Practice Essentials
Obstructive sleep apnea (OSA) in children is characterized by episodic upper airway obstruction that occurs during sleep. The airway obstruction may be complete or partial.
Signs and symptoms
The clinical presentation of a child with obstructive sleep apnea (OSA) is nonspecific and requires increased awareness by the primary care physician. OSA symptoms in children can include the following:
-
Abnormal breathing during sleep
-
Frequent awakenings or restlessness
-
Frequent nightmares
-
Enuresis
-
Difficulty awakening
-
Excessive daytime sleepiness
-
Hyperactivity/behavior problems
-
Daytime mouth breathing
-
Poor or irregular sleep patterns
Complications of OSA in children can generally be divided into the 4 following immediate consequences of upper airway obstruction during sleep:
-
Sleep fragmentation
-
Increased work of breathing
-
Alveolar hypoventilation
-
Intermittent hypoxemia
See Clinical Presentation for more detail.
Diagnosis
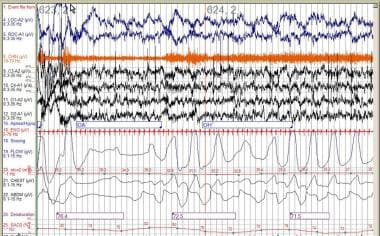
Currently, the only available tool for definitive diagnosis of OSA is an overnight polysomnographic evaluation in the sleep laboratory (see the image below). Ideally, polysomnography should be performed overnight and during the patient's usual bedtime.
Polysomnography provides the following measures:
-
Sleep state (≥2 EEG leads)
-
Electrooculogram (right and left)
-
Submental electromyelogram (EMG)
-
Airflow at nose and mouth (thermistor, capnography, or mask and pneumotachygraph)
-
Chest and abdominal wall motion (impedance or inductance plethysmography)
-
Electrocardiogram (preferably with R-R interval derivation technology)
-
Pulse oximetry (including a pulse waveform channel)
-
End-tidal carbon dioxide (sidestream or mainstream infrared sensor)
-
Video camera monitor with sound montage (analog or digital)
-
Transcutaneous oxygen and carbon dioxide tensions (in infants and children < 8 y)
Polysomnographic normal standards differ between children and adults. In the pediatric age range, abnormalities include oxygen desaturation under 92%, more than one obstructive apnea per hour, and elevations of ET CO2 measurements of more than 50 mm Hg for more than 9% of sleep time or a peak level of greater than 53 mm Hg.
See Workup for more detail.
Management
Surgical intervention
Although OSA has multiple etiologies in children, once the diagnosis has been established and its severity assessed, adenotonsillectomy is usually the first line of treatment. Tonsillotomy, rather than tonsillectomy, has been recently advocated as equally effective with less postoperative morbidity.
Adenotonsillectomy should be implemented along with weight normalization in obese children. Caloric intake limitation and dietary counseling are necessary if obesity complicates OSA. Children and adolescents with significant sleep apnea should avoid eating large amounts just before bedtime.
Continuous positive airway pressure
CPAP is the mainstay of therapy for most adults with OSA, as well as a large number of children and adolescents. However, it is often difficult for children to adhere to the therapy regimen.
CPAP devices can be uncomfortable and inappropriately fitting masks can leak, leading to the development of pressure sores on the bridge of the nose. Air leaks can also irritate the conjunctiva, causing increased lacrimation and eye discomfort. Also, midfacial hypoplasia may develop with long-term use, particularly in children with neuromuscular weakness.
See Treatment and Medication for more detail.
Background
Childhood obstructive sleep apnea (OSA) syndrome is characterized by episodic upper airway obstruction that occurs during sleep. The airway obstruction may be complete or partial. Three major components of obstructive sleep apnea have been identified: episodic hypoxia, intermittent hypercapnia, and sleep fragmentation. Habitual snoring without obstructive sleep apnea is more common and may also lead to sleep fragmentation. Both primary snoring and obstructive sleep apnea have been associated with poor quality of life and increased health care use in children.
Obstructive sleep apnea syndrome was described more than a century ago, but obstructive sleep apnea in children was first described in the 1970s. It is a common but underdiagnosed condition in children that may ultimately lead to substantial morbidity if left untreated.
