Background
Surgery for Dupuytren contracture generally should be performed on an affected metacarpophalangeal (MCP) joint if the contracture is 30° or greater. [1] Such contractures most likely cause some debilitation for the patient. Usually, a limited fasciectomy of the pretendinous cord is sufficient to establish normal function in the MCP joint.
The evaluation of a proximal interphalangeal (PIP) joint in Dupuytren disease differs from that of an MCP joint, and the prognoses differ as well. In PIP joint contractures, one should clearly define the method to be used in surgery and discuss with the patient his or her expectations and occupation, as well as activities the patient engages in that may require the use of his or her hands.
Various procedures are performed to treat Dupuytren disease. In a study using data from the PearlDiver nationwide administrative claims database for the period from 2012 to 2019 in the United States, Gordon et al reported the following frequency figures [2] :
-
Open fasciectomy (including palmar-only fasciectomy and fasciectomy involving one or more digits) - 60.7%
-
Collagenase Clostridium histolyticum (CCH) injection - 22.9%
-
Percutaneous needle aponeurotomy (PNA; also referred to as percutaneous needle fasciotomy [PNF]) - 10.1%
-
Open fasciotomy - 6.3%
Complications occur most often in patients who require total fasciectomy because of severe disease; McFarlane and McGrouther reported a complication rate as high as 17-19%. [3] During surgery, complications may include severing of the digital nerves, most often the neurovascular bundle; the inadvertent creation of a buttonhole through the skin flaps during their separation between the skin and the fascia; and circulatory compromise secondary to trauma to the digital arteries.
Postoperative complications include loss of flexion, hematoma, skin sloughing, infection, edema, and reflex sympathetic dystrophy (RSD; now commonly known as complex regional pain syndrome [CPRS] type 1). The most common postoperative PIP-joint complication is loss of flexion, which occurs in 6% of patients. The risk of trigger finger appears to be increased after treatment of Dupuytren contracture with fasciotomy or fasciectomy (though not CCH injection or PNA). [4]
The triad of hematoma, infection, and skin loss occurs in 3% of patients. Hematomas most often form in the palm, and they may be prevented by meticulous hemostasis, by removal of the tourniquet before the wound is closed, and by rapid evacuation of hematomas, which prevents necrosis of tissue and skin and decreases the risk of infection. Elevation of the hand can prevent postoperative edema.
RSD more commonly occurs in patients with extensive fasciectomies and, thus, more aggressive disease. This idiopathic pain syndrome, which often occurs 3-4 weeks after the surgery, consists of pain, edema, stiffness, and vasomotor disturbances. RSD occurs in 5% of patients, affecting 3% of men and 7% of women; treatment includes sympathetic blockade for symptomatic relief.
Indications
Indications for surgery depend on the patient’s requirements for hand function, the patient’s age, the severity of the contracture, and the joint or joints involved. Generally, surgery is not necessary until contracture occurs. [1]
MCP flexion contracture
MCP flexion contracture of 30º or more is an accepted criterion for surgical correction. [1] At this point, flexion becomes functionally significant for most people; even in the ulnar digits where there is some carpometacarpal (CMC) extension range. MCP-joint flexion contracture of up to 60º has been easily correctable.
PIP flexion contracture
PIP flexion contracture of any degree constitutes an indication for surgery. A flexion contracture of the PIP joint quickly becomes more difficult to correct because of shortening of collateral ligaments and fibrosis and adherence of periarticular structures such as the volar plate.
Adequate correction may require joint release after the resection of contracted, diseased tissue. Shortening of neurovascular bundles can also limit extension after release in long-standing PIP contracture. Because of these technical challenges, complete correction is less common, and persistence of joint flexion contracture is more likely.
Other factors in surgical intervention
Neurovascular compromise due to Dupuytren disease is an indication for intervention. Secondary involvement of periarticular structures may also require correction.
Thumb flexion deformities are well tolerated and less functionally significant; therefore, they are less urgently corrected. However, significant first web space contracture involving the thumb warrants surgical intervention.
Technical Considerations
Procedural planning
Some surgeons have maintained that early surgical intervention is more likely than delayed surgery to yield excellent results, whereas others have maintained that with natural disease progression, radical prophylactic palmar clearance potentiates the need for revisions. Surgical techniques for Dupuytren disease include closed (or percutaneous) and open fasciotomy, regional (or limited) palmar fasciectomy, and radical (or total) fasciectomy. [5] (See the images below.)
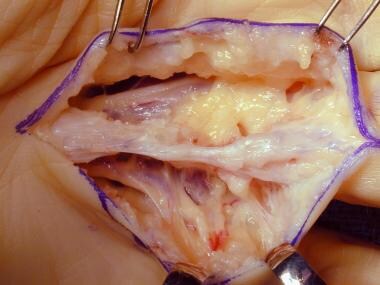
 Dissection of spiral cord in the hand of a patient with Dupuytren disease. Image courtesy of Lawrence Yeung, MD.
Dissection of spiral cord in the hand of a patient with Dupuytren disease. Image courtesy of Lawrence Yeung, MD.
