Practice Essentials
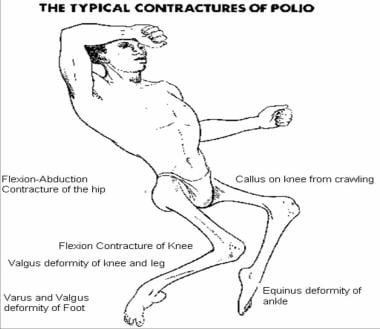
Poliomyelitis is an enteroviral infection that can manifest in 4 different forms: inapparent infection, abortive disease, nonparalytic poliomyelitis, and paralytic disease. Before the 19th century, poliomyelitis occurred sporadically. During the 19th and 20th centuries, epidemic poliomyelitis was more frequently observed, reaching its peak in the mid-1950s. The worldwide prevalence of this infection has decreased significantly since then because of aggressive immunization programs. Eradication of this disease during the present decade is a top priority for the World Health Organization (WHO). [1, 2] See the image below.
Signs and symptoms
The spectrum of disease ranges from inapparent infection to paralytic disease.
In mild cases, the following nonspecific signs and symptoms are observed and usually resolve within a few days:
-
Fever
-
Headache
-
Nausea
-
Vomiting
-
Abdominal pain
-
Oropharyngeal hyperemia
Nonparalytic poliomyelitis is characterized by the symptoms described above in addition to the following:
-
Nuchal rigidity
-
More severe headache
-
Back and lower extremity pain
-
Meningitis with lymphocytic pleocytosis (usually)
Paralytic poliomyelitis is characterized by the following:
-
Localized or widespread compromise of motor neurons
-
Asymmetric loss of muscle function, with involvement of major muscle groups
-
Muscle atrophy
See Presentation for more detail.
Diagnosis
Specimens from the cerebrospinal fluid (CSF), stool, and throat should be obtained for viral cultures in patients with suspected poliomyelitis. Additionally, acute and convalescent serum should be obtained for antibody concentrations against polioviruses.
Magnetic resonance imaging (MRI) can be useful in distinguishing between vaccine-associated paralytic poliomyelitis and other conditions and in assessing the extent of lesions.
See Workup for more detail.
Management
No antivirals are effective against polioviruses. The treatment of poliomyelitis is mainly supportive.
See Treatment and Medication for more detail.
See 11 Travel Diseases to Consider Before and After the Trip, a Critical Images slideshow, to help identify and manage several infectious travel diseases.
For excellent patient education resources, visit eMedicineHealth's Children's Health Center and Brain and Nervous System Center. Also, see eMedicineHealth's patient education articles Immunization Schedule, Children and Brain Infection.
Pathophysiology
Poliovirus is an RNA virus that is transmitted through the oral-fecal route or by ingestion of contaminated water. Three serotypes are able to cause human infection. The incubation period for poliovirus is 5-35 days. The viral particles initially replicate in the nasopharynx and GI tract and then invade lymphoid tissues, with subsequent hematologic spread. After a period of viremia, the virus becomes neurotropic and produces destruction of the motor neurons in the anterior horn and brainstem. The destruction of motor neurons leads to the development of flaccid paralysis, which may be bulbar or spinal in distribution.
Etiology
Polioviruses are enteroviruses within the Picornaviridae family. These viruses are resistant to ether and chloroform but can be inactivated by formaldehyde. They multiply in the GI tract but are particularly neurotropic.
Documentation suggests that infections with polioviruses can be potentiated by factors such as exercise and tonsillectomy. Additionally, patients who are immunocompromised, such as those with human immunodeficiency virus (HIV) infection, B-cell disfunction, immunoglobulin A (IgA) deficiency, or severe combined immunodeficiency, are particularly at high risk of developing poliomyelitis when exposed to both wild-type polioviruses and vaccine-attenuated viruses present in the oral poliovirus vaccine.
Epidemiology
United States statistics
No cases of wild-type poliovirus infection have been reported in the United States since 1979. Until 1998, an average of 8-10 cases associated with the vaccine virus were reported every year. Since the institution of an all-inactivated poliovirus vaccine (IPV) policy in the routine immunization schedule, the number of vaccine-associated cases has significantly decreased. Four cases of vaccine-derived poliovirus were identified in 2005 among unvaccinated children in an Amish community in Minnesota. [3, 4]
In 2022, vaccine-derived poliovirus type 2 infection was confirmed in an unvaccinated immunocompetent adult in New York State, who had been hospitalized with flaccid lower limb weakness. Related type 2 polioviruses were also detected in wastewater samples in two neighboring New York counties. [5]
International statistics
The global incidence of poliovirus infection has decreased by more than 99% since 1988. Although no outbreaks had been reported in the western hemisphere since 1991, the Pan American Health Organization reported an outbreak in Haiti and the Dominican Republic in 2001. Since 2001, no additional outbreaks of disease caused by wild poliovirus have been reported in the Americas. Clusters of wild-type disease are still found in some areas in Africa and Southeast Asia.
Significant progress has been made towards poliomyelitis eradication in India, which is considered a nonendemic area. [6, 7] Pakistan, Afghanistan, and Nigeria are 4 countries in which indigenous transmission of wild poliovirus still occurs. However, importation of wild poliovirus into countries previously considered free of poliomyelitis continues to be a problem, especially in Africa. [8, 9] In addition, there have been confirmed cases of poliomyelitis in Syria and Iraq caused by wild poliovirus type 1 (WPV1). [10]
Concern for importation of cases from Afghanistan and Pakistan into Israel has resulted in a change in their routine polio immunization to include at least one dose of oral vaccine. In 2014, India began requiring a dose of oral polio vaccine for anyone coming from countries where polio is still seen, particularly Afghanistan and Pakistan. [11]
Wild poliovirus type 2 (WPV2) was officially eradicated in 2015, which prompted the replacement of trivalent oral poliovirus vaccine with OPV containing only types 1 and 3. [12]
In 2017, the WHO confirmed two separate outbreaks of polio in the Democratic Republic of Congo as well as an outbreak in Syria. [13, 14]
In 2022, a case of wild poliovirus type 1 infection was confirmed in a 3-year-old girl in Lilongwe, Malawi. According to the WHO, it was the first case in Africa in 5 years. [15] The strain of poliovirus that infected the child was closely related to a strain detected in a sewage sample from Pakistan. [16]
Sex- and age-related demographics
Males and females of pediatric age are affected with equal frequency.
Poliovirus affects mainly children. However, individuals of any age (especially those who are immunocompromised) may also develop the disease.
Prognosis
Bulbar paralytic poliomyelitis has been associated with the highest rate of complications and a mortality rate as high as 60%; spinal poliomyelitis follows. Patients with inapparent or abortive poliomyelitis recover without significant sequelae.
Morbidity/mortality
Mortality is more frequently observed in cases of paralytic poliomyelitis and is associated with complications such as respiratory failure. No deaths due to wild-type poliovirus have been reported in the United States since 1979.
Although most cases of poliomyelitis (90-95%) are inapparent, 5-10% of patients who acquire this infection develop symptoms.
-
The typical contractures of postpolio residual paralysis.