Practice Essentials
True solitary thyroid nodules occur in 0.22-1.35% of the pediatric population and in close to 4% of the adult population. However, suspected thyroid nodules merit close attention in the pediatric population because such nodules are much more likely to be malignant in children than they are in adults. In addition, thyroid cancer is much more aggressive in children and is associated with early metastasis to regional lymph nodes and parenchymal organs, most commonly the lungs and bones. See the image below.
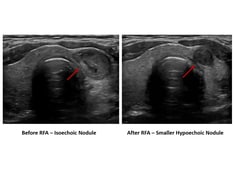
 A 12-year-old patient with an asymptomatic palpable thyroid nodule noticed upon routine physical examination.
A 12-year-old patient with an asymptomatic palpable thyroid nodule noticed upon routine physical examination.
Signs and symptoms
Benign versus malignant nodules
Benign masses are usually movable, soft, and nontender. Malignancy is associated with a hard nodule, fixation to surrounding tissue, and regional lymphadenopathy.
Reported rapid growth or recurrent laryngeal nerve dysfunction found on examination may indicate malignancy and local infiltration.
If medullary carcinoma is suspected in conjunction with multiple endocrine neoplasia (MEN) 2B, multiple mucosal neuromas, marfanoid body habitus, and skeletal defects may be evident.
Hormonal imbalance
Although most patients are asymptomatic, [1] some exhibit signs and symptoms of altered levels of thyroid hormone, as follows:
-
Hyperthyroidism - Nervousness, heat intolerance, diarrhea, muscle weakness, and loss of weight and appetite; in rare cases, exophthalmos may be present in a person with a hyperfunctioning nodule
-
Hypothyroidism - May result in cold intolerance, constipation, fatigue, and weight gain, which, in children, is primarily caused by the accumulation of myxedematous fluid.
Nerve involvement
Signs and symptoms of local nerve involvement should trigger rapid investigation, because such involvement may be indicative of local invasiveness from malignancy. The most important of these signs are dysphagia and hoarseness.
See Clinical Presentation for more detail.
Diagnosis
Laboratory studies
-
Thyroid function tests - An elevated thyroid-stimulating hormone (TSH) level may indicate agenesis of a thyroid lobe or thyroiditis; a very low TSH level indicates an autonomous or hyperfunctioning nodule
-
Antithyroid antibodies - Helpful in diagnosing chronic lymphocytic thyroiditis (ie, Hashimoto thyroiditis)
-
Complete blood count (CBC) - If abscess is suspected
-
Calcium levels - Should be monitored immediately postoperatively to assess parathyroid function and the need for supplementation
Imaging studies
-
Ultrasonography - To determine whether the nodule is cystic, solid, or mixed [2]
-
Radioiodine scintigraphy - To determine whether the nodule is cold, warm, or hot
-
Chest radiography - If malignancy is suspected, given the high incidence of early metastases to the lungs
-
Computed tomography (CT) scanning and magnetic resonance imaging (MRI) - To analyze the extent of disease by scanning the neck and chest
Histology
Follicular adenomas present the most common histology. These tumors maintain the follicular architecture of the gland and are usually encapsulated, without evidence of infiltration.
The 4 major malignancies that may be found in the thyroid gland are papillary carcinoma, follicular carcinoma, anaplastic carcinoma, and medullary thyroid cancer.
See Workup for more detail.
Management
Pharmacologic care and observation
-
Benign nodule - May simply be observed
-
Autoimmune thyroiditis - Treatment involves hormone replacement to maintain a euthyroid state
-
Infection - Abscesses should be drained and antibiotics administered
-
Warm nodule - A warm nodule without physical signs of malignancy is usually benign and may be observed with close follow-up for growth or change in the nodule
-
Hot nodule - A hot toxic nodule may require medical therapy before surgical removal; the patient should receive suppressive doses of antithyroid medications
Lobectomy
In the presence of a small, asymptomatic nodule, the surgeon may elect to perform a simple lobectomy with close follow-up observation. In such cases, full thyroid suppression also is recommended as lifetime postoperative therapy for the patient.
Nodule removal
All toxic nodules in children should be removed. In addition, if the presence of malignancy is still in question after diagnostic tests and procedures have been completed, perform surgical excision.