 Dissection of the spiral cord in a patient with Dupuytren disease. Image courtesy of Lawrence Yeung, MD.
Dissection of the spiral cord in a patient with Dupuytren disease. Image courtesy of Lawrence Yeung, MD.
Two important considerations are adequate release of longitudinal tension and the management of involved skin. Other important decisions involve selection of the incisions required and any special method of wound closure employed. The patient’s age and functional requirements and the potential for recurrent disease also impact decisions on the extent of surgery.
Total fasciectomy prevents recurrence because the entire diseased fascia is removed, along with the central, lateral, spiral, natatory, and retrovascular cords, as well as any normal fascia that may later be affected.
As stated above, a limited fasciectomy of the pretendinous cord is usually sufficient to establish normal function in the MCP joint. McFarlane favored a regional fasciectomy of the pretendinous cord to prevent recurrence of Dupuytren contracture. [3] For longitudinal incisions, Z-plasties or multiple Y-to-V advancements may adequately close the wound. A transverse incision may be necessary for more extensive disease; in such cases, a full-thickness skin graft may be required for the defect, or the wound may have to heal secondarily. [6]
Given the difficulty of correcting severe disease, fasciectomy is indicated for any amount of PIP joint contracture. Unfortunately, recurrence is common. The procedures of choice in the PIP joint are dermatofasciectomy and total fasciectomy.
Outcomes
The patient will likely judge his or her own result subjectively, with the perception of functional improvement as an endpoint. Andrew found that MCP contracture invariably was corrected (86% excellent), whereas good results for PIP contracture were less frequent (40% excellent result in middle and ring fingers; 20% in small fingers). [7] Excellent results in the correction of secondary contracture of the distal interphalangeal (DIP) joint occurred in approximately 50% of cases.
In a study by Donaldson et al, the extent of a patient’s preoperative deformity was found to be a significant predictor of complete intraoperative correction in Dupuytren contracture. [8] In addition, the extent of preoperative deformity and intraoperative correction were significant predictors of loss of surgical correction after surgery. The investigators prospectively studied 52 patients who underwent primary fasciectomy for Dupuytren disease, to determine whether preoperative contracture and the amount of intraoperative correction could predict postoperative outcome.
In this study, 42 MCP joints were treated, of which 41 achieved full intraoperative correction; 37 had full correction at 6 months' follow-up. [8] Of the 58 PIP joints treated surgically, full intraoperative correction was obtained in 35, and 13 had complete correction at 6 months' follow-up.
In another study, Villani et al found that full-thickness skin grafts prevented recurrence of Dupuytren contracture in 20 out of 23 hands after more than 8 years' follow-up. [9] Of the 18 patients who underwent dermofasciectomy and skin grafting, 13 received skin grafts on one hand, and five patients received grafts on both hands. The authors noted that because recurrence is difficult to predict, primary skin grafting remains controversial and that indications for the skin-grafting procedure are more definite once recurrence has taken place.
Selles et al evaluated the 5-year results of percutaneous aponeurotomy with lipofilling (PALF; n = 31) versus limited fasciectomy (n = 21) for primary Dupuytren contracture, with a special focus on recurrence (defined as either having a 20º or greater worsening in contracture relative to week 3 or as having undergone a secondary procedure for a new or worsening contracture). [10] At 5 years, 74% of the PALF joints had a recurrence, compared with 39% of the limited fasciectomy joints. When recurrence was redefined as a worsening of at least 30º in total extension deficit, the corresponding figures were 77% and 32%. Total extension deficit was worse for PALF-treated digits (53º vs 31º).
In a study of 350 patients treated for Dupuytren contracture (848 interventions), Leafblad et al evaluated the outcomes and direct costs of three treatments: PNA (444 interventions), CCH injection (272), and open fasciectomy (132). [11] The 2-year reintervention rates were 24% for PNA, 41% for CCH injection, and 4% for fasciectomy; the corresponding 5-year rates were 61%, 55%, and 4%. The standardized direct costs were $624 for PNA, $4189 for CCH injection, and $5291 for fasciectomy. With all reinterventions included, the cumulative costs per digit at 5 years were $1540 for PNA, $5952 for CCH injection, and $5507 for surgery.
A systematic review and meta-analysis by Liechti et al (N = 1051; minimum average follow-up, 3 mo) examined 11 comparative studies on outcome differences between CCH injection (n = 619) and limited fasciectomy (n = 432) for Dupuytren disease. [12] Residual contracture was significantly higher after CCH injection than after limited fasciectomy (27.8º vs 16.2º), as was the recurrence rate (25.8% vs 9.3%); however, the rate of severe complications was significantly lower (0.3% vs 7.3%).
-
Dissection of spiral cord in the hand of a patient with Dupuytren disease. Image courtesy of Lawrence Yeung, MD.
-
Dissection of the spiral cord in a patient with Dupuytren disease. Image courtesy of Lawrence Yeung, MD.
-
Visible cord characteristic of Dupuytren disease with planned markings for surgical release.
-
Dissection of a diseased cord.