The mechanisms of obstruction, adverse effects of obstructive sleep apnea, diagnostic criteria, and recommended treatment options are different in children from those in adults (see the image below). Important recent advances in the understanding of the underlying pathophysiological mechanisms of obstructive sleep apnea in children have been coupled with improved approaches to the diagnosis and management of obstructive sleep apnea.
Go to Obstructive Sleep Apnea for complete information on this topic.
Pathophysiology
Disordered breathing during sleep is a hallmark of obstructive sleep apnea syndrome. Breathing abnormalities include apnea (cessation of air flow) and hypopnea (decreased air flow). In addition, in contrast to adults, some children exhibit a variation of obstructive sleep apnea termed obstructive hypoventilation (OH). Children with obstructive hypoventilation demonstrate periods of hypercapnia that occur in the absence of discrete respiratory events that fulfill the criteria for apnea or hypopnea.
Apneas and hypopneas
Physiologic recording methods can differentiate the types of apnea. During obstructive apnea, an individual makes respiratory efforts, but no airflow occurs because of upper airway obstruction. Central apnea is an interruption in both airflow and breathing effort. Mixed apneas have both central and obstructive components. A typical mixed event begins with a central apnea, which is followed immediately by one or more obstructed breaths.
Hypopneas are episodes of shallow breathing during which airflow is decreased by at least 50%. They are usually accompanied by some degree of oxygen desaturation, which can be minor and transient. Like apnea, hypopnea is subdivided into obstructive, central, and mixed. Obstructive hypopneas are episodes of partial upper airway obstruction. Respiratory efforts occur, but airflow is reduced. In central hypopnea, breathing effort and airflow are both decreased. Mixed hypopneas have both central and obstructive components.
In adults, episodes of disordered breathing must last 10 seconds or more before being considered an apnea or hypopnea. Normal resting respiratory rates in children are faster than those in adults, and children have a smaller functional residual capacity and a more compliant chest wall. As a result, children undergo oxygen desaturation more rapidly than adults whenever airflow is interrupted. A definition of apnea or hypopnea requiring that an event last 10 seconds or more before being considered significant is somewhat arbitrary and does not take into account the physiologic differences between adults and children. Consequently, pediatric sleep centers use different duration criteria for labeling events such as apnea or hypopnea. In children, if obstruction occurs with 2 or more consecutive breaths, the event can be called an apnea or hypopnea, even if it lasts less than 10 seconds.
Upper airway obstruction
The ability to maintain upper airway patency during the normal respiratory cycle is the result of a delicate equilibrium between the forces that promote airway closure and dilation. This "balance of forces" concept was initially proposed by 2 independent groups and reflects the current line of thought regarding the underlying pathophysiological mechanisms that result in the clinical spectrum of obstructive apnea.
The 4 major predisposing factors for upper airway obstruction are the following:
-
Anatomic narrowing
-
Abnormal mechanical linkage between airway dilating muscles and airway walls
-
Muscle weakness
-
Abnormal neural regulation
Obstructive apnea and hypopnea are related to upper airway obstruction. Upper airway obstruction may occur at one or more levels, including the nasopharynx (area from the nose to the hard palate), mouth, velopharynx (space behind the palate), retroglossal region (area behind the tongue), hypopharynx (region between the tongue base and larynx), and larynx.
The upper airway is a pliant tube whose sidewalls consist of muscle and other soft tissues. During wakefulness, neural input to a number of small muscle groups in the pharynx maintains muscle tone and airway patency. With sleep, an increased resistance to airflow normally accompanies muscular relaxation of these muscle groups. Although most people compensate for these changes, individuals with certain anatomic problems have repeated episodes of partial or complete upper airway obstruction when they sleep.
Childhood sleep apnea differs from adult obstructive sleep apnea in that adults with sleep apnea frequently present with hypersomnia, whereas children often demonstrate short attention spans, emotional lability, and behavioral problems. Obesity is a major risk factor in both adults and children. [1] Fatty infiltration of the pharyngeal soft tissues narrows the caliber of the upper airway and contributes to airway resistance. Although obesity plays a role in some cases of childhood sleep apnea, the airway obstruction is usually related to tonsillar hypertrophy, adenoid hypertrophy, or craniofacial abnormalities. Children with some types of neuromuscular disease (eg, Duchenne muscular dystrophy, spinal muscular atrophy, cerebral palsy) may also have a higher risk of developing sleep apnea.
