Practice Essentials
Thyroid storm, also referred to as thyrotoxic crisis, is an acute, life-threatening, hypermetabolic state induced by excessive release of thyroid hormones (THs) in individuals with thyrotoxicosis. [1] Thyroid storm may be the initial presentation of thyrotoxicosis in undiagnosed children, particularly in neonates. The clinical presentation includes fever, tachycardia, hypertension, and neurological and GI abnormalities. Hypertension may be followed by congestive heart failure that is associated with hypotension and shock. Because thyroid storm is almost invariably fatal if left untreated, rapid diagnosis and aggressive treatment are critical. Fortunately, this condition is extremely rare in children.
Diagnosis is primarily clinical, and no specific laboratory tests are available. Several factors may precipitate the progression of thyrotoxicosis to thyroid storm. In the past, thyroid storm was commonly observed during thyroid surgery, especially in older children and adults, but improved preoperative management has markedly decreased the incidence of this complication. Today, thyroid storm occurs more commonly as a medical crisis rather than a surgical crisis.
Signs and symptoms of thyroid storm
General signs and symptoms include the following [2] :
-
Fever
-
Profuse sweating
-
Poor feeding and weight loss
-
Respiratory distress
-
Fatigue (more common in older adolescents)
Gastrointestinal (GI) signs and symptoms include the following [2] :
-
Nausea and vomiting
-
Diarrhea
-
Abdominal pain
-
Jaundice [3]
Neurologic signs and symptoms include the following [2] :
-
Anxiety (more common in older adolescents)
-
Altered behavior
-
Seizures, coma
Workup in thyroid storm
The diagnosis of thyroid storm is based on clinical features, not on laboratory test findings. If the patient's clinical picture is consistent with thyroid storm, do not delay treatment pending laboratory confirmation of thyrotoxicosis.
Results of thyroid studies are usually consistent with hyperthyroidism and are useful only if the patient has not been previously diagnosed.
Usual findings include elevated triiodothyronine (T3), thyroxine (T4), and free T4 levels; increased T3 resin uptake; suppressed thyroid-stimulating hormone (TSH) levels; and an elevated 24-hour iodine uptake. TSH levels are not suppressed in the rare instances of excess TSH secretion.
Chest radiography may reveal cardiac enlargement due to congestive heart failure. Radiography may also reveal pulmonary edema caused by heart failure and/or evidence of pulmonary infection.
Head computed tomography (CT) scanning may be necessary to exclude other neurologic conditions if diagnosis is uncertain after the initial stabilization of a patient who presents with altered mental status.
Management of thyroid storm
The approach to treatment of thyroid storm includes the following:
-
Supportive measures
-
Antiadrenergic drugs
-
Thionamides
-
Iodine preparations
-
Glucocorticoids
-
Bile acid sequestrants
-
Treatment of the underlying condition
-
Rarely plasmapheresis
Patients with contraindications to thionamides need to be managed with supportive measures, aggressive beta blockade, iodine preparations, glucocorticoids, and bile acid sequestrants for about a week in preparation for a thyroidectomy. Plasmapheresis may be attempted if other measures are not effective.
Pathophysiology
Thyroid storm is a decompensated state of thyroid hormone–induced, severe hypermetabolism involving multiple systems and is the most extreme state of thyrotoxicosis. The clinical picture relates to severely exaggerated effects of THs due to increased release (with or without increased synthesis) or, rarely, increased intake of TH.
Heat intolerance and diaphoresis are common in simple thyrotoxicosis but manifest as hyperpyrexia in thyroid storm. Extremely high metabolism also increases oxygen and energy consumption. Cardiac findings of mild-to-moderate sinus tachycardia in thyrotoxicosis intensify to accelerated tachycardia, hypertension, high-output cardiac failure, and a propensity to develop cardiac arrhythmias. Similarly, irritability and restlessness in thyrotoxicosis progress to severe agitation, delirium, seizures, and coma. [4] GI manifestations of thyroid storm include diarrhea, vomiting, jaundice, and abdominal pain, in contrast to only mild elevations of transaminases and simple enhancement of intestinal transport in thyrotoxicosis.