Total thyroidectomy
If any metastases are present, total thyroidectomy is the recommended treatment. [3] Thyroidectomy (near-total or total) may also be performed if Graves disease is diagnosed; thyroid hormone replacement therapy may not be needed if some tissue remains.
See Treatment and Medication for more detail.
Background
True solitary nodules occur in 0.22-1.35% of the pediatric population as opposed to the adult population, in which the prevalence is closer to 4%. Upon further examination, thyroid masses often reveal asymmetric enlargement of one lobe, such as in unilateral agenesis, chronic lymphocytic thyroiditis (ie, Hashimoto thyroiditis), or other abnormalities such as lymph node or thyroglossal duct cysts. In addition, developmental errors, such as ectopic tissue, may cloud the picture. Suspected thyroid nodules merit close attention, however, in the pediatric population because the presence of malignancy in such nodules in a child is much more likely than in an adult. This frequency of malignancy is estimated to be 15-25%. In addition, thyroid cancer is much more aggressive in children and is associated with early metastasis to regional lymph nodes and parenchymal organs, most commonly lung and bone.
Pathophysiology
Although benign tumors are the most common cause of thyroid nodules in children (because of the higher rates of malignancy in this population), consider the possibility of neoplasia in the presence of a solitary thyroid nodule. Missed malignancy is tragic, but the prospect of lifetime hormone replacement therapy in the absence of pathological need is frustrating, making accurate diagnosis much more vital in the pediatric population.
A palpated mass may be solid, cystic, or mixed in nature. Benign cysts can be evacuated successfully by aspiration, usually with no recurrence. The aspirated fluid is usually clear yellow or bloody, with high levels of thyroid hormones. Rarely, a parathyroid cyst is aspirated. In this case, the fluid is clear and colorless, with high levels of parathyroid hormone. A true cyst has a very low risk of malignancy. However, the presence of a cyst does not exclude neoplasia, especially if the mass is mixed. Desjardins et al found that one half of their patients with thyroid carcinoma had a cystic component in the tumor. [4]
If a palpated mass is diagnosed as a truly solitary solid thyroid nodule, scintigraphy enables the physician to classify its activity into hot, warm, or cold. Some authorities recommend that, because definitive diagnosis can only be made with fine-needle aspiration biopsy (FNAB) or excisional biopsy findings, scintigraphy findings should have a limited role in the initial diagnosis and management of thyroid nodules. However, these authors feel that radioactive iodine uptake characteristics of nodules can direct treatment and assist in estimating risk of malignancy.
Hot or autonomous nodules are less common in the pediatric population, comprising 5% of all nodules. These nodules have their own regulation and may suppress the rest of the gland. This autoregulation may cause hyperthyroidism and thyrotoxicosis. Hot nodules are fairly common in adults (comprising 20-25% of palpable nodules) and may be associated with Graves disease. The relative rarity in children is balanced somewhat by a higher tendency for thyrotoxicosis and malignancy. In children, speed of progression tends to be higher, with increased aggressiveness. However, gradual progression is also common. Initial symptoms may be insidious, such as mood and behavior changes, and may be overlooked.
Typically, most toxic nodules should be considered for surgical excision after the preoperative administration of antithyroid medications. The risk of malignancy in hot nodules in children is estimated at 2-18% (compared with < 1% in adults); therefore, one should not ignore the possibility of neoplasia. Pay careful attention to any histologic specimens because toxic nodules can display pseudopapillary structures that resemble papillary cancer.
Warm nodules are usually functioning adenomas; however, they may harbor malignancy or represent testing error. By definition, the nodule shows some function on scintigraphy, but the patient remains euthyroid. Controversy surrounds specific treatment recommendations. Some sources group warm nodules with hot nodules, whereas others group them with cold nodules. The risk of malignancy in this group is very low. Therefore, these nodules can generally be observed. However, if the patient has signs and symptoms suspicious for cancer, such as growth of the nodule, fixation to tissues, or lymphadenopathy, the nodule should be surgically excised. Observation of a warm nodule may be the optimal course; however, care should be taken to maintain follow-up with the patient.