Anatomic narrowing
At any point in life, a smaller cross-sectional area of the upper airway is associated with decreased ability to maintain upper airway patency. In adults, the upper airway behaves as predicted by the Starling resistor model. According to this model, under conditions of flow limitation, maximal inspiratory flow is determined by the pressure changes upstream (nasal) to a collapsible site of the upper airway, and flow is independent of downstream (tracheal) pressure generated by the diaphragm. Pressures at which the airway collapses have been termed critical closing pressures, or Pcrit. In other words, in the presence of a collapsible segment of the upper airway, such as the pharyngeal introitus, the overall resistance to airflow proximal to that segment is the major factor responsible for occlusion of the collapsible segment. This model explains why, for example, snoring and obstructive apnea worsen during a common cold (increased nasal-upstream resistance).
The validity of this model was also confirmed in children, and interestingly, the collapsibility of the upper airway in children was reduced when compared with that of adults. As predicted by the Starling resistor model, the collapsible segment of the upper airway in children displayed less negative (higher and, therefore, more collapsible) pressures in children with obstructive sleep apnea. Components that affect the upstream segment pressures or increase Pcrit are of major consequence to the ability to maintain airway patency. For example, a viral cold or allergic rhinitis that induces increased secretion in the nasal passages and mucosal swelling is associated with increased nasal resistance to airflow. Not surprisingly, the magnitude of snoring and the severity of obstructive apnea are increased during periods in which the upstream segment pressure has been adversely affected.
The contribution of the various anatomical nasopharyngeal structures to Pcrit and the interactions between these structures that lead to upper airway patency or obstruction during sleep are of obvious importance in increasing the understanding of the pathophysiology of obstructive sleep apnea in children. For most children, enlargement of the tonsils and/or adenoid is the proximate cause for the development of obstructive sleep apnea.
The static pressure and/or area relationships of the passive pharynx were endoscopically measured in 14 children with obstructive sleep apnea and in 13 healthy children under general anesthesia with complete paralysis, [2] and it was determined that children with obstructive sleep apnea closed their airways at the level of enlarged adenoids and tonsils at low positive pressures, whereas healthy children required subatmospheric pressures to induce upper airway closure. The cross-sectional area of the narrowest segment was significantly smaller in children with obstructive sleep apnea and particularly involved the retropalatal and retroglossal segments. Thus, both congenital and acquired anatomic factors clearly play a significant role in the pathogenesis of pediatric obstructive sleep apnea.
Abnormal mechanical linkage between airway dilating muscles and airway walls
Malposition or malinsertion of specific dilating muscles is likely to have major consequences on the mechanical dilating efficiency. Therefore, even if a major weakness is not present, the mechanical disadvantage imposed by muscle shortening or by displacement of the muscle insertion on the pharyngeal wall undoubtedly results in diminished ability to stiffen the airway, thus leading to increased collapsibility or elevation of Pcrit.
Control of the upper airway size and stiffness depends on the relative and rhythmic contraction of a host of paired muscles, which include the palatal, pterygoid, tensor palatini, genioglossus, geniohyoid, and sternohyoid muscles. These muscles tend to promote a patent pharyngeal lumen and receive phasic activation in synchrony with phrenic nerve activation. Upon contraction, these muscles promote motion of the soft palate, mandible, tongue, and hyoid bone. Although the coordinated action of these muscles during the respiratory cycle has yet to be deciphered, a reasonable generalization is that inspiratory muscle output stiffens the pharynx and related structures and enlarges the lumen.
The optimal activity of these muscles depends on their anatomic arrangement; for example, airway patency is compromised during increased neck flexion by changing the points of attachment of muscles acting on the hyoid bone, such that the resulting vector of their forces may be nullified. The activity of pharyngeal muscles greatly depends on various factors within the CNS and, more particularly, on the brainstem respiratory network. Wakefulness conveys a supervisory function that ensures airway patency, and sedative agents, which compromise genioglossal muscle activity, may result in significant upper airway compromise.
Mechanoreceptor-mediated and chemoreceptor-mediated genioglossal activity is critical for maintenance of upper airway patency in healthy and micrognathic infants. Changes in genioglossal activity during transitions, from oral to nasal breathing and relative to Pcrit, suggest that genioglossus activation is critical for airway patency in micrognathic infants.
