Practice Essentials
Human scabies is an intensely pruritic skin infestation caused by the host-specific mite Sarcoptes scabiei hominis. Approximately 300 million cases of scabies (see the image below) are reported worldwide each year.
 Scabies. Erythematous vesicles and papules are present on torso extremities, some with adjacent linear excoriations.
Scabies. Erythematous vesicles and papules are present on torso extremities, some with adjacent linear excoriations.
Also see Scabies Organism-Specific Therapy.
Signs and symptoms
Burrows are a pathognomonic sign and represent the intraepidermal tunnel created by the moving female mite. They appear as serpiginous, grayish, threadlike elevations in the superficial epidermis, ranging from 2-10 mm long. High-yield locations for burrows include the following:
-
Webbed spaces of the fingers
-
Flexor surfaces of the wrists
-
Elbows
-
Axillae
-
Belt line
-
Feet
-
Scrotum (men)
-
Areolae (women)
Classic scabies typically has a distribution involving the axillae, elbow flexures, wrists and hands, and genital area. This is commonly known as the circle of Hebra.
In geriatric patients, scabies demonstrates a propensity for the back, often appearing as excoriations. In infants and small children, burrows are commonly located on the palms and soles.
One- to 3-mm erythematous papules and vesicles are seen in typical distributions in adults. The vesicles are discrete lesions filled with clear fluid, although the fluid may appear cloudy if the vesicle is more than a few days old.
Nodular scabies
Nodules occur in 7-10% of patients with scabies, particularly young children. In neonates unable to scratch, pinkish brown nodules ranging in size from 2-20 mm in diameter may develop.
Crusted scabies
In crusted scabies, lesions are often hyperkeratotic and crusted and cover large areas. Marked scaling is common, and pruritus may be minimal or absent. Nail dystrophy and scalp lesions may be prominent. The hands and arms are the usual locations for lesions, but all sites are vulnerable.
Secondary lesions
These lesions result from scratching, secondary infection, and/or the host’s immune response against the scabies mites and their products. Characteristic findings include the following [1, 2, 3] :
-
Excoriations
-
Widespread eczematous dermatitis
-
Honey-colored crusting
-
Postinflammatory hyperpigmentation
-
Erythroderma
-
Prurigo nodules
-
Frank pyoderma
See Presentation for more detail.
Diagnosis
The diagnosis of scabies can often be made clinically in patients with a pruritic rash and characteristic linear burrows. The diagnosis is confirmed by light microscopic identification of mites, larvae, ova, or scybala (feces) in skin scrapings.
In rare cases, mites are identified in biopsy specimens obtained to rule out other dermatoses. Characteristic histopathology in the absence of actual mites also may suggest the diagnosis of scabies.
Clinically inapparent infection can be detected by amplification of Sarcoptes DNA in epidermal scale by polymerase chain reaction (PCR) assay. [4] In addition, elevated immunoglobulin E (IgE) titers and eosinophilia may be demonstrated in some patients with scabies.
See Workup for more detail.
Management
Scabies treatment includes administration of a scabicidal agent (eg, permethrin, lindane, or ivermectin), as well as an appropriate antimicrobial agent if a secondary infection has developed.
Pruritus may be partially alleviated with an oral antihistamine, such as hydroxyzine hydrochloride (Atarax), diphenhydramine hydrochloride (Benadryl), or cyproheptadine hydrochloride (Periactin). In rare cases, prednisone may be used to treat severe pruritus.
Because of their heavy mite burden, patients with crusted scabies may require repeated applications of topical scabicides or treatment that simultaneously uses oral ivermectin and a topical agent, such as permethrin.
See Treatment and Medication for more detail.
Background
Human scabies is an intensely pruritic skin infestation caused by the host-specific mite Sarcoptes scabiei var hominis. A readily treatable infestation, scabies remains common primarily because of diagnostic difficulty, inadequate treatment of patients and their contacts, and improper environmental control measures. Scabies is a great clinical imitator. Its spectrum of cutaneous manifestations and associated symptoms often results in delayed diagnosis. In fact, the term "7-year itch" was first used with reference to persistent, undiagnosed infestations with scabies (see the image below). (See Presentation, Workup, Treatment, and Medication.)