The solitary cold nodule is the most commonly discovered type in children, comprising 40-70% of all nodules. In addition, solitary cold nodules have the highest risk of malignancy (17-36%). Most commonly, cold nodules are follicular adenomas or other benign processes such as chronic lymphocytic thyroiditis (Hashimoto thyroiditis) or Hürthle cell hyperplasia. They may also represent ectopic tissue or other benign process, such as benign lymphadenopathy or abscess. Definitive diagnosis can only be histologically made.
Hashimoto thyroiditis may cause cold nodules. It occurs in 1% of school-aged children and may present as a nodule, have generalized swelling, or be undetectable upon clinical examination. It is generally felt to be a T cell–mediated autoimmune disorder with histologic evidence of lymphocytic invasion of thyroid tissue, usually resulting in hypothyroidism; however, in 5-10% of patients, it may present initially as transient hyperthyroidism. Diagnosis is confirmed by measurement of antithyroid antibodies, including antibodies directed against thyroperoxidase (anti-TPO antibodies), which may play a role in the development of the thyroid dysfunction.
Hashimoto thyroiditis is associated with human leukocyte antigen (HLA)-DR4, HLA-DR5, and HLA-DR3 haplotypes. It may also be associated with a slight increase in the occurrence of malignancy, but whether a lymphocytic response is induced locally by the presence of cancer cells or whether the disease itself increases risk of malignancy is unclear. Thus, lymphocytic thyroiditis may actually be a premalignant condition or induced locally by the malignancy.
Some studies have found that lymphocytic thyroiditis accompanied malignancy in as many as 50% of children with cancer. The key to accurate diagnosis in these individuals is the identification and biopsy of a dominant nodule. Additionally, Hürthle cell adenomas, which are considered benign, should generally be removed because of their increased aggressiveness and higher tendency toward progression to malignancy.
The most common malignancy types are papillary and follicular carcinoma (see the image below).
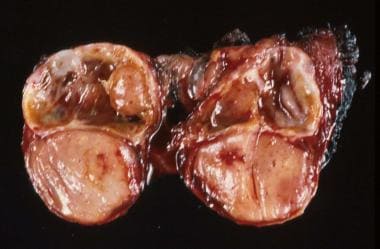 Surgical specimen of a thyroid lobe with papillary carcinoma taken from a 12-year-old patient with an asymptomatic palpable thyroid nodule noticed upon routine physical examination.
Surgical specimen of a thyroid lobe with papillary carcinoma taken from a 12-year-old patient with an asymptomatic palpable thyroid nodule noticed upon routine physical examination.
Medullary thyroid cancer and anaplastic or undifferentiated carcinomas are much more rare. Thyroid cancer is more common and aggressive in children than in adults, often with cervical lymph node metastases at the time of initial evaluation. Thyroid malignancy also metastasizes to the lungs in 10% of individuals. These metastases sometimes occur without lymph node spread, especially in individuals with follicular carcinoma. Cancer is also found in the contralateral lobe in as many as 66% of individuals with thyroid malignancy. Other sites of spread include the spinal cord, base of the tongue, and bone, especially the skull, tibia, and costochondral junction. Even metastatic thyroid cancer responds to treatment. Diligently search for possible metastatic sites to determine therapy.
Medullary thyroid cancer is rare in children and most often occurs with multiple endocrine neoplasia (MEN). Although medullary thyroid cancer usually affects the entire thyroid gland, it uncommonly may present as a solitary thyroid nodule, especially in adolescents with sporadic incidents of medullary cancer. This tumor involves the parafollicular C cells and is a calcitonin secretor. However, the tumor may also secrete adrenocorticotropic hormone (ACTH), melanocyte-stimulating hormone (MSH), histaminase, serotonin, prostaglandins, somatostatins, or beta-endorphin. It is an aggressive tumor treated by total thyroidectomy, but surgical cure is possible if spread is limited to the central compartment of the neck.
MEN is a hereditary syndrome of endocrine tumors. Medullary thyroid carcinoma occurs in MEN 2A and MEN 2B. MEN 2A consists of medullary thyroid cancer, adrenal pheochromocytoma, and hyperparathyroidism. MEN 2A is characterized by autosomal dominant inheritance and usually becomes clinically evident when the individual is aged 12-30 years. The associated thyroid malignancy is more aggressive in younger patients and metastasizes early to perithyroid lymph nodes, liver, lung, and bone.