Muscle weakness
Little evidence suggests that intrinsic muscle weakness is a major contributor to upper airway dysfunction in conditions other than those associated with neuromuscular disorders. However, in neuromuscular disorders, upper airway obstruction is frequently observed during sleep, further reinforcing the validity of the balance-of-pressures concept.
Abnormal neural regulation
Abnormal respiratory control does not appear to play a significant role in upper airway obstruction during sleep in children with obstructive sleep apnea. In one study, the ventilatory response to hyperoxic hypercapnic challenge in children and adolescents with obstructive sleep apnea was similar to that measured in age-matched and sex-matched controls. [3] Similarly, no differences were found in the ventilatory response to isocapnic hypoxia. Blunting in central chemosensitivity was reported in some children with obstructive sleep apnea undergoing surgery; however, despite such reports, central chemosensitivity during sleep in children with obstructive sleep apnea was similar to that in matched controls. However, arousal to hypercapnia was blunted, suggesting that subtle alterations in the central chemosensitive arousal network may have occurred in these children.
These subtle changes have been further substantiated by examining the ventilatory response to repeated hypercapnia, whereby reciprocal changes in respiratory frequency and tidal volume occur. In addition, children with obstructive sleep apnea demonstrate impaired arousal responses to inspiratory loads during rapid eye movement (REM) and non-REM sleep, compared to controls. Neural responses to hypoxia and hypercapnia have not been well studied in children with obstructive sleep apnea and underlying syndromes.
In addition to the aforementioned considerations, diminished laryngeal reflexes to mechanoreceptor and chemoreceptor stimulation, with reduced afferent inputs into central neural regions underlying inspiratory inputs, can be present. For example, chemoreceptor stimuli, such as increased PaCO2 or decreased PaO2, stimulate the airway, dilating muscles in a preferential mode (ie, upper airway musculature is more stimulated than the diaphragm).
This preferential recruitment tends to correct an imbalance of forces acting on the airway and, therefore, maintains airway patency. Similarly, stimuli that result from suction pressures in the nose, pharynx, or larynx rapidly stimulate the activity of upper airway dilators. This effect is also preferential to the upper airway, causing some degree of diaphragmatic inhibition and, thus, compensating for increases in upstream resistance. The function of these upper airway receptors in children with adenotonsillar hypertrophy with and without obstructive sleep apnea is not known.
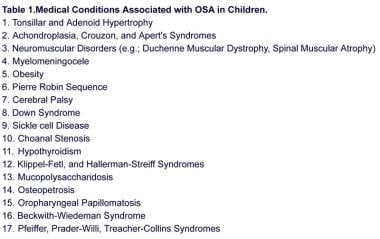
Etiology
Obesity and hypertrophy of tonsils and/or adenoids account for most cases of obstructive sleep apnea in children. [1] However, any anomaly of the upper airway may produce intermittent obstructive symptoms during sleep. Facial, oral, and throat eccentricities occur in numerous congenital syndromes. Certain storage diseases, hypothyroidism, and Down syndrome result in upper airway crowding due to a relative increase in tongue mass compared to mouth size.
Neuromuscular diseases contribute to obstructive sleep apnea because of abnormal muscle tone in the pharyngeal constrictors, which are responsible for maintaining airway patency. Children with Chiari malformations are usually not weak but may develop obstructive apnea due to dysfunction of the same pharyngeal muscle groups. Individuals with obesity typically have fatty infiltration of the soft tissues of the throat, limiting airway caliber and predisposing them to obstructive apnea. Persons with sickle cell anemia have a tendency toward obstructive apnea for reasons that are still unclear.
