Practice Essentials
Rectal prolapse refers to the circumferential extrusion of some or the entire rectal wall through the external anal sphincter. [1] Although, less common in Western societies, pediatric rectal prolapse is a relatively common benign disorder in children. However, without proper treatment, it can become a lifestyle limiting chronic condition. Most cases are self-limiting, with prompt resolution after conservative measures aimed at correcting the associated underlying process.
In children, rectal prolapse should always be considered a presenting sign of an underlying condition, and not a disease entity unto itself. Rectal prolapse starts as a mucosal extrusion from the mucocutaneous junction, which may eventually progress to full-thickness prolapse.
Rectal prolapse starts as a mucosal extrusion from the mucocutaneous junction, which may eventually progress to full-thickness prolapse. It is one of the first surgical entities ever described in medicine. (see the image below).
 Image of young patient with full-thickness rectal prolapse with multiple circular folds seen on exposed mucosa.
Image of young patient with full-thickness rectal prolapse with multiple circular folds seen on exposed mucosa.
Rectal prolapse and its etiology were first described in 1912 by Moschcowitz. Rectal prolapse in childhood was first highlighted in 1939 by Lockhart and Mummery [2] , who attributed the condition to malnutrition and careless nursing, but also acknowledged diarrheal disease and wasting illnesses as contributing factors. Lockhart-Mummery’s preferred operative treatment was linear cauterization of the prolapsed rectum, with recurrences treated by 5% phenol injection.
Loss of the normal sacral curvature that causes a vertical tube between the rectum and the anal canal has been described as a causative factor. Straining during defecation predisposes children with constipation, diarrhea, or parasitosis to prolapse, as does childhood laxative usage. About 60%-70% of patients have fecal incontinence. [3] The prolapse can spontaneously reduce or may require digital reduction.
Background
One classification of rectal prolapse divides the entity into true prolapse (protrusion of all layers of the rectum) and procidentia (herniation of only the mucosa). However, this classification is confusing and nonspecific and therefore, fallen out of use.
The most used classification for rectal prolapse was described in 1971 by Altemeier et al, who divided the entity into the following types [4] :
Type I Protrusion of redundant mucosa, termed false prolapse; usually associated with hemorrhoids
Type II Intussusception without sliding hernia of the cul-de-sac; it occupies the rectal ampulla but does not continue through the anal canal; the most common symptom is fecal incontinence, but solitary ulcers in the anterior rectal mucosa can be seen
Type III Complete, full-thickness rectal wall prolapse, associated with a sliding hernia of the Douglas pouch. It is the most frequent type.
Types II and III can be further subdivided into three degrees [5] :
First degree prolapse includes the mucocutaneous junction. The length of the protrusion from the anal verge usually is greater than 5cm.
Second degree prolapse occurs without involvement of the mucocutaneous junction. The length of the protrusion from the anal verge usually is between 2 and 5 cm.
Third degree prolapse is internal concealed or occult, and does not pass through the anal verge.
For the particular case of rectal prolapse occurring after the surgical correction of an anorectal malformation, [6] the entity can also be classified as:
Minimal, when the rectal mucosa was visible at the anal verge with Valsalva manoeuvre
Moderate, when there was a protrusion of the rectal mucosa inferior to 5 mm without the Valsalva manoeuvre; and
Evident, when the mucosal protrusion was greater than 5 mm without the Valsalva manoeuvre
The entity can also be categorized as circumferential,when it affects the rectum for 360o and hemi-circumferential, when the rectum is affected for less than 180o. [6] Most patients (77%) with rectal prolapse presenting after anorectoplasty can be successfully managed with conservative treatment. [6]
Anatomy
The anal canal extends cephalad from the anal verge to the anorectal ring. The rectum extends from this point to the sacral promontory.