MEN 2B causes mucosal neuromas, typical facies, marfanoid body habitus, and medullary thyroid carcinoma. The associated thyroid cancer is especially aggressive and often appears when the individual is aged almost 5 years. In both syndromes, because of disease aggression, early genetic identification is recommended with prophylactic thyroidectomy.
Etiology
Many risk factors are associated with the development of thyroid nodules and cancer. A family history of thyroid disease, benign or malignant, significantly increases risk. Fowler et al found that a family history of thyroid disease was present in 41% of their patients with thyroid nodules. [5] A family history of endocrine tumors also has been shown to increase risk, especially in persons with MEN. Increased risk has been found in some endemic areas, although environmental reasons have not been elucidated fully. In the pediatric population, pubertal girls are more likely to develop a thyroid nodule, although the risk of malignancy in these individuals is lower than that in boys. Thyroid disease has also been associated with familial polyposis syndrome.
Exposure to certain carcinogens predisposes patients to the development of thyroid disease. Previous head and neck irradiation is the most obvious and well-known risk factor.
In the first half of the 20th century, head and neck irradiation was used widely for treating a number of benign conditions, including acne, tonsillar enlargement, thymic enlargement, and tinea capitis. During this period, the incidence of thyroid nodules in children and the risk of malignancy in the nodules were much higher.
In the 1950s, 70% of thyroid nodules in children harbored malignancy. Fortunately, widespread misuse of irradiation has ceased, and malignancy rates have fallen.
Irradiation is still a factor in children who have received therapeutic radiation for Hodgkin lymphoma, bone marrow transplants, or other malignancies or in those who have been exposed to unusual environmental radiation, such as the Chernobyl accident.
Thyroid tumors may occur as early as 5 years to as late as 40 years after radiation exposure, with a peak at 10-20 years after treatment. Radiation levels as low as 0.1 Gy have been demonstrated to increase the risk of cancer. Nuclear fallout exposure, such as that which occurred at Nagasaki, Hiroshima, and Chernobyl, also significantly increases risk. Children near Chernobyl were 62 times more likely to develop thyroid cancer after the Chernobyl incident than before it occurred. These tumors were especially aggressive, often occurring 4-6 years after exposure.
A history of other malignancy may also increase risk for thyroid cancer. Alkylating agents have been associated with the development of thyroid nodules and malignancy. In addition, thyroid cancer comprises 9% of all second malignancies, most often associated with Hodgkin lymphoma. The mean age at incidence of second malignancies is 20 years.
Several genetic markers are under investigation for their association with thyroid tumors. Papillary tumors are more likely to demonstrate abnormalities on chromosome arm 10q, whereas follicular tumors more often involve chromosome 3.
The ras proto-oncogene is present in 80% of follicular tumors and often is present in follicular adenomas. It is also found in 20% of papillary tumors, and the presence of p21 ras is considered a prognostic indicator.
The ret proto-oncogene is associated with papillary tumors and medullary cancer, both familial and nonfamilial. It may be induced directly by radiation exposure. The presence of ret mutations in patients with family histories of MEN 2 is an indication for prophylactic thyroidectomy.
Finally, mutations in the thyroid-stimulating hormone (TSH)-receptor gene have been associated with the development of papillary tumors. As genetic research continues, the actual cause of thyroid tumors may become more evident.
Epidemiology
United States statistics
The prevalence of solitary thyroid nodules in children is relatively low (0.22-1.35%) compared with adults (4%). The frequency of malignancy in nodules of pediatric patients is much higher than in those of adults, estimated at 15-25% compared with an adult rate of 4%. Malignancy rates decrease to 11% in adolescence, more closely approximating adult rates. Thyroid cancers comprise 0.5-3% of childhood malignancies; 2.7-10% of the 13,900 new thyroid cancer cases each year occur in children. In addition, thyroid cancer comprises 9% of second malignancies. Most thyroid nodules are benign, either cystic or adenomatous lesions. Other benign disease processes may present with nodularity, most prominently autoimmune thyroiditis (chronic lymphocytic Hashimoto thyroiditis); 10-15% of these cases are associated with nodularity. However, an increased risk of malignancy occurs with autoimmune thyroiditis, and, in some cases, its nodules have harbored malignancy.
