Practice Essentials
Hypochloremic alkalosis results from either low chloride intake or excessive chloride wasting. Whereas low chloride intake is very uncommon, excessive chloride wasting often occurs in hospitalized children, usually as a result of diuretic therapy or nasogastric tube suctioning. Diarrhea, when watery (see the image below), is highly suggestive of chloride-losing diarrhea.
 Watery stool from an infant with congenital chloride-losing diarrhea. Chloride level was 205 mmol/L.
Watery stool from an infant with congenital chloride-losing diarrhea. Chloride level was 205 mmol/L.
Signs and symptoms
Hypochloremia itself often has no signs or symptoms. Instead, associated signs and symptoms result from electrolyte imbalance or underlying causes of the hypochloremia.
Symptoms that may be noted in fetuses and neonates include the following:
-
Prenatal polyhydramnios
-
Lack of meconium or delayed meconium
-
Abdominal distension of unknown etiology
-
Prolonged neonatal jaundice
-
Hypotonia and lethargy without sepsis
Symptoms that may be noted in infants include the following:
-
Repeated vomiting
-
Failure to thrive
-
Constipation
-
Watery diarrhea
-
Polyuria
-
Salty taste upon being kissed
-
Central nervous system (CNS) dysfunctions (eg, lethargy, confusion, or seizure)
-
Neuromuscular symptoms (eg, weakness and muscle cramps)
-
Other symptoms (eg, abdominal distention, dry skin, apathy, loss of interests, and frequent hospital admissions for recurrent dehydration)
General physical findings may include the following:
-
Small size for age
-
Signs of chronic dehydration (eg, skin tenting and poor peripheral perfusion)
CNS manifestations may include the following:
-
Confusion
-
Apathy
-
Disorientation
-
Excessive sleeping
-
Seizure
-
Stupor
Abdominal manifestations may include the following:
-
Scaphoid or distended abdomen (depending on the cause of the hypochloremic alkalosis)
-
Peristaltic waves in children with chloride-losing diarrhea (CLD)
-
Exacerbated bowel sounds in patients with CLD
-
Hard stools in patients with Bartter syndrome
-
Hepatomegaly (suggesting cystic fibrosis)
Musculoskeletal findings include muscle wasting, atrophy, and hypotonia. Respiratory findings include shallow breathing and hypopnea in severely affected children.
See Presentation for more detail.
Diagnosis
Laboratory studies that may be helpful include the following:
-
Amniocentesis
-
Blood workup - Serum electrolyte levels; pH; serum bicarbonate, uric acid, hemoglobin, renin, and aldosterone levels
-
Urine and stool studies - Urine chloride, sodium, and potassium concentrations; urine calcium-to-creatinine and uric acid–to–creatinine ratios; stool electrolytes (when measurable)
-
Kidney and liver function tests
-
Genetic studies
Ultrasonography may be useful for the following purposes:
-
Prenatal - Detection of minimal prenatal polyhydramnios and assessment of intestinal fluid content
-
Postnatal - Evaluation of a fluid-filled bowel, renal echogenicity, nephrocalcinosis, medullary or diffuse calcinosis, and renal growth
Physiologic study of renal tubules by performing maximal free water clearance during hypotonic saline diuresis is indicated.
Additional studies that may be considered include the following:
-
Wrist radiography
-
Upper gastrointestinal (GI) series
-
Computed tomography (CT) of the brain
-
Magnetic resonance imaging (MRI) of the brain
-
Electroencephalography (EEG)
-
Renal nuclear scanning
-
Renal biopsy
See Workup for more detail.
Management
Replacement of electrolytes with chloride salts is the most important mode of therapy. Nonsteroidal anti-inflammatory drugs (NSAIDs) are used in patients with Bartter syndrome. Hydrochloric acid and carbonic anhydrase inhibitors may be used in some acute situations.
Initial management (≤6 hours) includes the following:
-
Assessment of dehydration status and severity of hypochloremia, hypokalemia, hyponatremia, and metabolic alkalosis
-
In cases of shock, aggressive resuscitation with isotonic fluid, preferably normal saline
-
Drawing of blood and urine samples for testing of electrolytes
Maintenance therapy (7-72 hours) depends on how much improvement occurred after initial management. The aim is to increase the serum potassium concentration very slowly as the serum bicarbonate level drops.