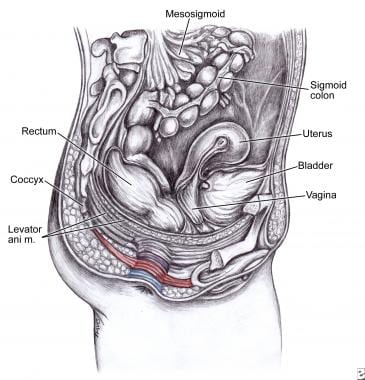
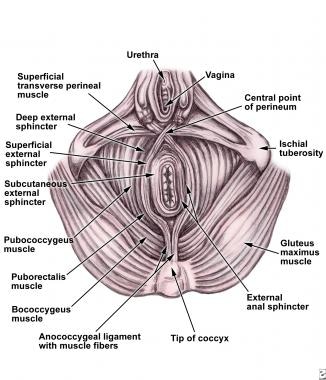
Upon histologic examination, the anal canal consists of mucosa, submucosa, and 2 muscular layers: the internal anal sphincter (IAS), which is a continuation of the circular muscle of the rectum, and [3] the external anal sphincter (EAS), which lies outside the IAS as an elliptic cylinder, continuous with the puborectalis muscle superiorly. The surgical anal canal includes this entire muscular sphincter mechanism (see the images below).
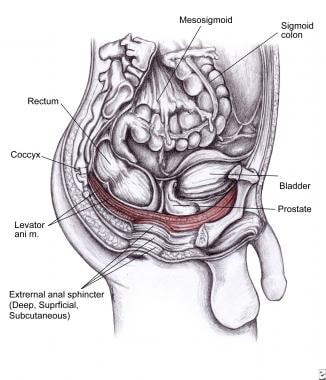 Levator ani muscle is shown in red. It includes ileococcygeus (stretches during defecation and labor), pubococcygeus (maintains integrity of pelvic floor), and puborectalis muscles (closes the anorectal canal as a sling).
Levator ani muscle is shown in red. It includes ileococcygeus (stretches during defecation and labor), pubococcygeus (maintains integrity of pelvic floor), and puborectalis muscles (closes the anorectal canal as a sling).
The many and varied procedures described for the treatment of rectal prolapse attempt to create a fixation of the anorectal mucosa to the submucosa, or the rectal wall to perirectal tissues.
Pathophysiology
Children are predisposed to rectal prolapse due to anatomic considerations: A pelvic floor defect with levator ani muscle diastasis and a deep endopelvic fascia represent the pathophysiology of the disease. Patients with rectal prolapse have lost the normal semi-horizontal rectal position; they also have weak muscle insertions to the pelvic walls and sacrum, an abnormally deep Douglas pouch and Houston’s valves absence in approximately 75% of infants younger than 1 year of age. [7] A redundant rectosigmoid and weaker / wider anal sphincter are common.
The normal resting tone of the anal sphincter decreases in response to rectal distention. In 1962, Porter found that patients with rectal prolapse have a profound and lengthy response and weakened tone of the levator ani muscles. [8] Whether this is a causative factor or a secondary finding is not clear, since the prolapse begins above the pelvic musculature. Most recently, information has suggested that rectal prolapse can be developed as a result of circumferential intussusception of the upper rectum and rectosigmoid colon. [7]
Rectal prolapse has been associated with a myriad of conditions, including:
-
Increased intraabdominal pressure due to straining (as often occurs in toilet training and constipation)
-
Parasitic disease (the most common cause of rectal prolapse in developing countries)
-
Neoplastic disease
-
Malnutrition (loss of ischiorectal fat pad) Worldwide, this is possibly the most common condition associated with pediatric rectal prolapse; the loss of ischiorectal fat reduces perirectal support
-
Ulcerative colitis
-
Ehlers-Danlos syndrome
-
Meningomyelocele
-
Pertussis
-
Surgical repair of anorectal malformation
-
Chronic constipation [11]
-
Neuromuscular disorders
-
Mental challenge [12]
-
Poor sacral root innervation (Spina bifida)
-
Bladder or cloacal exstrophy [13]
-
Scleroderma [14]
-
Hirschsprung disease (especially in ultrashort aganglionic segment, which acts as subocclusion, favoring prolapse) [15]
-
Rectal polyps (the polyp acts as a leading point) [16]
-
Cystic fibrosis [17]
-
Shigellosis in neonates [1]
-
Diarrheal disease (Infection by organisms that increases bowel motility) [7]
Cystic fibrosis (CF) deserves special attention as it may cause rectal prolapse in children. In the past, rectal prolapse was described in up to 20% of individuals with cystic fibrosis. However, current reports estimate an incidence of 3% of children with the disease. [18, 19] Potential mechanisms include bulky bowel movements, coughing paroxysms, and undernutrition. It is most frequently seen in toddlers, but it can occur at any age (triggered by cough). Clinical clues to cystic fibrosis include oily, malodorous, or floating stools; poor growth; wheezing or other respiratory symptoms; and digital clubbing. The absence of respiratory symptoms and normal findings upon physical examination do not necessarily exclude this diagnostic possibility. Sweat chloride test should be performed in order to rule out cystic fibrosis.
