Practice Essentials
Cyclic vomiting syndrome (CVS), first described in children by Samuel Gee in 1882, is a chronic functional disorder of unknown etiology that is characterized by paroxysmal, recurrent episodes of vomiting. (See the image below.)
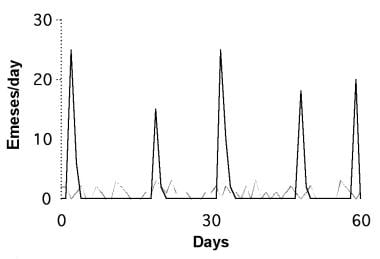 Cyclic versus chronic temporal patterns of recurrent vomiting. Number of emeses is plotted over 2-month period. Chronic pattern, represented by thin dashed line, has low grade on nearly daily basis (eg, gastroesophageal reflux). Cyclic pattern, represented by heavy solid line, involves high-intensity episodes intermittently once every several weeks (eg, cyclic vomiting syndrome).
Cyclic versus chronic temporal patterns of recurrent vomiting. Number of emeses is plotted over 2-month period. Chronic pattern, represented by thin dashed line, has low grade on nearly daily basis (eg, gastroesophageal reflux). Cyclic pattern, represented by heavy solid line, involves high-intensity episodes intermittently once every several weeks (eg, cyclic vomiting syndrome).
The pathophysiology is unknown (see Pathophysiology and Etiology), but data suggest a strong genetic component in children with CVS, with evidence of mitochondrial heteroplasmies that predispose to CVS and other related disorders (eg, migraine and chronic fatigue syndrome). Other theories include autonomic dysfunction and, possibly, corticotropin-releasing factor (CRF) because stress is known to be a trigger for these episodes. The possible role of cannabis in causing CVS has been examined, though it remains controversial.
Signs and symptoms
CVS is characterized by recurrent, discrete, stereotypical episodes of rapid-fire vomiting between varying periods of completely normal health. This on-and-off stereotypical pattern of vomiting is nearly pathognomonic.
See Presentation for more detail.
Diagnosis
Because no biochemical markers for CVS have been identified, physicians must initially look for alarming symptoms and then tailor the subsequent workup accordingly. Depending on the presenting symptoms and signs other than vomiting, different diagnostic approaches are recommended.
See Workup for more detail.
Management
In the absence of known pathophysiology, treatment of CVS remains empiric.
See Treatment and Medication for more detail.
Patient education
For ongoing support and information, families are encouraged to contact the Cyclic Vomiting Syndrome Association, which is an international voluntary organization that serves the needs of patients in the United States and Canada.
Pathophysiology and Etiology
The etiology and pathophysiology of CVS are not known. However, studies have suggested several potential brain-gut mechanisms.
Migraine-related mechanisms have been proposed. [1, 2] In one study, patients with CVS have a significantly higher prevalence of family members with migraine headaches (82% vs 14% of control subjects with a chronic vomiting pattern). Furthermore, 28% of patients with CVS whose vomiting subsequently resolved developed migraine headaches. Approximately 80% of affected patients with family histories positive for migraine respond to antimigraine therapy. [1, 2]
Mitochondrial DNA (mtDNA) mutations may be involved in the pathogenesis of CVS. Boles et al demonstrated that 86% of children with CVS and neuromuscular disease had a history of migraines on the matrilineal side. In children with CVS, 2 mtDNA polymorphisms (16519T and 3010A) are expressed with a high degree of frequency and may serve as a surrogate marker for predisposition to the disease. [3]
The 16519T polymorphism is 6 times more common in pediatric CVS patients than in control populations. [4] The 3010A polymorphism increases the likelihood of CVS in subjects with 16519T by as much as 17 times. These mtDNA polymorphisms may account for the clustering of functional conditions and symptoms in the same individuals and families. One small (and possibly underpowered) study found that adult-onset CVS, unlike pediatric CVS, CVS is not associated with these polymorphisms, suggesting a degree of genetic distinction. [2]
Sympathetic hyperresponsiveness and autonomic dysfunction also appear to contribute to the pathogenesis of CVS. [5] Many associated symptoms, such as pallor, flushing, fever, lethargy, salivation, and diarrhea, are mediated by the autonomic nervous system. [6, 7] Several studies support altered autonomic function in CVS.