Changing medical practices have lowered the incidences of nodules and malignancies. In the 1950s, solitary thyroid nodules in children had a 70% risk of malignancy, most likely because of the widespread use of head and neck irradiation for benign disease processes. During this period, 80% of children with thyroid nodules had undergone such irradiation. Modern malignancy rates have fallen to 15-25%. Hung et al have demonstrated that this rate of malignancy may be falling further, even in patients with no history of irradiation. [6] From 1963-1990, in Hung et al's irradiation-free pediatric population, the prevalence of malignancy was 20%. From 1991-1998, this rate fell to 5%. [7] Further examination in the decades to come may continue to support this finding.
International statistics
Some variation has been recognized in the occurrence of thyroid nodules throughout the world. The most common determining factors are endemic iodine intake and nuclear fallout exposure. In the areas surrounding Nagasaki, Hiroshima, and Chernobyl, rates of thyroid disease have greatly increased. One study showed that, after the incident at Chernobyl, incidence of thyroid disease in Eastern Europe increased to 62 times the normal rate. [8] In addition, thyroid disease was found in increasing numbers in the atolls near the Bikini atoll in the Marshall Islands, where the United States tested nuclear arms. The Rongelap and Utrik atolls especially have shown correlation with fallout exposure; however, the picture is clouded by concomitant decreased iodine intake by individuals in this area.
The widespread use of iodized salt has helped to decrease the occurrence of thyroid disease, including nodular disease. However, iodized salt is not used in some countries, especially in underdeveloped areas. Iodine deficiency has been documented in many areas, including Tanzania, Ecuador, and Fiji. In the absence of iodized salt, a diet rich in fish may provide enough iodine; however, some species contain much more iodine than others, and consuming a fish-rich diet does not guarantee iodine sufficiency.
An international population-based study found that the incidence of thyroid cancer among children and adolescents ranged from 0.4 (in Uganda and Kenya) to 13.4 (in Belarus) cancers per 1 million person-years. The incidence rates among pediatric patients mirrored the rates among adults in each country. [9]
Race-, sex-, and age-related demographics
No race predilection has been described.
Thyroid nodules are 2-3 times more common in girls than in boys, with pubertal girls being at the highest risk. However, the probability that a nodule has associated malignancy is higher in boys than in girls. One study noted that the frequency of cancer in thyroid nodules in boys was twice as high as that in girls, 26.3% versus 13.5%.
Thyroid nodules are quite infrequent in infants and young children. The incidence appears to increase with age, and they are more common in adult patients. In the pediatric population, pubertal females are more likely to develop a thyroid nodule, although the risk of malignancy in these individuals is less than in younger girls or in boys.
Prognosis
Because mortality rates for thyroid cancer approach zero, prognosis is based on diagnosis of malignancy and progression-free survival rates. Most pediatric patients with a solitary thyroid nodule can expect a normal life span. Even in patients with malignancy, the progression-free survival rate is 60-70% at 10-20 years.
Determinants of poor prognosis include younger age (< 10 y), extensive pulmonary metastases, and tracheal and laryngeal invasion. Medullary thyroid cancer and anaplastic cancer also result in poor outcomes.
Nondiploid DNA in tumor cells, overexpression of p21 ras, or mutations of the n-ras gene indicate poor prognosis. Close follow-up care after treatment is essential because late deaths from extension of residual disease can occur.
Morbidity/mortality
The prognosis of a solitary thyroid nodule is generally quite good, even with diagnosed malignancy. Despite early metastasis and the relative aggressiveness of disease in the pediatric population, the 10-year and 20-year mortality rates are almost zero. Because of this, survival rates are often based on the progression-free survival rate.