Scabies is a global public health problem, affecting persons of all ages, races, and socioeconomic groups. Worldwide, an estimated 300 million cases occur annually. [5] Overcrowding, delayed diagnosis and treatment, and poor public education contribute to the prevalence of scabies in industrial and developing nations.
Prevalence rates are higher in children and sexually active individuals than in other persons. Patients with poor sensory perception due to entities such as leprosy and persons with immunocompromise due to conditions such as status posttransplantation, human immunodeficiency virus (HIV) disease, and old age are at particular risk for the crusted variant. These populations present with clinically atypical lesions and often are misdiagnosed, thus delaying treatment and elevating the risk of local epidemics.
Pathophysiology
Mode of transmission
Transmission of scabies is predominantly through direct skin-to-skin contact, and for this reason scabies has been considered a sexually transmitted disease. The mite does not penetrate deeper than the superficial layer of the epidermis, the stratum corneum.
A person infested with mites can spread scabies even if he/she is asymptomatic. [6] There may be a prolonged interval (up to 10 wk) between the primary infection, when the patient becomes contagious, and the onset of clinical manifestations. [7, 8] Scabies is less frequently transmitted by indirect contact through fomites such as infested bedding or clothing. However, the greater the number of parasites on a person, as in crusted scabies, the more likely that indirect contact will transmit the disease.
The S scabiei hominis mite that infects humans is female and is large enough (0.3-0.4 mm long) to be seen with the naked eye. (The male is about half this size.) The mite has 4 pairs of legs and crawls at a rate of 2.5 cm/min; it is unable to fly or jump. [9] Although its life cycle occurs completely on the host, the mite is able to live on bedding, clothes, or other surfaces at room temperature for 2-3 days, while remaining capable of infestation and burrowing. At temperatures below 20°C, S scabiei are immobile, although they can survive such temperatures for extended periods. (See the image below.)
Mite life cycle
The scabies mite is an obligate parasite that completes its entire life cycle on humans. Other variants of the scabies mite can cause infestation in other mammals, such as dogs, cats, pigs, ferrets, and horses, although they can irritate human skin as well. However, they are unable to reproduce in humans and cause only a transient dermatitis.
The female S scabiei var hominis mite lays 60-90 eggs in her 30-day lifespan, although less than 10% of the eggs result in mature mites. The average patient is infected with 10-15 live adult female mites at any given time. Life cycle stages are as follows (see the images below) [6] :
Eggs incubate and hatch in 3-4 days (90% of the hatched mites die)
Larvae (3 pairs of legs) migrate to the skin surface and burrow into the intact stratum corneum to make short burrows, called molting pouches (3-4 days)
Larvae molt into nymphs (4 pairs of legs), which molt once into larger nymphs before becoming adults
Mating takes place once, and the female is fertile for the rest of her life; the male dies soon after mating
The female makes a serpentine burrow using proteolytic enzymes to dissolve the stratum corneum of the epidermis, laying eggs in the process; she continues to lengthen her burrow and lay eggs for the rest of her life, surviving 1-2 months
Transmission of impregnated females from person-to-person occurs through direct or indirect skin contact
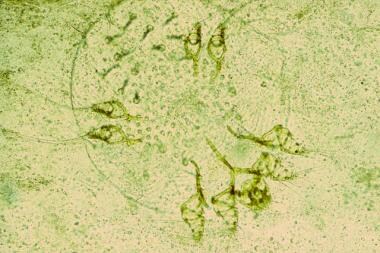
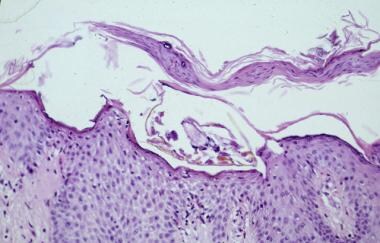 In routine scabies, a single mite is seen. Eosinophilic spongiosis may be present (hematoxylin and eosin; original magnification, 400X).
In routine scabies, a single mite is seen. Eosinophilic spongiosis may be present (hematoxylin and eosin; original magnification, 400X).