Rashed et al [8] and To et al [9] demonstrated heightened sympathetic cardiovascular tone in patients with CVS. Kasawinah et al reported the successful use of dexmedetomidine, an alpha2-adrenergic agonist, to treat CVS. [10] In a small study involving 6 children with CVS, all patients had sympathetic autonomic dysfunction, affecting mainly the vasomotor and sudomotor systems. Symptoms developed during tilt testing in half of these patients, suggesting that these findings may play a role in the pathophysiology of CVS. [11]
To evaluate this association with autonomic dysfunction, a cross-sectional study was performed in which the Ohio dysautonomia (ODYSA) questionnaire was administered to 21 patients with CVS (3 children) and 46 patients with migraines. [12] The 2 patient groups had similar comorbid conditions, with fibromyalgia noted in 38% of subjects with CVS, orthostatic intolerance in 47% of subjects with CVS, functional dyspepsia in 9.5% of subjects with CVS, and complex regional pain syndrome in 24% of subjects with CVS.
The main limitation of this study was that the findings were not corroborated by means of either a physical examination or standard autonomic function testing. [12] However, the findings of orthostatic intolerance are of clinical significance because the use of pharmacologic therapy (eg, fludrocortisone and beta-blockers) may be considered in these patients.
In a prospective trial in adult CVS patients, Venkatesan et al found that most subjects with CVS (90%) had impairment of the sympathetic nervous system with postural tachycardia or sudomotor dysfunction while parasympathetic nerve function was intact. [13]
In this study, 17 (85%) of 20 adult CVS subjects and 2 (10%) of 20 control subjects had abnormalities on thermoregulatory sweat testing. [13] A total of 7 (35%) patients and 1 control subject had evidence of postural tachycardia with an increase of more than 30 beats/min in heart rate (HR) on standing. Of the subjects, 18 (90%) had abnormal sudomotor function, postural tachycardia, or both. The HR response to deep breathing was normal in 19 (95%) subjects with CVS and 18 (95%) controls.
The stress response, mediated by the hypothalamic-pituitary-adrenal (HPA) axis, can also potentially induce episodes of CVS. Infectious, psychological, and physical stressors are known triggers of episodes. [14, 15, 16, 17, 18] Sato et al documented increased levels of adrenocorticotropic hormone (ACTH) and cortisol, associated with extreme lethargy and hypertension, before the onset of vomiting. [19, 20, 21, 22] Furthermore, Taché showed that central CRF induced gastric stasis, emesis, or both in animals. [23]
Therefore, CRF may be a brain-gut mediator of CVS that directly connects stress and vomiting. [24] If this theory holds true, CRF receptor antagonists currently in development could theoretically ablate vomiting by blocking the CRF receptor’s vagally mediated actions. [25]
Cannabis use in CVS has received considerable attention. Chronic marijuana use has been associated with hot showers or compulsive hot water bathing and CVS, though a cause-and-effect relation has not been confirmed. The endocannabinoid system (ECS) consists of the ligands 2-AG and anandamide and the cannabinoid receptors CB1 and CB2. This system is thought to play a role in nausea and vomiting and in coping with stress.
There is considerable evidence that activation of central and peripheral CB1 cannabinoid receptors inhibits nausea and vomiting; conversely, both nausea and vomiting are frequent adverse effects accompanying CB1 receptor antagonist use in humans. These and other data strongly suggest that the tone of the ECS regulates nausea and vomiting; further studies are needed to explore this possibility more fully. [26, 27]
That CVS has a central component has been suggested by functional magnetic resonance imaging (MRI) studies using whole-brain seed-based analysis. Patients with CVS exhibited a distinct alteration in resting state functional connectivity involving connections from the cingulate and inferior frontal gyrus (IFG), a known neural correlate of nausea. [28]
In conclusion, the pathogenesis of CVS is likely to be multifactorial, with multiple genetic, autonomic, central, and environmental factors playing a role. Further studies are needed to elucidate the exact mechanisms underlying this disorder.
Epidemiology
United States statistics
The true incidence and prevalence of CVS in the United States are unknown, although a prevalence of about 2% among US children and adults has been estimated. [29] In central Ohio, amid a predominantly White population, the prevalence of CVS in children (evaluated by the sole pediatric gastroenterology referral center) was 0.04%. [30]
International statistics
On the basis of limited epidemiologic data, Cullen and MacDonald estimated the prevalence of periodic vomiting in western Australia to be 2.3%. [6] Similarly, Abu-Arafeh and Russell observed a prevalence of 1.9% in school-aged children in Aberdeen, Scotland. [31] Both of these figures are derived from White populations and may not accurately reflect prevalence in all races or ethnic populations.
