Background
In simple terms, an atrial septal defect (ASD) is a deficiency of the atrial septum. Atrial septal defects account for about 10-15% of all congenital cardiac anomalies and are the most common congenital cardiac lesion presenting in children and adults. [1] Sinus venosus atrial septal defects account for only 10% of atrial septal defects. The remaining atrial septal defects are ostium secundum type (70%), ostium primum type (20%), and unroofed coronary sinus, or coronary sinus septal defects, (< 1%). Most children with sinus venosus atrial septal defects are asymptomatic but may develop symptoms as they age.
Excellent surgical results with a mortality rate near 0% can be expected. This is particularly true in patients who undergo repair when younger than 15 years. An atrial septal defect was the first lesion repaired using cardiopulmonary bypass in 1954 by John Gibbon, MD, at the Mayo Clinic.
Pathophysiology
The more common sinus venosus type defect (often referred to as the "usual type") occurs in the upper atrial septum and is contiguous with the superior vena cava (SVC). The lesion is rostral and posterior to the fossa ovalis (where secundum type defects occur) and is separate from it. It is almost always associated with anomalous pulmonary venous drainage of the right upper pulmonary vein into the SVC. See the image below.
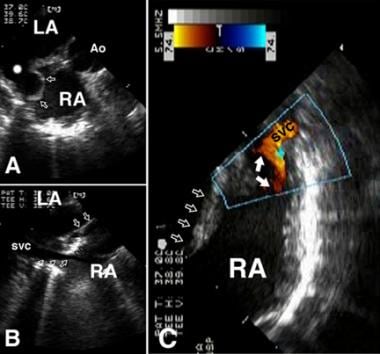 Panel A. Transesophageal echocardiogram (transverse view) of a patient with a sinus venosus defect of the superior vena cava (SVC) type. The original defect (white star burst) has been repaired by placing a baffle (arrows), which directs blood from the anomalously connected right upper pulmonary vein into the left atrium (LA). In this patient, the baffle was redundant so at a more rostral level (Panel B), it could be seen (black open arrows) to bulge into the superior vena cava (SVC)–right atrial (RA) junction (trio of white arrows). The remainder of the atrial septum is denoted by the duo of white open arrows. Panel C is a transesophageal echocardiogram, sagittal view. Doppler color flow mapping verifies that the protruding baffle (white closed arrows) results in a narrowing of the pathway from the SVC to the RA. The quartet of white open arrows points to the remainder of the atrial septum.
Panel A. Transesophageal echocardiogram (transverse view) of a patient with a sinus venosus defect of the superior vena cava (SVC) type. The original defect (white star burst) has been repaired by placing a baffle (arrows), which directs blood from the anomalously connected right upper pulmonary vein into the left atrium (LA). In this patient, the baffle was redundant so at a more rostral level (Panel B), it could be seen (black open arrows) to bulge into the superior vena cava (SVC)–right atrial (RA) junction (trio of white arrows). The remainder of the atrial septum is denoted by the duo of white open arrows. Panel C is a transesophageal echocardiogram, sagittal view. Doppler color flow mapping verifies that the protruding baffle (white closed arrows) results in a narrowing of the pathway from the SVC to the RA. The quartet of white open arrows points to the remainder of the atrial septum.
Less commonly, the defect may occur at the junction of the right atrium and inferior vena cava (IVC) and be associated with anomalous connection of the right lower pulmonary vein to the IVC. Rarely, sinus venosus defects occur posterior to the fossa ovalis without bordering the SVC or IVC. The predominant hemodynamic consequence is a left-to-right shunt through the defect. See the image below.
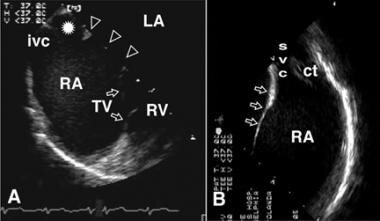 Panel A is a transesophageal echocardiogram, transverse view. The white star burst shows the sinus venosus defect of the inferior vena cava (IVC) type, lying adjacent to the IVC junction with the right atrium (RA). The remainder of the atrial septum is just out of the view of this sector but is represented by the white open arrowheads. The leaflets of the closed tricuspid valve (TV) are visible. RV = right ventricle. Panel B is a transesophageal echocardiogram, sagittal view. This is the same patient as in Panel A. This view proves that the rostral portion of the atrial septum (which would be missing in a patient with a sinus venosus defect of the SVC type) is intact. ct = crista terminalis; svc = superior vena cava.
Panel A is a transesophageal echocardiogram, transverse view. The white star burst shows the sinus venosus defect of the inferior vena cava (IVC) type, lying adjacent to the IVC junction with the right atrium (RA). The remainder of the atrial septum is just out of the view of this sector but is represented by the white open arrowheads. The leaflets of the closed tricuspid valve (TV) are visible. RV = right ventricle. Panel B is a transesophageal echocardiogram, sagittal view. This is the same patient as in Panel A. This view proves that the rostral portion of the atrial septum (which would be missing in a patient with a sinus venosus defect of the SVC type) is intact. ct = crista terminalis; svc = superior vena cava.