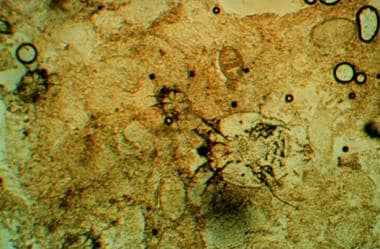
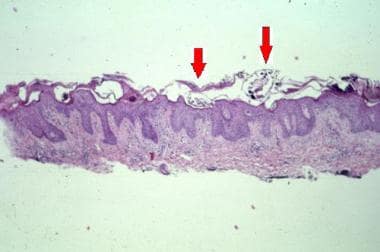 In crusted scabies, sections show multiple mites (arrows) within the hyperkeratotic stratum corneum. The epidermis is spongiotic (hematoxylin and eosin; original magnification, 100X).
In crusted scabies, sections show multiple mites (arrows) within the hyperkeratotic stratum corneum. The epidermis is spongiotic (hematoxylin and eosin; original magnification, 100X).
Classic scabies
In classic scabies infection, typically 10-15 mites (range, 3-50) live on the host. [9] Little evidence of infection exists during the first month (range, 2-6 wk), but after 4 weeks and with subsequent infections, a delayed type IV hypersensitivity reaction to the mites, eggs, and scybala (feces) occurs. The time required to induce immunity in primary infestations probably accounts for the 4-week asymptomatic latent period. With reinfestation, the sensitized individual may develop a rapid reaction (within hours). The resultant skin eruption and its associated intense pruritus are the hallmarks of classic scabies. (See the images below.)
 Scabies. Erythematous vesicles and papules are present on torso extremities, some with adjacent linear excoriations.
Scabies. Erythematous vesicles and papules are present on torso extremities, some with adjacent linear excoriations.
An immunologic study analyzing the cellular infiltrate types and patterns in scabies lesions concluded that T4-cell dominance is the cause of persistent itching, while an increase in T8 cells reduces pruritus. [10]
Crusted scabies
Crusted, or Norwegian, scabies (so named because the first description was from Norway in the mid-1800s) is a distinctive and highly contagious form of the disease. In this variant, hundreds to millions of mites infest the host individual, who is usually immunocompromised, elderly, or physically or mentally disabled and impaired. (Assessment of immune function may be indicated in individuals presenting with crusted scabies.) [11, 12] Some data suggest a higher incidence of autoimmune diseases in patients with scabies. [13]
Crusted scabies can be easily confused with severe dermatitis or psoriasis because widespread, crusted lesions appear with thick, hyperkeratotic scales over the elbows, knees, palms, and soles. The diagnosis of crusted scabies should be considered when suspected dermatitis or suspected psoriasis does not respond to usual treatments. (See the images below.) [2]
Serum immunoglobulin E (IgE) and IgG levels are extremely high in patients with crusted scabies, yet the immune reaction does not seem to be protective. Cell-mediated immunity in classic scabies demonstrates T4-cell predominance in the dermal infiltrate, while one study suggests a T8-cell predominance in crusted scabies.
Certain patient populations are susceptible to crusted scabies. These include patients with primary immunodeficiency disorders or a compromised ability to mount an immune response secondary to drug therapy. A modified host response may be a key factor in patients with malnutrition. Motor nerve impairments result in the inability to scratch in response to the pruritus, thus disabling the utility of scratching to remove mites and destroy burrows. Rare cases have been described in which immunocompetent patients have developed the crusted variant without clear explanation.
Etiology
Human scabies is caused by the host-specific mite S scabiei hominis, an obligate human parasite. It is a member of the family Sarcoptidae, which belongs to the order Astigmata, in the subclass Acari, class Arachnida.
Human infestation with S scabiei varieties of animal origin can occur. Domestic and wild animals worldwide are susceptible to infestation with S scabiei, and the resultant disease is referred to as sarcoptic mange. Mange due to S scabiei varieties other than hominis has been reported in dogs, pigs, horses, camels, black bears, monkeys, dingoes, and wild foxes, among other animals.