Most cases of childhood rectal prolapse occur in children younger than 4 years, with the highest incidence during the first year of life. Anatomic considerations related to this early presentation include the vertical course of the rectum along the straight surface of the sacrum, a relatively low position of the rectum in relation to other pelvic organs, increased mobility of the sigmoid colon, relative lack of support by the levator ani muscle, loose attachment of the rectal mucosa to the underlying muscularis, and absence of Houston valves, seen in about 75% of infants.
Etiology
Several predisposing factors have been identified, chronic constipation and straining being most common (52%). Other causes include diarrhea (15%), [9] rectal parasites, [20] malnutrition, [7] neuromuscular and pelvic nerve disorders, myelomeningocele, bladder and cloacal exstrophy, Hirschsprung disease, behavioral and psychological disorders, [21] high anorectal malformations, [22] cystic fibrosis, chronic respiratory infections and cough, [23] lymphoid hyperplasia, rectal polyps, and shigellosis. [24] Rectal prolapse has also been described in a case of Clostridium difficile –associated pseudomembranous colitis in a child. [22]
Hill et al. evaluated 39 patients for associated behavioral/psychiatric disorders. Of these, they identified 21 (54%) children with one or more behavioral or psychological disorders (ADHD, anxiety disorder, depression, encopresis/stool withholding). They concluded there’s a high rate (over 50%) incidence of behavioral and psychological disorders in older (3-18 years) children presenting with rectal prolapse. However, there is scant published literature identifying a high rate of BPD in prolapsed children. [25]
Broden and Snellman demonstrated by cineradiography, that the entity implies a circumferential intussusception of the rectum, with its origin three inches above the anal margin. [26]
Epidemiology
In adults, rectal prolapse is six times more common in females than in males. 75% of patients have history of constipation, which stretches the pelvic floor and the anal sphincter mechanism, predisposing them to the disease.
In children, incidence is higher during the first year of life, after which it becomes increasingly infrequent. It is slightly more common in boys than in girls and usually occurs between infancy and 4 years of age.
Rentea and St. Peter, proposed the following risk factors for rectal prolapse [7] :
-
Chronic constipation 28%
-
Neurologic or anatomic conditions 24%
-
Diarrheal disease 20%
-
No underlying cause 17%
-
Cystic Fibrosis 11%
As mentioned before, the cystic fibrosis group deserves special interest. An earlier review of CF revealed that 23% of patients with CF experienced rectal prolapse and that 78% of these patients experiencing rectal prolapse before the diagnosis of CF. This led to the recommendation that CF should be considered in a child with rectal prolapse of unknown etiology. [1]
Prognosis
Most cases reduce spontaneously. Otherwise, venous stasis, edema, and ulceration ensure. Longstanding or frequent recurrent prolapse episodes lead to proctitis.