Etiology
Thyroid storm is precipitated by the following factors in individuals with thyrotoxicosis:
-
Surgery
-
Anesthesia induction [5]
-
Radioactive iodine (RAI) therapy [6]
-
Drugs (anticholinergic and adrenergic drugs, eg, pseudoephedrine; salicylates; nonsteroidal anti-inflammatory drugs [NSAIDs]; chemotherapy [7]
-
Excessive thyroid hormone (TH) ingestion
-
Withdrawal of or noncompliance with antithyroid medications
-
Direct trauma to the thyroid gland
-
Vigorous palpation of an enlarged thyroid
-
Preeclampsia, hydatidiform mole, labor
Thyroid storm can occur in children with thyrotoxicosis from any cause but is most commonly associated with Graves disease. Other reported causes of thyrotoxicosis associated with thyroid storm include the following:
-
Transplacental passage of maternal thyroid-stimulating immunoglobulins in neonates
-
McCune-Albright syndrome with autonomous thyroid function [9]
-
Hyperfunctioning thyroid nodule
-
Hyperfunctioning multinodular goiter
-
Thyroid-stimulating hormone (TSH)-secreting tumor
Graves disease may also occur in children with Down syndrome or Turner syndrome and in association with other autoimmune conditions, including the following:
-
Chronic active hepatitis
The pathophysiologic mechanisms of Graves disease are shown in the image below.
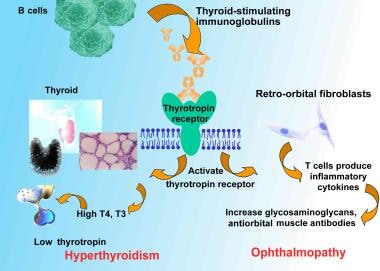 Pathophysiologic mechanisms of Graves disease relating thyroid-stimulating immunoglobulins to hyperthyroidism and ophthalmopathy. T4 is levothyroxine. T3 is triiodothyronine.
Pathophysiologic mechanisms of Graves disease relating thyroid-stimulating immunoglobulins to hyperthyroidism and ophthalmopathy. T4 is levothyroxine. T3 is triiodothyronine.
Although the exact pathogenesis of thyroid storm is not fully understood, the following theories have been proposed:
-
Patients with thyroid storm reportedly have relatively higher levels of free THs than patients with uncomplicated thyrotoxicosis, although total TH levels may not be increased.
-
Adrenergic receptor activation is another hypothesis. Sympathetic nerves innervate the thyroid gland, and catecholamines stimulate TH synthesis. In turn, increased THs increase the density of beta-adrenergic receptors, thereby enhancing the effect of catecholamines. The dramatic response of thyroid storm to beta-blockers and the precipitation of thyroid storm after accidental ingestion of adrenergic drugs such as pseudoephedrine support this theory. This theory also explains normal or low plasma levels and urinary excretion rates of catecholamines. However, it does not explain why beta-blockers fail to decrease TH levels in thyrotoxicosis.
-
Another theory suggests a rapid rise of hormone levels as the pathogenic source. A drop in binding protein levels, which may occur postoperatively, might cause a sudden rise in free hormone levels. In addition, hormone levels may rise rapidly when the gland is manipulated during surgery, during vigorous palpation during examination, or from damaged follicles following RAI therapy.
-
Other proposed theories include alterations in tissue tolerance to THs, the presence of a unique catecholaminelike substance in thyrotoxicosis, and a direct sympathomimetic effect of TH as a result of its structural similarity to catecholamines.
Epidemiology
Frequency
In the US, the true frequency of thyrotoxicosis and thyroid storm in children is unknown. The incidence of thyrotoxicosis increases with age. Thyrotoxicosis may affect as many as 2% of older women. Children constitute less than 5% of all thyrotoxicosis cases. Graves disease is the most common cause of childhood thyrotoxicosis and, in a possibly high estimate, reportedly affects 0.2-0.4% of the pediatric and adolescent population. About 1-2% of neonates born to mothers with Graves disease manifest thyrotoxicosis.
