Practice Essentials
Proteus syndrome is a rare condition that can be loosely categorized as a hamartomatous disorder. It is a complex disorder with multisystem involvement and great clinical variability. [1] Once thought to have neurofibromatosis, Joseph Merrick (also known as "the elephant man" and studied by Treves in the 19th century) is now, in retrospect, thought by clinical experts to actually have had Proteus syndrome.
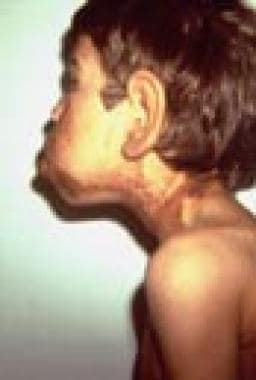
This condition is characterized by various cutaneous and subcutaneous lesions, including vascular malformations, lipomas, hyperpigmentation, and several types of nevi. [2] Cerebriform nevi are thought to be characteristic of the disorder. [3] Progressive, asymmetrical limb overgrowth is pathognomonic, and patients have an unusual body habitus. Because cutaneous lesions tend to appear over time, the diagnosis may be delayed until late infancy, childhood, or even adulthood. Orthopedic complications often pose the most challenging medical problems, although vascular complications also contribute to overall morbidity. Severe disfigurement and social stigmatization are additional challenges that must be addressed. [4, 5]
Examples of various malformations and physical symptoms in Proteus syndrome are shown in the images below.
Signs and symptoms of Proteus syndrome
The following are characteristics of Proteus syndrome:
-
When present at birth, asymmetrical limb, digital, or cranial overgrowth may be a major diagnostic finding
-
Digital, limb, or cranial overgrowth usually involves both soft tissue and bone
-
Cranial or external auditory canal hyperostosis may be seen
-
Scoliosis associated with disproportionate vertebral growth is common [6]
-
The combination of disproportionate overgrowth and focal atrophy can lead to a unique habitus characterized by wasting of upper arm muscles, an elongated thorax, an extremely gracile neck, and muscular hypertrophy of the thighs
-
Cystic lung malformations that lead to cystic pulmonary emphysema and restrictive lung disease secondary to severe scoliosis are relatively common; recurrent pneumonias, shortness of breath, or reduced exercise tolerance may point to significant respiratory compromise
-
Organomegaly is less common but can also occur with splenomegaly or occasional thymus enlargement
Cutaneous findings include the following:
-
The six most common skin findings include (from most to least frequent) lipomas, vascular malformations, connective tissue nevi, epidermal nevi, partial lipohypoplasia, and patchy dermal hypoplasia
-
Connective tissue nevi are virtually pathognomonic and typically have a cerebriform contour; they often occur on the soles of the feet but can also be found on other areas
-
Epidermal nevi tend to be the flat, soft variety
-
Lipomas may be well demarcated or locally invasive, with large intra-abdominal or intrathoracic lesions presenting serious medical concerns
-
Vascular lesions may involve capillaries, lymphatics, venules, or combinations of these; port wine stains or patchy hyperpigmentation may also be seen
Facial features that often coincide with poor mental development include the following:
-
Prominent occiput
-
Ptosis with or without down-slanting palpebrae
-
Upturned nose
-
Long narrow face
Workup in Proteus syndrome
Laboratory studies can include the following:
-
AKT1 testing - Should be offered to patients suspected of having Proteus syndrome
-
Punch biopsy of affected tissue - Ideal, but a skin scraping of epidermal nevi has been noted to be effective [7]
-
Platelet studies - May be indicated for patients with numerous vascular malformations or splenomegaly, especially those with a history of easy bruising or petechiae
-
Coagulation workup - May be indicated preoperatively for patients with Proteus syndrome in light of the apparent increased risks for thrombotic events such as deep vein thrombosis (DVT) or pulmonary embolism (PE)
Imaging studies can include the following:
-
Radiography
-
Magnetic resonance imaging (MRI)
-
Computed tomography (CT) scanning
Other tests can include the following:
-
Electroencephalography - Indicated for any patient with a history or symptoms suggesting seizures
-
Pulmonary function tests - May help to evaluate patients with respiratory symptoms
-
Venograms, Doppler studies, or ventilation/perfusion (V/Q) studies - May be helpful diagnostic tools in patients with symptoms suggestive of deep vein thrombosis (DVT) or pulmonary embolism (PE)
Management of Proteus syndrome
Medical care
Early recognition of scoliosis may permit nonsurgical attempts to halt progression.
Aggressive management of thrombosis may be lifesaving in patients who present with calf or leg pain, a palpable cord, and shortness of breath or respiratory distress. Physicians who care for individuals with Proteus syndrome should be made aware of the potential thrombotic risks; hematologic evaluation prior to elective surgery should also be considered. [8]
Surgical care
Surgical intervention may be required for the following:
-
Progressive scoliosis
-
Hemifacial macrosomia or macroglossia - May require surgical intervention if airway obstruction, feeding difficulties, or severe malocclusion is present
-
Large or invasive cutaneous or subcutaneous lesions - While resectable by any competent surgeon, plastic surgical consultation is advisable for cosmetically important areas such as the face
-
Internal lipomas
-
Cystic lung malformations
Patient education
Patients and families can be referred for education and supportive services to the Proteus Syndrome Foundation.