Approximately 10% of patients who experience rectal prolapse as children continue to be symptomatic into adulthood. Over 90% of children who prolapsed during the first 3 years of life, respond to conservative treatment by age 6. It is important to achieve this early because the more episodes of rectal prolapse, especially, those cases that do not reduce spontaneously or have difficult reduction, demonstrate a lesser response to conservative management. [27] Spontaneous resolution is much less likely in children who develop their first episode of prolapse after age 4 years. After a surgical rectopexy, continence is achieved in 92% of patients. Resective procedures demonstrate lower recurrence rates.
Recovery of continence after surgery is not immediate, it may take up to a year.
Nwako et al reported a 100% success rate with the Lockhart-Mummery procedure, which involves packing the presacral space with gauze through a posterior approach, with excision of the prolapsed mucosa. [24]
Hight et al recommend linear cauterization of the rectal mucosa, with a 98% success rate in 72 patients. [28]
-
Image of young patient with full-thickness rectal prolapse with multiple circular folds seen on exposed mucosa.
-
Photograph of severe rectal prolapse with clinically significant edema and mucosal ulceration.
-
Picture of infant with full-thickness rectal prolapse. Severe edema and abundant mucus are seen on mucosal surface.
-
Levator ani muscle is shown in red. It includes ileococcygeus (stretches during defecation and labor), pubococcygeus (maintains integrity of pelvic floor), and puborectalis muscles (closes the anorectal canal as a sling).
-
Deep, superficial, and subcutaneous external sphincter.
-
Anatomy of internal and external anal sphincter mechanisms.
-
Image demonstrates mucosal prolapse, with radial folds seen on mucosa.
-
Diagram depicting clinical difference between true (full-thickness) prolapse (left), including all layers of rectum, with circular mucosal folds, and mucosa-only prolapse (right), in which radial folds are seen.
-
Thiersch procedure. Perianal subcutaneous sutures create mechanical barrier for prolapse.
-
Lomas and Cooperman modified the Thiersch procedure by performing right anterior and left posterior radial incisions, encircling the anus with a Marlex mesh stripe, and tying it around a finger placed on the anal canal. Care must be taken to avoid perforating the posterior vaginal or anterior rectal walls. The skin is closed, and the mesh left subcutaneously.
-
Ripstein procedure is designed to maintain normal posterior rectal curvature by attaching it to the presacral fascia, thus avoiding the straight tube that intussuscepts during straining. (A) Rectum is mobilized down to the coccyx. (B) Marlex mesh is placed around rectum while this is tensed upward and sutured to the presacral fascia with nonabsorbable sutures. Mesh loop must be loose enough to prevent postoperative constipation. (C) Sagittal view shows suspended rectum. (D) Peritoneum is closed with a continuous absorbable suture.
-
Intraoperative photograph of a 12-year-old girl with recurrent rectal prolapse and mucosal ulceration with profuse bleeding. She had a long sigmoid colon, which was resected; end-to-end anastomosis was performed. This photograph depicts anastomosed rectum fixed to presacral fascia with mesh. Non-absorbable sutures retain the mesh to the serosa. Note that the mesh is slightly loose to allow for child's growth. Uterus and its ligaments can be seen in front of rectum. Iliac vessels remain intact on each side.
-
Ivalon sponge procedure. (A) Rectum is mobilized. Meticulous hemostasis is mandatory to prevent hematoma that predisposes patient to prosthetic material infection. (B) Ivalon rectangular sponge made of polyvinyl alcohol is sutured to sacral periosteum. (C) Rectum is retracted upward, and sponge is wrapped around it and tied to the anterior sacral surface. A portion of the anterior rectal wall is left free to prevent luminal obliteration. (D) Peritoneum is closed with continuous absorbable suture.
Tables
What would you like to print?
- Overview
- Presentation
- DDx
- Workup
- Treatment
- Approach Considerations
- Manual Reduction
- Conservative Management
- Indications for Surgical Treatment
- Selection of Surgical Approach
- Injection Sclerotherapy
- Open Abdominal and Perineal Surgical Procedures
- Laparoscopic Repairs
- Robot-Assisted
- Other Treatments
- Surgical Complications
- Consultations
- Long-Term Monitoring
- Show All
- Medication
- Questions & Answers
- Media Gallery
- References