Based on nationwide surveys conducted between 2004 and 2008, the incidence of thyroid storm in Japan has been estimated to be 0.2 persons per 100,000 population, with the rate of thyroid storm in all thyrotoxic patients being 0.22%, and in hospitalized thyrotoxic patients, 5.4%. [10]
Sex
Thyrotoxicosis is 3-5 times more common in females than in males, especially among pubertal children. Thyroid storm affects a small percentage of patients with thyrotoxicosis. The incidence is presumed to be higher in females; however, no specific data regarding sex-specific incidence are available.
Age
Neonatal thyrotoxicosis occurs in 1-2% of neonates born to mothers with Graves disease. Infants younger than 1 year constitute only 1% of cases of childhood thyrotoxicosis. More than two thirds of all cases of thyrotoxicosis occur in children aged 10-15 years. Overall, thyrotoxicosis occurs most commonly during the third and fourth decades of life. Because childhood thyrotoxicosis is more likely to occur in adolescents, thyroid storm is more common in this age group, although it can occur in patients of all ages.
Prognosis
Thyroid storm is an acute, life-threatening emergency. If untreated, thyroid storm is almost invariably fatal in adults (90% mortality rate) and is likely to cause a similarly severe outcome in children, although the condition is so rare in children that these data are not available. Death from thyroid storm may be a consequence of cardiac arrhythmia, congestive heart failure, hyperthermia, multiple organ failure, or other factors, [11] though the precipitating factor is often the cause of death.
With adequate thyroid-suppressive therapy and sympathetic blockade, clinical improvement should occur within 24 hours. Adequate therapy should resolve the crisis within a week. Treatment for adults has reduced mortality to less than 20%. In one retrospective study from Japan of 1324 patients who were diagnosed with thyroid storm, the overall mortality was 10%. [12] In the same study, the following factors were associated with increased mortality risk in thyroid storm [12] :
-
Age 60 years or older
-
Central nervous system (CNS) dysfunction at admission
-
Lack of antithyroid drug and beta-blockade use
-
Need for mechanical ventilation and plasma exchange along with hemodialysis
In addition, a study by Swee et al of 28 patients with thyroid storm reported that CNS dysfunction of greater than mild severity appeared to be a risk factor for mortality. [13]
Using the National (Nationwide) Inpatient Sample database, a study by Waqar et al indicated that in hospitalized patients with thyroid storm, the inhospital mortality rate is higher in those with cardiovascular events than in persons without (3.5% vs 0.2%, respectively). The cardiovascular events that were most frequently associated with thyroid storm in hospitalized patients were arrhythmia (96.8%), acute heart failure (14.2%), and ischemic events (3.9%). Of patients with an ischemic event, 16.7% suffered inhospital mortality, compared with 3.6% and 3.2% of those with acute heart failure or arrhythmia, respectively. [14]
A retrospective study by Bourcier et al of 31 French intensive care units (ICUs) found that in ICU patients with thyroid storm, multiple organ failure (as evaluated using the Sequential Organ Failure Assessement [SOFA] score, absent the cardiovascular component), and the occurrence, within 48 hours following ICU admission, of cardiogenic shock are independent risk factors for mortality in the ICU. [15]
A study by Burmeister reported a mortality rate of 38% in patients with thyroid storm–related coma, including 70% between 1935 and 1977, and 11% between 1978 and 2019. The investigator found that there was a greater tendency for patients to awaken from their coma when total and free T4 values, and possibly the total T3 value as well, was reduced. Moreover, the employment of antithyroid drugs, corticosteroids, beta blockers, and intubation correlated positively with lower death rates. Although plasmapheresis-related awakenings occurred in 67% of patients in which plasmapheresis was used, the procedure was not linked to a reduction in the death rate. [16]
Patient Education
For excellent patient education resources, visit eMedicineHealth's Thyroid and Metabolism Center. Also, see eMedicineHealth's patient education articles Thyroid Problems and Thyroid Storm.
-
Pathophysiologic mechanisms of Graves disease relating thyroid-stimulating immunoglobulins to hyperthyroidism and ophthalmopathy. T4 is levothyroxine. T3 is triiodothyronine.