Disorders associated with childhood obstructive sleep apnea include, but are not limited to, the following:
-
Adenotonsillar hypertrophy, which is the most common cause of obstructive sleep apnea in children (however, the size of the tonsils and adenoids alone does not predict the presence or severity of obstructive sleep apnea)
-
Chronic nasal obstruction, including choanal stenosis, severe septal deviation, allergic rhinitis, nasal polyps, and rare nasal and/or pharyngeal tumors
-
Down syndrome
-
Pierre Robin anomaly
-
Treacher Collins syndrome
-
Klippel-Feil syndrome
-
Morbid obesity
-
Mucopolysaccharidoses
-
Conditions involving neuromuscular weakness, including Duchenne muscular dystrophy, Werdnig-Hoffman disease, late-onset spinal muscular atrophy, Guillain Barré syndrome, myotonic dystrophy, and myotubular myopathy
-
Chiari malformation
-
Cerebral palsy
-
Hallermann-Streiff syndrome
-
Osteopetrosis
-
Oropharyngeal papillomatosis
Epidemiology
In nonobese and otherwise healthy children younger than 8 years, the prevalence of obstructive sleep apnea is estimated to be 1-3%. Habitual snoring is common during childhood and affects approximately 10% of children aged 2-8 years; the frequency decreases after age 9-10 years. Obesity confers 4-fold to 5-fold added risk for sleep-disordered breathing. In children and adolescents with coexisting medical conditions such as trisomy 21, the prevalence of obstructive sleep apnea may be as high as 80%. [4]
In the United Kingdom, approximately 1.75-2.25% of children aged 4-5 years are thought to have obstructive sleep apnea. Unfortunately, very few epidemiologic studies of childhood obstructive sleep apnea are available.
Racial distribution
Obstructive sleep apnea occurs more commonly among Black and Hispanic individuals than among White adults and children. In patients younger than 18 years, Blacks are 3.5 times more likely to develop obstructive sleep apnea than Whites.
The high frequency of obstructive sleep apnea in adult Asian populations indicates that the anthropometric characteristics of the craniofacial structures in this racial group also predispose to higher obstructive sleep apnea rates in children. The frequency of obstructive sleep apnea in Hispanic children is equal to that of White children.
Sex distribution
The male-to-female ratio of obstructive sleep apnea in children is approximately 1:1. At puberty, the male-to-female ratio starts to increase. In older adolescents, a male preponderance emerges that essentially reflects the typical male predominance observed in the adult population. By adulthood, symptomatic men outnumber symptomatic women by 2:1 or more.
Age distribution
Obstructive sleep apnea is observed in children of all ages and may develop even in infancy. Retrospective studies note that a large number of parents with children in whom obstructive sleep apnea is diagnosed recall that their child's snoring began within the first months of life. Preterm babies are at risk for more obstructive events while supine, but some have suggested that they are still at a lower risk of death from sudden infant death syndrome. However, Moon et al, citing 3 studies, report that premature infants may be at 4 times increased risk for sudden infant death syndrome compared with term infants, with the risk increasing at lower gestational age and birthweight. [5]
Most children with obstructive sleep apnea are aged 2-10 years (coinciding with adenotonsillar lymphatic tissue growth). Children with severe obstructive apnea are likely to present when aged 3-5 years. The mean age at diagnosis has been reported to be 14 months, plus or minus 12 months.
Prognosis
Major morbidities associated with childhood obstructive sleep apnea include failure to thrive, difficulty concentrating and/or developmental delay, behavioral problems, hypertension, pulmonary hypertension, and, ultimately, cor pulmonale. Some pulmonologists theorize that chronic upper airway obstruction with labored breathing may result in the development of a pectus excavatum deformation in a compliant immature chest wall. Concomitant gastroesophageal reflux is likely to be exacerbated by obstructive sleep apnea.
Children with obstructive sleep apnea syndrome, as well as children with a history of loud habitual snoring, appear to be at risk for developing deficits of executive function. According to the model by Beebe and Gozal, sleep fragmentation, intermittent hypoxemia, and hypercapnia contribute to dysfunction in the prefrontal areas of the brain. [6] Executive functions include behavioral inhibition, regulation of affect and arousal, ability to analyze and synthesize, and memory. Executive dysfunction interferes with cognitive abilities and learning.
Obesity-related hypoventilation, commonly known as the pickwickian syndrome, occurs in some children who have obesity and obstructive sleep apnea. These individuals respond abnormally to both hypercapnic and hypoxemic stimuli to breathe; they have repetitive obstructive events with sleep and marked daytime sleepiness, daytime hypoventilation, and hypercapnia.
The incidence of cor pulmonale and death due to obstructive sleep apnea is unknown. Once pulmonary hypertension has developed, it is usually reversible if the underlying obstructive sleep apnea is effectively treated.