Long-term management (>72 hours) includes the following:
-
Discontinuance of intravenous (IV) fluids
-
Oral administration (q6-8h) of calculated daily amounts of chloride, sodium, and potassium required to correct serum electrolyte levels
-
Other management procedures as appropriate for the condition determined to be the primary cause of hypochloremic alkalosis
Surgical or endoscopic intervention is unnecessary except in particular circumstances (eg, when the cause of hypochloremic alkalosis is an upper GI tract abnormality)
Dietary measures that may be considered include the following:
-
Kilojoule intake appropriate for the patient’s catabolic status
-
Additional protein to prevent malnutrition
-
Additional fat, depending on the individual patient’s requirements
-
Multivitamins and hematinic agents as required
-
Supplemental trace elements (eg, zinc) as necessary
-
High-sodium and high-potassium diets for patients with Bartter syndrome or CLD
See Treatment and Medication for more detail.
Background
Hypochloremic alkalosis is common in hospitalized children and is rare in outpatient settings. In the neonatal intensive care unit (ICU), this form of alkalosis frequently results from diuretic therapy for bronchopulmonary dysplasia. Hypochloremic alkalosis due to loss of gastric acid via nasogastric tube suctioning is also common in pediatric ICUs.
Other rare but potentially serious causes must be considered in any child presenting with failure to thrive, poor development, and a family history of neonatal demise and metabolic alkalosis in the absence of diuretic or laxative abuse. Repeated vomiting may be a clue that the patient has severe gastroesophageal reflux or pyloric stenosis.
A history of polyhydramnios is helpful; polyhydramnios may result from polyuria or congenital diarrhea. A lack of both symptoms may help identify cystic fibrosis. Severe hypochloremic metabolic alkalosis may be the presenting metabolic derangement for multiple conditions. Molecular diagnostic procedures sometimes help resolve differential diagnoses. Severe brain damage and psychomotor retardation may occur in children when diagnosis and treatment are delayed.
Etiology
Hypochloremia is defined as a serum chloride level of less than 95 mEq/L. Hypochloremia results from either low chloride intake or excessive chloride wasting. Low chloride intake is very uncommon. Excessive chloride wasting often occurs in hospitalized children, usually as a consequence of diuretic therapy or nasogastric tube suctioning. Chloride-wasting syndromes, including Bartter syndrome, congenital chloride-losing diarrhea (CLD), and cystic fibrosis, result from renal tubular loss, defective electrolyte transport across intestinal epithelia, and chloride loss via the skin, respectively. [1] There have been reports of dietary deficiencies or formula lacking chloride causing metabolic alkalosis and severe neurological consequences. [2, 3, 4] However, these causes are now rare since the introduction of standard nutritional guidelines for formulas and dietary requirements.
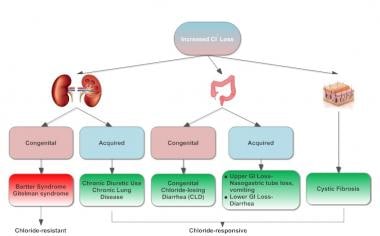
Hypochloremic alkalosis can be classified into two categories: chloride-responsive and chloride-resistant. Causes of chloride-responsive alkalosis (extrarenal chloride loss) include recurrent vomiting, gastric acid loss, diuretic-induced alkalosis (loop or thiazide diuretics), and posthypercapnic metabolic alkalosis. CLD, cystic fibrosis, and laxative abuse are also potential causes.
With respect to chloride-resistant alkalosis (with either euvolemia or hypovolemia), renal chloride wasting, as well as severe potassium and magnesium depletion, may occur in patients with Bartter syndrome and, rarely, in patients with Gitelman syndrome. [5] Chloride-resistant alkalosis may result from acute administration of exogenous alkali, as in milk-alkali syndrome or after massive blood transfusion. Rare causes include hypercalcemia due to vitamin D toxicity and hyperparathyroidism and nonreabsorbable anions.
Pathophysiology
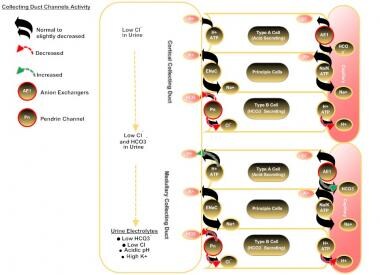
The renal collecting duct plays an important role in acid-base balance by maintaining bicarbonate (HCO3-) reabsorption and secretion. [6] Abundant evidence now supports pendrin as an important regulatory transporter in the cortical collecting ducts, which responds briskly [7] in vivo and in vitro [8] to alterations in chloride intake and to acid-base perturbations, including metabolic alkalosis and acidosis and respiratory acidosis. The figure below depicts a detailed explanation of ion exchange at collecting duct cells in a hypochloremic condition.