Pathophysiology
A study by Lindhurst et al demonstrated that a somatic mutation in the AKT1 gene, located on chromosome 14q32.3, is causative for Proteus syndrome. The researchers performed exome sequencing of DNA from biopsies of affected tissues and compared this with DNA from normal tissues in these patients. AKT1 mutations were found in the affected tissues but not in the normal tissues. [9]
Proteus syndrome is caused by a somatic mutation rather than a germline one, meaning that only cells descended from the affected cell will display symptoms. This means that individuals with mutations later in development will generally have a less severe phenotype. The random nature of the somatic mutation explains the variability of presentation in patients with Proteus syndrome.
Epidemiology
Frequency
International
Proteus syndrome is believed to be exceedingly rare, with approximately 100 individuals known worldwide. [8] This suggests that the prevalence range of Proteus syndrome is 1:1,000,000 to 1:10,000,000 persons. However, this condition is often misdiagnosed.
Mortality/Morbidity
The following is noted in patients with Proteus syndrome:
-
Hemihyperplasia (asymmetrical overgrowth of the head, face, and digits) and soft tissue overgrowth are among the more significant medical complications. Some scientists have suggested that the bony overgrowth in Proteus syndrome is secondary to mesenchymal changes beginning during embryonic life, with formation of extra-large cartilage precursors. [10]
-
Soft tissue and bone overgrowth may slow after puberty.
-
Absent or decreased subcutaneous fat (lipohypoplasia) of the trunk or limbs may also be seen in patients with Proteus syndrome, contributing to the gracile appearance and well-recognized body habitus in severely affected individuals. [11]
-
Facial involvement may be associated with not only asymmetrical mandibular growth, maxillary growth, or both, but also with premature dental eruption and idiopathic root resorption.
-
Eye findings may include strabismus as well as epibulbar dermoids or cysts; ocular findings are reported in more than 40% of affected individuals. [12]
-
Scoliosis or kyphoscoliosis may be severe and progressive, leading to respiratory compromise in some cases. Neck and trunk elongation with upper body wasting and leg muscle hypertrophy may contribute to overall abnormal body habitus and concomitant functional abnormalities.
-
Although less common, kidney or bladder problems may be identified in slightly less than 10% of affected individuals. Genitourinary problems described include hydronephrosis, renal cysts, asymmetry of the kidneys or bladder, and nephrogenic diabetes. [12]
-
Cutaneous and subcutaneous lesions can create significant cosmetic and functional problems. Benign growths, such as lipomas, connective tissue nevi, epidermal nevi, and vascular malformations, may be locally invasive and contribute greatly to morbidity.
-
Individuals with a larger number of skin manifestations are also more likely to have more severe involvement of other tissues.
-
Whereas ovarian cystadenomas are frequent enough in women with Proteus syndrome to be included as part of the diagnostic criteria, other fairly rare neoplasms have been identified in affected individuals. Meningiomas, various testicular tumors, and parotid monomorphic adenomas have been described. [8] More recently, a patient with Proteus syndrome was shown to have multiple spinal cord meningiomas. [13]
-
Increased risk for thrombotic events such as deep vein thrombosis (DVT) or pulmonary embolism (PE) contribute to the overall morbidity and mortality, even in young children, and is reported to be one of the most common causes of death in affected individuals. [16, 17]
-
Learning disabilities or intellectual disability occur in a subset of patients. A particular facial phenotype often is associated with mental impairment with or without CNS malformations and seizures. Infantile seizures, specifically Ohtahara syndrome, have been described in several patients with Proteus syndrome in association with hemimegalencephaly. [18]
A study by Sapp et al indicated that in individuals with Proteus syndrome, the probability of death by age 22 years is 25%. However, the report also found evidence of a postadolescence moderation of the disease process and resulting reduction in the mortality rate. [19]
Race-, sex-, and age-related demographics
No racial or ethnic differences in disease occurrence are apparent. Classically, males have been thought to be more commonly affected than females, but new studies with genetically confirmed cases have not yet been published. [12]
The genetic mutation that causes Proteus syndrome is a somatic mutation that occurs after conception and is propagated in one or more subsets of embryonic cells. The classic progressive, asymmetrical overgrowth may not be obvious at birth, which can delay diagnosis.
-
Macroglossia and hemifacial overgrowth associated with hyperpigmentation.
-
Port wine stain on the trunk with small epidermal nevus.
-
Macrodactyly with splaying of toes after toe reduction procedure.
-
Ear enlargement associated with cutaneous hyperpigmentation and hemifacial macrosomia.
-
Scoliosis with scar resulting from prior surgical resection of a large subcutaneous lipoma.
-
Evidence of proximal muscle wasting of the upper extremities.
-
Hypertrophy of the thighs and calves.
-
Profile demonstrating retrognathia.