Children with severe obstructive sleep apnea may develop postobstructive pulmonary edema within a few hours of surgery undertaken to relieve upper airway obstruction. Furthermore, such patients are at risk for postoperative respiratory compromise, which is characterized by severe upper airway obstruction and may require endotracheal intubation or the use of noninvasive respiratory support such as continuous positive airway pressure via a nasal mask.
Prognosis after surgery
Surgical treatment of severe obstructive sleep apnea warrants an overnight observation, especially if the child is younger than 3 years or has concomitant cardiopulmonary disease, morbid obesity, hypotonia, or craniofacial anomalies.
The major determinants of surgical outcome include the apnea hypopnea index (AHI) and obesity at the time of diagnosis. The AHI is the total number of apneas and hypopneas that occur divided by the total duration of sleep in hours. An AHI of 1 or less is considered to be normal by pediatric standards. An AHI of 1-5 is very mildly increased, 5-10 is mildly increased, 10-20 is moderately increased, and greater than 20 is severely abnormal.
In children with enlarged tonsils and adenoids that lead to obstructive sleep apnea, an adenotonsillectomy usually results in complete cure, although no definitive studies have clearly demonstrated this issue.
The outcome of patients who require extensive surgical management obviously depends on the severity of the condition that leads to upper airway compromise. With the emergence of noninvasive ventilation as an alternative option for these children, upper airway obstruction during sleep can be conservatively and successfully managed in most children.
In children with failure to thrive (FTT), treatment of obstructive sleep apnea leads to resolution of the somatic growth disturbance. Similarly, pulmonary hypertension resolves. Although major improvements in neurobehavioral outcomes are expected, data are currently insufficient to support a complete recovery in some of the cognitive abilities affected by obstructive sleep apnea.
Tauman et al reported that only 25% of children treated for obstructive sleep apnea with adenotonsillectomy had complete postoperative normalization of symptoms. [7]
Patient Education
Patients receiving continuous positive airway pressure (CPAP) therapy for obstructive sleep apnea must understand that they need to use their machines every night and each time they nap.
Educate families of children and adolescents who have obesity and obstructive apnea about nutrition and weight loss.
Obesity is increasing in children; 16-33% of children and adolescents are obese. Primary care providers should provide basic weight loss information and support and readily refer patients to a pediatric weight loss program. A pediatric sleep disorders clinic should work closely with a weight loss program and can be a portal of entry for a patient into such care systems.
Compliance issues are of particular importance in patients treated with noninvasive ventilation. Weight loss through an appropriate program of diet and exercise is clearly beneficial for patients with obstructive sleep apnea who are obese.
Avoidance of certain drugs and alcohol
Patients should avoid alcohol and other depressant recreational drugs, which may worsen their sleep apnea. They should avoid sedating medications when possible; if necessary appropriate monitoring and medical supervision is required.
Infants and children with obstructive sleep apnea may have serious respiratory embarrassment when given any sedative medication. Caution is necessary during any medical or dental procedures requiring conscious sedation.
-
Palate appearance following uvulopalatopharyngoplasty (UPPP) surgery.
-
Example of an obstructive apnea and an obstructive hypopnea recorded during polysomnography.
-
Medical complications associated with obstructive sleep apnea in children.
-
Compressed overnight polysomnography tracing of a 6-year-old boy who snores, showing multiple events of obstructive apnea (green-shaded areas) associated with oxyhemoglobin desaturation (yellow-shaded areas) and EEG arousals (red-shaded areas).
-
Parameters monitored during an overnight pediatric sleep study.
-
Normal parameters for sleep gas exchange and gas exchange in children.
Tables
What would you like to print?
- Overview
- Presentation
- DDx
- Workup
- Approach Considerations
- Polysomnography
- Apnea Hypopnea Index
- Daytime Nap Studies
- Overnight Oximetry
- Anteroposterior and Lateral Neck Radiography
- Cine MRI
- Thyroid-Stimulating Hormone and Thyroxine
- Electrocardiography and Echocardiography
- Multiple Sleep Latency Test (MSLT)
- MRI of the Brain and Brainstem
- Other Studies
- Emerging Studies
- Show All
- Treatment
- Medication
- Questions & Answers
- Media Gallery
- References