Practice Essentials
A cloacal malformation is defined as an abnormal congenital confluence of the rectum, vagina, and urethra into a single common channel (see the image below). [1, 2] This defect is one of the most formidable technical challenges in pediatric surgery.
Cloacal malformations occur in 1 per 20,000-25,000 live births; the etiology is unknown. They occur exclusively in girls and represent the most complex defect in the spectrum of anorectal malformations (ARMs). Families of a newborn baby girl who has a cloacal malformation have four main concerns, as follows:
-
Maintenance of renal function
-
Urinary continence (social)
-
Bowel continence (social)
-
Sexual function and fertility
The goals of treatment include performing a successful anatomic reconstruction and achieving bowel and urinary control, as well as normal sexual function, while maintaining the patient's long-term renal health. In many girls with complex malformations, however, performing a sound anatomic repair by no means guarantees a successful functional outcome. Surgical risk and morbidity must be weighed in patients with complex malformations.
Diverse surgical treatments for the management of cloacal malformations have been proposed in the past. The most common approach consisted of repairing the rectal component of the malformation without repairing the urogenital sinus or planning its repair in a second stage. A combined abdominal, perineal, vaginal, and simultaneous rectal pull-through was also used.
Some treatments were adequate for certain malformations, but not for others. The perineal approach to the urogenital sinus aspect of the repair may be useful in patients with low defects but not in those with more complex defects. Similarly, the abdominal approach is required for some anomalies but not for others. Traditional approaches were limited in their exposure and thus could not clearly define the complex anatomy of the defect, and the urinary sphincter and anorectal sphincter were matters of speculation.
In the 1960s and 1970s, Hendren described cloacal repair with a specific focus on the urologic reconstruction. [3] In 1982, the posterior sagittal approach, which was used to repair an imperforate anus (as described by Peña and Devries [4] ), was first performed for a cloacal malformation. [3] This procedure was ideally suited for the more complex repair of cloacal malformations and led to the operation described as posterior sagittal anorectovaginourethroplasty (PSARVUP). This approach allowed direct exposure to the complex anatomy and provided excellent visualization of the voluntary muscles of urinary and fecal continence.
Total urogenital mobilization (TUM), introduced by Pena in 1992, in many ways changed the approach to repair in these patients. TUM had the advantage of all but eliminating the risk of a dreaded complication of cloacal reconstruction, urethrovaginal fistula. Though indicated for short (< 3 cm) common-channel abnormalities only, in time TUM came to be advocated for more complex cases and was described as transabdominal TUM. [5] The advent of transabdominal TUM led to a much broader application of this approach but also yielded some significant morbidity.
Subsequently, a newer approach was proposed that took into account not only common-channel length but also urethral length for the purposes of surgical planning and decision-making. [6] This approach has been shown to lead to much improved urethral preservation in complex malformations. [7] Such improvement is important in that many patients with complex malformations may need intermittent catheterization, and urethral preservation obviates the need for complex urologic reconstruction.
Subsequently, several groups proposed the use of minimally invasive techniques to perform the abdominal portions of the reconstruction. Such techniques include a laparoscopic approach to the rectal portion, the urogenital portion, or both. [8]
For patient education resources, see the Kidneys and Urinary System Center, as well as Bladder Control Problems.
Pathophysiology
Genitourinary defects
More than 85% of all patients with a cloaca have an associated urogenital anomaly:
-
Persistent cloaca - 90%
-
Recto–bladder neck fistula - 84%
-
Rectoprostatic urethral fistula - 63%
-
Rectovestibular fistula - 47%
-
Rectobulbar urethral fistula - 46%
-
Rectoperineal fistula - 26%
-
ARM with no fistula - 31%
All patients must be evaluated at birth for an associated urologic problems; the most valuable screening test is ultrasonography (US) of the abdomen and pelvis.
Urologic evaluation, either by a pediatric surgeon experienced with pediatric urology or in consultation with a pediatric urologist, is necessary before one can proceed with colostomy. This provides the surgeon with the information needed to address any urologic problem at the time of the colostomy.