Etiology
During normal embryonic development, the right horn of the sinus venosus encompasses the right superior vena cava (SVC) and inferior vena cava (IVC). If abnormal resorption of the sinus venosus occurs, an atrial septal defect results near the orifice of either the SVC or IVC.
Atrial septal defects occur as associated anomalies in many major complex congenital lesions but sinus venosus atrial septal defects occur more often as an isolated abnormality.
Other abnormalities may exacerbate an atrial septal defect. For example, systemic hypertension in an adult with a sinus venosus atrial septal defect may result in left ventricular hypertrophy and reduce left ventricular compliance, which, in turn, exacerbates the atrial level left-to-right shunt. Mitral stenosis, which is either congenital or acquired, may also exacerbate the atrial level left-to-right shunt.
Epidemiology
United States data
Sinus venosus atrial septal defects represent approximately 1% of congenital cardiac lesions.
Race-, sex-, and age-related demographics
No racial predilection is known; however, atrial septal defects affect females more often than males. The female-to-male ratio is 2:1. No difference in outcome is associated with sex.
Sinus venosus atrial septal defects are congenital lesions present at birth. The age at presentation depends on the size of the left-to-right shunt (atrial and partial anomalous pulmonary venous return). Atrial septal defects in infancy are usually asymptomatic. They are usually detected by echocardiography while undergoing a cardiac evaluation.
Prognosis
The prognosis is excellent for young patients who undergo repair of uncomplicated defects. Repair delayed until the third decade of life is associated with a decrease in life expectancy. [2]
Morbidity/mortality
Surgical repair in the first 2 decades of life is associated with a mortality rate near zero. Life expectancy approaches that of the general population if the defect is repaired during this time. Right heart dilation rapidly regresses after surgery, and the functional result is excellent. In cases of repair during adulthood, life expectancy may be decreased despite successful repair. Surgical morbidity rates are related to early postoperative pericardial effusion, early postoperative pulmonary venous or systemic venous obstruction, and supraventricular arrhythmias. If the baffle directing pulmonary venous blood to the left atrium is not placed correctly, it may obstruct pulmonary venous drainage. If the baffle bulges into the superior vena cava (SVC), it may obstruct SVC inflow, necessitating the placement of an augmentation patch on the anterior surface of the SVC and right atrial junction.
Untreated atrial septal defects are associated with a significantly shortened life expectancy. After age 20 years, the mortality rate is approximately 5% per decade with 90% of patients dead by age 60 years. These patients present with an increase in left-to-right shunting and occasionally with congestive heart failure with pulmonary hypertension in the fourth to sixth decades of life. Guidelines for the diagnosis and treatment of pulmonary artery hypertension have been established. [3] Late problems in untreated patients also include the risk of paradoxical embolus as well as atrial fibrillation, pulmonary hypertension, and right heart failure.
Complications
Complications include the following:
-
Pulmonary venous obstruction
-
Atrial fibrillation, atrial flutter, or supraventricular tachycardia (SVT)
-
Pulmonary hypertension
-
Atrial baffle leak
-
Pericardial effusion or postpericardiotomy syndrome
-
SVC syndrome
Patient Education
Patient education mainly focuses on preoperative and postoperative care and recovery, which are especially important in young children undergoing surgery. Centers with experienced child life personnel are invaluable in preparing children for open-heart surgery.
-
Panel A. Transesophageal echocardiogram (transverse view) of a patient with a sinus venosus defect of the superior vena cava (SVC) type. The original defect (white star burst) has been repaired by placing a baffle (arrows), which directs blood from the anomalously connected right upper pulmonary vein into the left atrium (LA). In this patient, the baffle was redundant so at a more rostral level (Panel B), it could be seen (black open arrows) to bulge into the superior vena cava (SVC)–right atrial (RA) junction (trio of white arrows). The remainder of the atrial septum is denoted by the duo of white open arrows. Panel C is a transesophageal echocardiogram, sagittal view. Doppler color flow mapping verifies that the protruding baffle (white closed arrows) results in a narrowing of the pathway from the SVC to the RA. The quartet of white open arrows points to the remainder of the atrial septum.
-
Panel A is a transesophageal echocardiogram, transverse view. The white star burst shows the sinus venosus defect of the inferior vena cava (IVC) type, lying adjacent to the IVC junction with the right atrium (RA). The remainder of the atrial septum is just out of the view of this sector but is represented by the white open arrowheads. The leaflets of the closed tricuspid valve (TV) are visible. RV = right ventricle. Panel B is a transesophageal echocardiogram, sagittal view. This is the same patient as in Panel A. This view proves that the rostral portion of the atrial septum (which would be missing in a patient with a sinus venosus defect of the SVC type) is intact. ct = crista terminalis; svc = superior vena cava.