In a study of 329 pediatric patients with thyroid cancer, Newman et al found that the progression-free survival rate was 67% at 10 years and 60% at 20 years. [10] They reported only 2 disease-related deaths. Factors contributing to less favorable prognosis vary among studies; however, patients younger than 10 years are generally considered to have an increased risk for poor outcomes. Other risk factors for poor prognosis are residual cervical disease after thyroidectomy, extensive pulmonary metastases, and tracheal and laryngeal invasion. Unfortunately, younger patients with thyroid cancer are likely to have more extensive disease on diagnosis than older patients, confusing the independence of these risk factors. Genetic markers indicating poor prognosis include nondiploid DNA, overexpression of p21 ras, and mutations of the n-ras gene.
Histologic findings also help determine mortality rates. Patients exhibiting papillary carcinoma or well-differentiated follicular carcinoma with proper treatment can have excellent recovery. Undifferentiated follicular cancer and anaplastic carcinoma cause poor outcomes. Medullary thyroid carcinoma in association with MEN has an increased mortality rate, as high as 50% at 10 years with MEN 2B. For this reason, prophylactic thyroidectomy is recommended for patients who have a family history of MEN and the proper genetic markers.
Operative morbidity mainly involves parathyroid complications, nerve injuries, and wound complications. Some centers report more complications with extensive operations as opposed to lobectomy; however, this finding is not universal. Most reports indicate that younger patients are more at risk of operative and recovery complications.
The consequence of hypothyroidism in a child can be devastating, whether the child is rendered hypothyroid by surgery, ablation, or by pathology. Growth delays and intellectual disability can be severe if hormone deficiency is prolonged. Adequate replacement is fundamental to prevent hypothyroidism. Lifetime treatment from childhood involves adjustment in dosing based on changing size and development needs. Compliance with therapy and follow-up may become an issue.
Complications
The most common complications of thyroidectomy are injuries to the recurrent laryngeal nerve and parathyroid compromise, causing hypocalcemia. Both of these complications have been divided into temporary (< 6 mo) and permanent categories. Permanent hypocalcemia has occurred in 6-27% of operative cases, whereas, in some studies, temporary hypocalcemia has affected an additional 29%.
In one study, recurrent laryngeal nerve damage temporarily caused difficulties in 12% of cases and permanently caused difficulties in 2%. Overall, permanent damage rates have been estimated at 0-24%. This wide range is most likely the result of differing treatment and surgical techniques.
Some centers remove tumor-invaded recurrent laryngeal nerves, whereas others have achieved good results with careful dissection and subsequent treatment with131 I. Millman et al assert that, with experience and proper technique, the rates of both these complications should approach 1%. [11]
Much more rarely, other major complications can affect recovery. Damage can occur in cranial nerves VII, X, and XI and the superior laryngeal nerve. An occasional postoperative pneumothorax has been noted. Postoperative hemorrhage can be devastating because of possible airway compromise and may cause emergent reoperation. In addition, required tracheostomy and extensive wound necrosis or infection can occur, severely delaying recovery.
Minor complications include hypertrophic scarring, delayed healing, seromas, temporary dysphagia, facial edema, and serous otitis media.
In general, complications are proportional to the amount of gland removed. Simple lobectomy is associated with a low risk of complication, whereas total thyroidectomy may cause more problems. In addition, children with malignant nodules tend to sustain more complications than children with benign disease.
Patient Education
Patient and family education should focus on the monitoring of symptoms. Parents of children with a strong family history, past exposure to head and neck irradiation, or a prior malignancy should be informed of the risk of thyroid cancer and the importance of a neck mass.
Postoperatively, parents and patients should monitor for recurrence of disease. If thyroid replacement is used, families should understand symptoms of insufficient or excessive dosing.
In the catastrophic event of nuclear fallout, all families within the vicinity should be educated about the possibility of thyroid cancer and take preventative measures if possible.
For excellent patient education resources, visit eMedicineHealth's Cancer Center and Thyroid and Metabolism Center. Also, see eMedicineHealth's patient education articles Cancer of the Mouth and Throat and Thyroid Problems.
-
A 12-year-old patient with an asymptomatic palpable thyroid nodule noticed upon routine physical examination.
-
Surgical specimen of a thyroid lobe with papillary carcinoma taken from a 12-year-old patient with an asymptomatic palpable thyroid nodule noticed upon routine physical examination.