In addition, drainage of a distended vagina (hydrocolpos) in the presence of hydronephrosis may be required. [9] This may be done through the common channel in the form of intermittent catheterization or transabdominally in the form of a vaginostomy tube or surgical vaginostomy. The treatment of hydrocolpos has evolved: Whereas previously most patients with hydronephrosis and hydrocolpos had a vaginostomy formed at the time of the colostomy formation, the majority of surgeons recently polled are now using intermittent catheterization with close follow-up.
Tethered cord
A tethered spinal cord refers to a fixation of the filum terminale to the lower end of the spinal canal.
Tethered cord has a known association with ARMs and is particularly common in patients with persistent cloaca.
Motor and sensory disturbances of the lower extremities, as well as bladder and bowel dysfunction, may result.
Patients with ARMs and tethered cord have a worse functional prognosis regarding bowel and urinary function. However, they also have higher anorectal defects, less developed sacra, associated spinal problems, and less developed perineal musculature; thus, the actual impact of tethered cord alone on the functional prognosis is unclear.
Untethering of the cord for motor and sensory problems is indicated in the neurosurgical literature. No definitive evidence suggests that this operation affects the functional prognosis of a patient with an ARM. Some evidence in the urologic literature indicates that this operation may improve urodynamics. [10]
Anomalies of the sacrum, particularly hypodevelopment, sacral hemivertebrae, and hemisacra, are associated with tethered cord and most likely fall along the spectrum of caudal regression, of which spinal anomalies are a part.
Spinal US in the first 3 months of life and magnetic resonance imaging (MRI) thereafter are useful in diagnosis.
Sacrum and spine anomalies
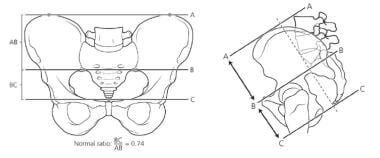
The sacrum is the most frequently affected bony structure. An objective assessment of the sacrum can be obtained by calculating the sacral ratio. The sacrum is measured, and its length is compared with bony parameters of the pelvis (see the image below).
To calculate the sacral ratio, the distance from the coccyx to the sacroiliac joint is divided by the distance from the sacroiliac joint to the top of the pelvis. Lateral radiography is more accurate than the anteroposterior (AP) view because the calculation is not affected by the tilt of the pelvis. [11]
The assessment of the hypodevelopment of the sacrum correlates with the patient's functional prognosis. Normal sacra have a ratio higher than 0.7. Bowel control has rarely been observed in patients with ratios lower than 0.3. [12]
A hemisacrum is often associated with a presacral mass, commonly a teratoma, or anterior meningocele; malignant yolk sac tumor, though rare, has been well described. The Currarino triad, which includes an ARM, a hemisacrum, and a presacral mass, has been described.
Hemivertebrae may also affect the lumbar and thoracic spine, leading to scoliosis.
Patients may have spinal anomalies other than tethered cord, such as syringomyelia and myelomeningocele.
Epidemiology
The literature reports that the incidence of cloacal malformations is approximately 1 per 20,000-25,000 live births. However, the literature often contains reports of rectovaginal fistula, which are most likely cloacal malformations in which the rectal component was corrected but the urogenital sinus was not. Therefore, cloacal malformations are probably more common than was previously thought.
Prognosis
Functional prognosis with regard to achieving fecal continence depends on the complexity of the defect and the status of the spine and sacrum.
Fecal continence is more likely in patients with a less complex cloaca and in those who have a normal sacrum. Approximately 70% of patients can achieve voluntary bowel movements (for comparison with patients with other anorectal anomalies, see Imperforate Anus [Anorectal Malformation]). The percentage of these patients who continue to soil is not insignificant, and many will require bowel management to remain clean, according to the Rome criteria. [13]
Postoperative monitoring of bowel function is similar to that in patients with imperforate anus (see Surgery for Pediatric Anorectal Malformation [Imperforate Anus]).