The collecting duct plays the main role in acid-base balance by maintaining HCO3- reabsorption and secretion. In type-B intercalated cells of the cortical collecting duct, pendrin channel (Pn) activity is increased because of a low Cl- concentration in that segment (due to low chloride levels in ultrafiltrate from hypochloremia), but secretion of HCO3- is inhibited by insufficient Cl- for anion exchange. HCO3- reabsorption is continued by Na+/H+ exchange in the principal cell and in the type-A intercalated cells. In the medullary collecting duct, HCO3- reabsorption is continued because a decreased HCO3- concentration in that segment enhances H+ secretion in type-A cells. [9] Rat studies have shown that, after Cl- delivery to the cortical collecting ducts increases, HCO3- secretion occurs and medullary HCO3- reabsorption diminishes, allowing correction of the hypochloremic alkalosis. In these studies, bicarbonaturia occurred within minutes of Cl- administration intravenously, and Cl- did not increase in the urine until correction of serum Cl- was nearly complete. [8]
Chloride-losing diarrhea
Chloride-losing diarrhea (CLD) is caused by a defective anion exchange protein, an epithelial chloride/bicarbonate (Cl-/HCO3-) exchanger located in the brush border of the ileum and colon, resulting in defective intestinal chloride absorption and secretion of HCO3-, with a secondary defect in sodium/hydrogen (Na+/H+) transport, altogether leading to intestinal losses of both sodium and water, hypochloremia, hyponatremia, and metabolic alkalosis.
Epidemiology
The frequency of hypochloremic alkalosis is unknown, both in the United States and worldwide. However, there is some reason to think that this condition may be more common worldwide than was previously accepted. Many cases of CLD have emerged from Eastern Europe and Middle Eastern Arab countries; indeed, the largest purported series is from Saudi Arabia. [10] Fewer cases in the English language literature have been reported in the Far East and North America, perhaps because of cultural and academic barriers.
CLD can manifest before birth as severe midtrimester polyhydramnios. Metabolic derangements may manifest as early as the first few days of life. Bartter syndrome may present at any age but primarily occurs in infants younger than 1 year. Hypochloremic alkalosis resulting from cystic fibrosis is infrequent in infancy but can become more severe in summer because of excessive chloride loss from sweating. Drug-related hypochloremic alkalosis is observed at all ages. Males and females are affected in equal numbers.
Prognosis
Prognosis is usually good for patients with Bartter syndrome, provided the patient complies well with treatment. Children who receive effective treatment have minimal risk of severe renal damage.
In patients with CLD, renal failure and ESRD may complicate the picture if diagnosis and treatment are delayed.
In patients with cystic fibrosis, prognosis depends on the severity of lung and liver involvement.
Anorexia and polyuria eventually lead to malnutrition and growth failure. Chronic dehydration frequently causes constipation. A small muscle mass and muscle wasting are frequently seen in patients following a late diagnosis or in untreated patients.
CNS effects include cerebral dysfunction and defective cognitive function resulting from chronic hypoperfusion in moderate-to-severe metabolic alkalosis due to hypokalemic and hypochloremic states. Hypopnea is due to depression of respiratory drive. CNS calcification occurs in some patients for unclear reasons. Seizure disorder, brain atrophy, and mental retardation are other known sequelae.
Depending on the renal disorder, complications may include nephrocalcinosis, interstitial nephropathy, hypercalcemia, hyperuricemia, hypertension during the late stages of renal damage, and renal failure. Children with end-stage renal disease require renal replacement therapy in the form of hemodialysis or peritoneal dialysis. Kidney transplantation with the consequences of graft loss due to metabolic derangements adds more morbidity in these patients.
Patient Education
Genetic counseling should be considered when prenatal diagnosis is offered to mothers with familial diseases, such as cystic fibrosis, Bartter syndrome, or chloride-losing diarrhea (CLD).
Educate the caregiver regarding the primary disease and how to identify signs of dehydration and to prevent it.
Ask the clinical pharmacist to discuss the importance and methods of drug administration, timing, and adverse effects with the caregiver, in addition to storage of medications at home.
-
Infant with severe metabolic alkalosis resulting from congenital chloride-losing diarrhea.
-
Watery stool from an infant with congenital chloride-losing diarrhea. Chloride level was 205 mmol/L.
-
Renal sonogram of an infant with congenital chloride-losing diarrhea showing diffuse sclerosis.
-
Sonogram depicting severe nephrocalcinosis in a 2-year-old child with Bartter syndrome.
-
Visible bowel loops in an infant with congenital chloride-losing diarrhea.
-
Explanation of ion exchange at collecting duct cells in a hypochloremic condition.
-
Causes of hypochloremic alkalosis in children.
-
Approach to hypochloremic alkalosis.