Background
Histoplasmosis is a fungal infection caused by the dimorphic fungus Histoplasma capsulatum. The fungus grows saprophytically and develops mycelia with macroconidia and microconidia. The parasitic form is characterized by the production of yeasts 2-4 μm in diameter. Histoplasmosis is endemic in the central United States and in other parts of the world with warm humid soil and large populations of migratory birds. It is the most common pulmonary and systemic mycosis of humans. Clinical manifestations vary from a mild flulike illness that often goes unnoticed to rapidly progressive, often fatal, disseminated disease. [1] The presentation varies depending on the host's immunity and the size of the inoculum.
The principal challenges to the clinician caring for patients with histoplasmosis are to recognize the disease, which can mimic a number of processes, and to rationally use a confusing array of tests for diagnosis and treatment. In 1905, Samuel Darling described histoplasmosis in a patient working in the Panama Canal Zone. As early as the 1940s, Amos Christie, MD, and colleagues used the histoplasmin skin test to demonstrate that numerous patients with abnormal chest radiographs but negative tuberculin results actually had self-limited infection with histoplasmosis.
Pathophysiology
Five serotypes of capsulatum are known, including some avirulent strains. Histoplasma species have a mycelial form at ambient temperatures. The spores of H capsulatum (microconidia) become airborne when soil is disturbed (see Causes).
The initial neutrophil response is ineffective against the yeast form. Macrophages ingest the yeast, but they continue to proliferate. Specific immunity, which occurs 10-21 days after infection, is needed to kill the organisms. Specific helper T cells are able to activate macrophages to form the granulomas that are characteristic of the disease. Natural killer cells mediate extracellular killing, which antibodies enhance.
Pneumonitis, with a predominant mononuclear infiltrate, peaks 2 weeks after infection. Granulomas can form in the pulmonary parenchyma and in the hilar and mediastinal lymph nodes. These lesions can be caseating and may develop calcification and fibrosis over time. In most infections, fungemia likely occurs at some point because splenic granulomas have been observed after asymptomatic infection. In individuals with impaired T cell–mediated immunity, other sites of infection include the bone marrow, liver, adrenal glands, CNS, joint spaces, heart valves, and blood vessels.
Reports describe infectious complications in almost every tissue. Reactivation of infection may occur in individuals who become immunosuppressed long after a primary infection; this reactivation accounts for many of the cases observed in nonendemic areas. Reinfection can occur in the setting of heavy conidial burdens but is generally mild because of specific immunity.
Recent animal studies have revealed that interleukin (IL)-1, tumor necrosis factor (TNF)-alpha, and GR 1(+) cells are important in localizing and controlling Histoplasma infection. YPS3 and cell wall alpha-(1,3)-glucan of Histoplasma are also associated with virulence.
Epidemiology
Frequency
United States
An estimated 50 million individuals have been infected with H capsulatum. Nationwide, approximately 22% of the population have positive skin-test results for histoplasmin, though the rate may be as high as 80% in endemic areas in the central United States, specifically the Ohio and Mississippi River Valleys (see the image below). Of the 500,000 individuals who are exposed annually, 50,000-200,000 develop symptoms, and 1500-4000 require hospitalization.
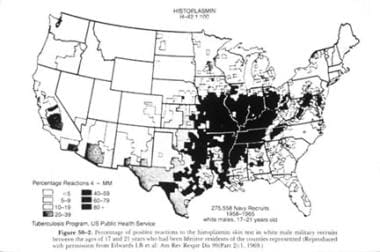 Map demonstrates the distribution of histoplasmin skin-test positivity by region. Used with permission from the American Thoracic Society.
Map demonstrates the distribution of histoplasmin skin-test positivity by region. Used with permission from the American Thoracic Society.
International
Endemic regions for histoplasmosis are found in Central and South America, in the Caribbean, in Africa, and in Asia. [2] However, microfoci are believed to occur anywhere soil conditions are appropriate to support the growth of H capsulatum.
Mortality/Morbidity
The overall mortality rate of histoplasmosis is low; most cases spontaneously resolve. In individuals with immunosuppression, progressive disseminated disease has a high mortality rate of 7-23%. Without treatment, disseminated disease is usually fatal. Disseminated infection can localize in any tissue, leading to various complications. Pericarditis and obstruction of mediastinal structures are the principal complications in individuals who are immunocompetent.
Race
No racial predilection to infection or to disease presentation is apparent.
Sex
Among adults, histoplasmosis is described more commonly in men than in women. However, certain clinical manifestations, such as erythema nodosum, are described most commonly in women. These sex differences in infection and disease are not observed in children.
Age
Histoplasmosis occurs at any age. Disseminated disease is more likely to occur in individuals at the extremes of life, unless a person has immunodeficiency. The incidence of disseminated histoplasmosis in children appears to have decreased in the last 30 years. The sex-related differences observed in infection and disease among adults are not observed in children.
-
Hilar lymphadenopathy in an 11-year-old child.
-
Map demonstrates the distribution of histoplasmin skin-test positivity by region. Used with permission from the American Thoracic Society.
-
Hematoxylin and eosin stain of infected lung tissue. Histoplasma organisms appear to have a false capsule.
-
Starling roost in Alabama.
-
Acute pulmonary syndrome in a 16-year-old female adolescent.
-
Fibrosing mediastinitis with mediastinal widening and tracheal deviation.