Although reports have described transfer to humans from animals, experimental studies have demonstrated limited cross-infectivity between different host species. Further, genotyping studies have revealed that the Sarcoptes mites segregate into separate host-associated populations, thus limiting the transmission across host species.
In the rare instance of transmission of nonhuman scabies from animals to humans, the clinical manifestations differ in many respects. The incubation period is shorter, the symptoms are transient, the infestation is self-limiting, no burrows are formed, and the distribution is atypical compared with infestation caused by S scabiei hominis. Contacts of patients with scabies contracted from an animal source require no treatment.
Risk factors
Prevalence rates for scabies are higher in children and sexually active individuals than in other persons. Patients with poor sensory perception due to entities such as leprosy and persons with immunocompromise due to conditions such as status posttransplantation, human immunodeficiency virus (HIV) disease, and old age are at particular risk for the crusted variant.
A 2009 study conducted in an impoverished rural community in Brazil identified the following major risk factors for scabies in that community [14] :
-
Young age
-
Presence of many children in the household
-
Illiteracy
-
Low family income
-
Poor housing
-
Sharing clothes and towels
-
Irregular use of showers
Epidemiology
An estimated 200 million people are affected by scabies at any given time, with prevalence rates ranging from 0.2% to 71%. [15] Natural disasters, war, and poverty lead to overcrowding and increased rates of transmission. [16, 17]
In industrialized countries, scabies epidemics occur primarily in institutional settings, such as prisons, and in long-term care facilities, including hospitals and nursing homes. [18, 19, 20] Scabies occurs more commonly in fall and winter months in these countries. Prevalence rates for scabies in developing nations are higher than those in industrialized countries.
A survey of children in a welfare home in Pulau Pinang, Malaysia found that the infestation rate for scabies was highest among children aged 10-12 years. [21] The disease was more commonly evident in boys (50%) than in girls (16%). The overall prevalence rate for scabies was 31%.
Of 200 dermatology outpatients in Sirte, Libya, with scabies, the following distribution was found [22] :
-
Females - 59%
-
Children - 37.5%
-
Military personnel - 18%
While many accounts of the epidemiology of scabies suggest that epidemics or pandemics occur in 30-year cycles, this may be an oversimplification of its incidence, since these accounts have coincided with the major wars of the 20th century. Because it is not a reportable disease and data are based on variable notification, the incidence of scabies is difficult to ascertain.
Scabies is clearly an endemic disease in many tropical and subtropical regions, being 1 of the 6 major epidermal parasitic skin diseases (EPSD) that are prevalent in resource-poor populations, as reported in the Bulletin of the World Health Organization in February 2009. [23] Prevalence rates are extremely high in aboriginal tribes in Australia, Africa, South America, [24] and other developing regions of the world. Incidence in parts of Central and South America approach 100%. [23] One report suggests the highest reported rates of the crusted scabies in the world is in remote Aboriginal communities of northern Australia. [25]
Age-related demographics
The World Health Organization reports a prevalence rate of 5-10% in children in resource-poor tropical countries. [15]
In a 2009 retrospective study of 30,078 children in India, scabies was found to be the second most common skin disease in all age groups of children and the third most common skin disease in infants. [26]
In parts of Bangladesh, the number of children with scabies exceeds the number with diarrheal and respiratory diseases combined. [23]
Prognosis
With proper diagnosis and treatment, the prognosis in otherwise healthy individuals with classic scabies is excellent. If one medication is ineffective, the sequential use of agents can be curative. Immunocompromised or institutionalized individuals are at an increased risk for crusted scabies, which is associated with a less favorable outcome.
