Practice Essentials
Löffler syndrome is a transient respiratory illness associated with blood eosinophilia and radiographic shadowing. (See the image below.) It was initially described by Löffler in 1932. In 1952, Crofton included Löffler syndrome as one of the 5 categories for conditions that cause pulmonary infiltrates with eosinophilia. The original description of Löffler syndrome listed parasitic infection with Ascaris lumbricoides as its most common cause; however, other parasitic infections and acute hypersensitivity reactions to drugs are included as etiologies for simple pulmonary eosinophilia.
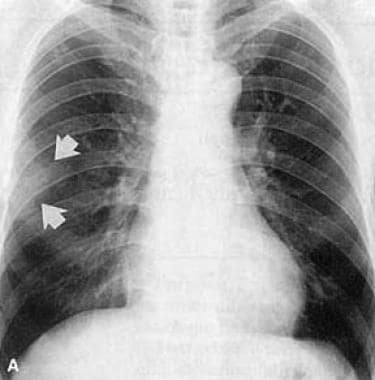 Initial chest radiograph of a 54-year-old man showing subtle opacity (arrows) in the right middle lung zone.
Initial chest radiograph of a 54-year-old man showing subtle opacity (arrows) in the right middle lung zone.
Signs and symptoms
Symptoms of Löffler syndrome are usually mild or absent and tend to spontaneously resolve after several days or, at most, after 2-3 weeks. Cough is the most common symptom among symptomatic patients.
See Presentation for more detail.
Diagnosis
Laboratory studies
The following studies are indicated in Löffler syndrome:
-
Complete blood cell (CBC) count with differential
-
Stool examination
-
Immunoglobulin E (IgE) level
-
Analysis of sputum or gastric lavages
-
Bronchoalveolar lavage
Imaging studies
The following studies may be included in the workup:
-
Chest radiography
-
Chest computed tomography (CT) scanning
See Workup for more detail.
Management
The minimal nature of symptoms in most patients with Löffler syndrome usually denotes that no pharmacologic therapy is required for this self-limiting condition. Surgical care is not indicated.
See Treatment and Medication for more detail.
Pathophysiology
Löffler syndrome has classically been related to the transit of parasitic organisms through the lungs during their life cycle in the human host. After ingestion of Ascaris lumbricoides eggs, larvae hatch in the intestine and penetrate the mesenteric lymphatics and venules to enter the pulmonary circulation. They lodge in the pulmonary capillaries and continue the cycle by migrating through the alveolar walls. Finally, they move up the bronchial tree and are swallowed, returning to the intestine and maturing into adult forms. This process takes approximately 10-16 days after ingestion of the eggs. Other parasites, such as Necator americanus, Ancylostoma duodenale, and Strongyloides stercoralis, have a similar cycle to Ascaris, with passage of larval forms through the alveolar walls. These parasites are not orally ingested but enter the human host through the skin.
A review of the parasitic infections of the lung provides an excellent guide for the pulmonary physician. [1]
Researchers initially thought that transit of parasitic forms through the lung was cardinal in the pathogenesis of Löffler syndrome; however, pulmonary eosinophilia has been described in association with parasites whose life cycle does not include passage through the alveoli and also in association with an increasing number of medications. Additionally, eosinophilic pulmonary infiltrates have appeared in mice challenged with a transnasal Ascaris extract. In these situations, accumulation of eosinophils in the lungs is likely secondary to immunologic hyperresponsiveness. The exact immunopathogenic mechanism for this reaction remains unknown.
Animal models demonstrated that development of pulmonary eosinophilia is T cell–dependent because challenged athymic mice do not develop pulmonary eosinophilia. Production of cytokines such as interleukin-5 (IL-5) is necessary for development of pulmonary eosinophilia. Recent data suggest that circulating, but not local, lung IL-5 is critically required for the development of antigen-induced pulmonary eosinophilia.
Etiology
Most cases of simple pulmonary eosinophilia are caused by parasitic infections or drugs; however, no cause is identified in one third of patients.
Parasites that can cause pulmonary eosinophilia include the following:
-
Ascaris lumbricoides (the most common parasitic etiology)
-
Ascaris suum
-
Necator americanus
-
Strongyloides stercoralis
-
Ancylostoma braziliense
-
Ancylostoma caninum
-
Ancylostoma duodenale
-
Toxocara canis
-
Toxocara cati
-
Entamoeba histolytica
-
Fasciola hepatica
-
Dirofilaria immitis
-
Clonorchis sinensis
-
Paragonimus westermani
Agents in drug-induced eosinophilia include the following:
-
Antimicrobials - Dapsone, ethambutol, isoniazid, nitrofurantoin, penicillins, tetracyclines, clarithromycin, pyrimethamine, daptomycin [2]
-
Anticonvulsants - Carbamazepines, phenytoin, valproic acid, ethambutol
-
Anti-inflammatories and immunomodulators - Aspirin, azathioprine, beclomethasone, cromolyn, gold, methotrexate, naproxen, diclofenac, fenbufen, ibuprofen, phenylbutazone, piroxicam, tolfenamic acid
-
Other agents - Bleomycin, captopril, chlorpromazine, granulocyte-macrophage colony-stimulating factor, imipramine, methylphenidate, sulfasalazine, sulfonamides
Epidemiology
United States statistics
Intestinal helminthiases associated with Löffler syndrome, such as ascariasis, have a reported prevalence of 20-67% among children in rural southern communities. No specific statistics have been reported for the occurrence of Löffler syndrome. Because of widespread globalization, immigration, and travel, US physicians may now more commonly encounter imported tropical diseases that may present with Löffler syndrome.
International statistics
Intestinal helminthiases associated with Löffler syndrome are distributed worldwide; however, they are more prevalent in tropical climates, especially in communities with poor sanitary conditions.
Age-related demographics
Because young children are exposed to contaminated soil and exhibit hand-to-mouth behavior more often than adults, they have a higher incidence of intestinal helminthiases and Löffler syndrome.
Prognosis
Prognosis is excellent.
Morbidity/mortality
No deaths due to Löffler syndrome have been reported. Löffler syndrome is considered a benign, self-limiting disease without significant morbidity. Symptoms usually subside within 3-4 weeks or shortly after the offending medication is withdrawn in drug-induced pulmonary eosinophilia.
Complications
A case report describes hypereosinophilic syndrome with isolated Loeffler endocarditis, which resolved completely after 2 months of corticosteroid therapy. [3]
Patient Education
Sanitary practice
Educate people about sanitary disposal of feces, associated with educational campaigns for the use of latrines and pit privies in rural communities.
Promote good handwashing technique to avoid ingestion of parasitic forms from contaminated soil.
Prevention
In endemic areas of ancylostomiasis and strongyloidiasis, encourage use of proper footwear to avoid skin penetration of larvae of N americanus, A duodenale, or S stercoralis.
Avoid future use of the offending medication in patients with drug-induced pulmonary eosinophilia.
-
Initial chest radiograph of a 54-year-old man showing subtle opacity (arrows) in the right middle lung zone.
-
Follow-up chest radiograph of a 54-year-old man showing migrating opacity in the left lower lobe (arrows) obtained 20 days after the previous image.
-
High-resolution CT scan (1 mm collimation) obtained in a 54-year-old man showing consolidation with surrounding ground-glass opacity in the left lower lobe. Dilated airways are observed within the lesion. This CT scan was obtained between the first and second images above.