In a study performed at KEM Hospital in Pune, India, CVS accounted for 0.5% of admissions to pediatric wards during 1998-2000. In a retrospective study conducted in Japan, Chang et al found that the prevalence of CVS among children was 2.10 per 1000 population, and the prevalence among adults was 0.05 per 1000 population. [32]
In a population-based study from Ireland, the incidence of CVS was relatively high at 3.15 cases per 100,000 children. This incidence is comparable to those of other major GI diseases of childhood (eg, Crohn disease) in Ireland. [33]
Age-, sex-, and race-related demographics
The median age at onset is 4.8 years; however, CVS has been observed in infants as young as 6 days and in adults as old as 73 years. [1] The typical interval from onset of symptoms to diagnosis is 2.7 years. [1] In adults, the average age of onset is 21 years and the average age of evaluation for recurrent vomiting 34 years. [7] Females show a slight predominance over males (female-to-male ratio, 57:43). CVS occurs in all races but seems to affect White persons disproportionately.
Prognosis
Most published series indicate that CVS lasts an average of 2.5-5.5 years, resolving in late childhood or early adolescence. A few patients continue to be symptomatic through adulthood.
As early as 1898, clinicians observed that some patients went on to develop migraine headaches. That some children with CVS progress to abdominal migraines and then to migraine headaches implies that there may be a sequential progression of age-dependent manifestations of migraine.
A survey by Abu-Arafeh et al found the mean ages of children with CVS, abdominal migraines, and migraine headaches to be 5.3 years, 10.3 years, and 11.5 years, respectively. [31] This finding supports the developmental progression from vomiting to abdominal pain to headache. In unpublished data, Li and Hayes determined that nearly one third of patients develop migraines after resolution of CVS and predicted that nearly 75% would develop migraines by age 18 years.
A study of 31 patients with CVS by Hikita et al found that the median overall duration of the disorder was 66 months and that 44% of the patients seen for follow-up (25 patients) developed migraine. The authors also found abnormally high adrenocorticotropic hormone and antidiuretic hormone levels among the 25 patients for whom follow-up data were available. Significant correlations between attack duration and adrenocorticotropic hormone levels and attack duration and antidiuretic hormone levels were noted. [34]
Although patients are well about 90% of the time, CVS can be medically and socially disabling. More than 50% of patients require intravenous (IV) fluids, compared with less than 1% of patients with rotavirus gastroenteritis. The average annual cost of testing, treatment, and absenteeism totals $17,000. Children miss an average of 24 school days per year and often need home tutoring or, occasionally, home schooling. Additionally, because of its frequency during times of excitement, CVS has ruined many birthdays, holidays, and vacations. [30]
In adults, substantial morbidity is associated with CVS, perhaps because of lack of awareness and resultant delays in diagnosis. In a study of 41 CVS patients, Fleisher found that 32% were completely disabled at the time of diagnosis. [7] A total of 293 procedures were performed in the 41 patients, and none were indicative of organic etiology. In addition, 17 surgical procedures, including 10 cholecystectomies, appendectomies, exploratory laparotomies, a pyloroplasty, and a hysterectomy, were performed without any therapeutic benefit.
Adults and children with CVS also have multiple emergency department (ED) visits (see Table 1 below), and the diagnosis is often unrecognized. [35]
Table 1. Characteristics of Emergency Department Visits in Patients With Cyclic Vomiting Syndrome (Open Table in a new window)
Characteristic |
Adults (n = 104) |
Children (n = 147) |
Number of ED visits per patient with CVS (median) |
15 (range, 1-200) |
10 (range, 1-175) |
Number of ED visits before diagnosis of CVS (median) |
7 (range, 1-150) |
5 (range, 0-65) |
Diagnosis not made in ED |
89 (93%) |
119 (93%) |
Diagnosis not recognized in ED in patients with established diagnosis of CVS |
84 (88%) |
97 (80%) |
Number of different EDs visited (mean ± SD) |
4.69 ± 4.72 |
2.6 ± 2.42 |
CVS = cyclic vomiting syndrome; ED = emergency department; SD = standard deviation. |
||
Complications
A study that evaluated the relationship between anxiety and health-related quality of life in children and adolescents with cyclic vomiting syndrome (CVS) reported that children and adolescents with CVS appear to be at increased risk for anxiety. Anxiety symptoms are a stronger predictor of health-related quality of life than disease characteristics in children and adolescents with CVS. Assessment and treatment of anxiety in children and adolescents with CVS may have a positive impact on health-related quality of life. [36]
-
Cyclic versus chronic temporal patterns of recurrent vomiting. Number of emeses is plotted over 2-month period. Chronic pattern, represented by thin dashed line, has low grade on nearly daily basis (eg, gastroesophageal reflux). Cyclic pattern, represented by heavy solid line, involves high-intensity episodes intermittently once every several weeks (eg, cyclic vomiting syndrome).