Persistent symptoms in scabies may last up to 2-4 weeks after treatment. Anxiety or a hypersensitivity state may prolong symptoms even after the mites have been destroyed. [27] Residual pruritus may require antihistamines or a short course of topical or oral steroids. If symptoms last longer than 2-4 weeks, treat the patient with another dose of scabicides. [6, 9, 7]
Symptoms may also persist as a result of the following:
-
Treatment failure
-
Allergic dermatitis due to the topical medicine used
-
Ordinary household mites that cause a cross reactivity, driving persistent symptoms
-
Acarophobia - Delusional parasitosis; requires psychiatric intervention
-
Secondary infection requiring antibiotics
Morbidity/mortality
Complications of scabies are rare and generally result from vigorous rubbing and scratching. Disruption of the skin barrier puts the patient at risk for secondary bacterial invasion, primarily by Streptococcus pyogenes and Staphylococcus aureus. [28, 29] Superinfection with S pyogenes can precipitate acute poststreptococcal glomerulonephritis, chronic renal failure, and even rheumatic fever.
Common pyodermas include impetigo and cellulitis, which in rare cases cause sepsis. [30] The staphylococci or streptococci in the lesions can also lead to pyelonephritis, abscesses, pyogenic pneumonia, sepsis, and death.
A retrospective, matched-cohort study by Chung et al comparing more than 5000 patients with scabies with more than 25,000 randomly selected subjects found an association between scabies and increased risk of chronic kidney disease. It was determined that the likelihood of being diagnosed with chronic kidney disease during the study’s 5-year follow-up period was 1.4 times greater in males with scabies than in those without it, and that it was 1.27 times greater in females with scabies than in females without it. [31]
Complications can also result if a scabies infestation exacerbates underlying eczema, psoriasis, transient acantholytic dermatosis (Grover disease), or another preexisting dermatosis. Even with appropriate treatment, scabies can leave in its wake residual eczematous dermatitis and/or postscabietic pruritus, which can be debilitating and recalcitrant. [32]
In remote Aboriginal communities in Australia, where scabies is endemic, extremely high levels of renal failure and rheumatic heart disease appear to be related to repeated scabies infestations and secondary streptococcal infections.
Crusted scabies carries a higher mortality rate than the classic form of the disease, because of the frequency of secondary bacterial infections resulting in sepsis. Patients with crusted scabies often contribute to widespread infestation in long-term care facilities, and delays in diagnosis contribute to the spread. [33]
Patient Education
Additional information can be obtained from the Centers for Disease Control and Prevention, Parasites - Scabies site and from the American Academy of Dermatology.
-
Scabies mite scraped from a burrow (original magnification, 400X).
-
A typical linear burrow on the flexor forearm. Courtesy of Kenneth E. Greer, MD.
-
A subtle linear burrow accompanied by erythematous papules on the sole of the foot in a child with scabies. Courtesy of Kenneth E. Greer, MD.
-
Erythematous papules and papulovesicles on the flexor wrist. Courtesy of Kenneth E. Greer, MD.
-
Scabies on the penile shaft and glans. Courtesy of William D. James, MD.
-
Scabietic papules on the penile shaft and scrotum. Courtesy of Kenneth E. Greer, MD.
-
Widespread eruption on the back of an infant with scabies. Courtesy of Kenneth E. Greer, MD.
-
Nodular scabies in an infant. Courtesy of Kenneth E. Greer, MD.
-
Nodular scabies. Courtesy of Kenneth E. Greer, MD.
-
Crusted scabies. Courtesy of William D. James, MD.
-
Crusted scabies. Courtesy of Kenneth E. Greer, MD.
-
Scabies preparation demonstrating a mite and ova. Courtesy of William D. James, MD.
-
Scabies. Erythematous vesicles and papules are present on torso extremities, some with adjacent linear excoriations.
-
In routine scabies, a single mite is seen. Eosinophilic spongiosis may be present (hematoxylin and eosin; original magnification, 400X).
-
Scabies mite in the stratum corneum. Courtesy of William D. James, MD.
-
In crusted scabies, sections show multiple mites (arrows) within the hyperkeratotic stratum corneum. The epidermis is spongiotic (hematoxylin and eosin; original magnification, 100X).
-
Scabies. Courtesy of William D. James, MD.
-
Scabies in the interdigital web spaces. Courtesy of William D. James, MD.
-
Papulovesicles and nodules on the palm in a patient with scabies. Courtesy of Kenneth E. Greer, MD.
-
Scabies on buttocks. Courtesy of William D. James, MD.
-
Scabies on penis. Courtesy of Hon Pak, MD.