroidism enter remission and become euthyroidism. [17]
-
Three multinuclear, giant cell granulomas observed in a fine-needle aspiration biopsy of the thyroid; from a patient with thyrotoxicosis from lymphocytic or subacute granulomatous thyroiditis.