Urinary control varies according to the length of the common channel and the length of the urethra (see the image below).
Intermittent catheterization is required in seven of 10 patients with persistent cloaca who have a common channel longer than 3 cm, compared with one in five patients with a common channel shorter than 3 cm. Many patients will need further urologic interventions to be dry. Overall, more than 70% of patients in two large series were unable to void spontaneously with full urinary control. [14, 15] This finding prompted the development of an approach that looks to ensure adequate urethral length and therefore maintains the bladder neck above the urogenital diaphragm. Functional outcomes from this approach are awaited. [6]
In many patients, the bladder neck is competent, and the patients who require catheterization remain dry between voids. If catheterization is not performed, overflow incontinence occurs. Another group of patients either lose the urethra after surgery or are left with a short urethra and struggle with incontinence. It is these patients, along with those who have significant spinal abnormalities or poorly developed bladder neck function, who may require urinary diversion (eg, a Mitrofanoff procedure) with bladder-neck tightening and, occasionally, bladder augmentation.
Functional patient/parent reported outcome measures (PROMs) are becoming the standard of care in many fields, and future reporting of results in this population should include them. In addition to functional outcomes measures, patient/parent reported quality of life measures should also be reported to examine the benefit of various treatment modalities.
It is not possible to discuss prognosis in cloaca patients without including renal health. The incidence of renal failure in these patients varies widely but has been reported to be in the range of 20-50%. [16] The authors advocate a nephron-protecting approach from day 1 and believe that all patients should be followed carefully by urology and nephrology when necessary.
-
Calculation of sacral ratio.
-
Newborn with persistent cloaca and massive hydrocolpos.
-
Ultrasonogram showing hydronephrosis before and after drainage of hydrocolpos, which was compressing trigone of bladder.
-
Hysterosalpingogram in baby who has persistent cloaca with symmetric hemiuteri.
-
Perineum of baby with persistent cloaca.
-
Perineum of baby with persistent cloaca.
-
Perineum of baby with persistent cloaca. Note single perineal orifice.
-
Perineum of baby with persistent cloaca showing common finding of small external genitalia.
-
Artist's drawing of persistent cloaca, lateral view.
-
Posterior sagittal approach to repair cloacal malformation, showing rectum, vagina, and urethra.
-
Total urogenital mobilization during repair of persistent cloaca.
-
Repair of persistent cloaca with 3-cm common channel.
-
MRI of teenage girl born with persistent cloaca, with pelvic masses caused by metrocolpos and metrometra.
-
Artist's drawing of retrograde menstruation due to left atretic hemicervix in patient with persistent cloaca and hemiuteri.
-
Artist's view of laparotomy in patient with menstrual blood–filled anomalous müllerian structures.
-
Cross-lateral radiographic fluoroscopic image of cloaca (cloacagram). Hydrosoluble contrast is injected via cloaca into orifices of the bladder (solid black arrow), vagina (white arrow), and rectum (dashed black arrow) to demonstrate anatomic relation of these organs.
-
Cloacal malformation. Posterior sagittal incision, with rectum, vagina, and common channel exposed. Reproduced with permission from © Center for Colorectal and Pelvic Reconstruction at Nationwide Children’s Hospital.
-
Cloacal malformation. Rectum separated, with vagina opened and Foley catheter visible in common channel and urethra. Reproduced with permission from © Center for Colorectal and Pelvic Reconstruction at Nationwide Children’s Hospital.
-
Cloacal malformation. Rectum separated, with vagina now being separated from posterior urethra and bladder neck. Reproduced with permission from © Center for Colorectal and Pelvic Reconstruction at Nationwide Children’s Hospital.
-
Cloacal malformation. Repair of urethra/common channel in layers, followed by coverage with biologic patch and ischiorectal fat pad. Reproduced with permission from © Center for Colorectal and Pelvic Reconstruction at Nationwide Children’s Hospital.