Practice Essentials
Primary spinal tumors fall into a distinct category because their timely diagnosis and the immediate institution of treatment have an enormous impact on the patient's overall prognosis and hope for a cure. [1, 2]
Generally, with spinal pathology, problems that arise are either chronic problems related to degenerative disease or deformity or acute manifestations of traumatic sequelae. When considering tumors of the spine, one must consider the different tissue types around the spinal column. The presence of neural tissue, meningeal tissue, bone, and cartilage makes any of these tissue types a possible nidus for neoplastic change. Also, metastatic lesions may spread to the spine from distant primary tumor sites via hematogenous or lymphatic routes.
Primary nonlymphoproliferative tumors of the spine are uncommon and make up fewer than 5% of bone neoplasms; the annual incidence of primary spine tumors is in the range of 2.5-8.5 per 100,000 population. Metastatic disease of the spine is much more common. Approximately 40-80% of patients who die of cancer have bony metastases at the time of death, with the spine being the most common metastatic skeletal location.
Neoplastic disease, however, can present with back pain that is indistinguishable from back pain resulting from more benign causes. Therefore, the physician caring for patients complaining of back pain is faced with the challenges of (1) distinguishing benign causes from those that can be neurologically or systemically devastating and (2) prescribing the appropriate treatment.
This distinction sometimes can be difficult to make because of the complicated architecture of the spine (see Anatomy). The physician must consider differential diagnoses of degenerative processes, infections, muscular strains, neurologic impingements, and, finally, neoplastic processes. With thorough history taking, physical examination, and diagnostic imaging, the physician can acquire enough information to make the correct diagnosis in an efficient manner.
The relevant anatomy is frequently the limiting factor in determining contraindications for surgical excision of spine tumors. (See Treatment.) The morbidity of the tumor, the tumor's malignant potential, and the patient's overall prognosis must be compared to the morbidity and potential mortality of radical resection of a tumor near the spinal cord, the aorta, or the heart. The degree of associated blood loss and the overall health of the patient also must be taken into consideration in considering a resection. Oncologic staging aids the surgeon in deciding what surgical margin provides the best chance for complete tumor resection and possible cure.
Anatomy
The spine consists of 33 vertebrae that form the bony spinal column. The spinal column can be divided into the cervical, thoracic, lumbar, and sacrococcygeal regions. Although morphologically distinct, each vertebra in the subaxial cervical, thoracic, and lumbar spine has a consistent architecture, consisting of a vertebral body, pedicles, laminae, and spinous and transverse processes. Flexibility of the spine is produced by the intervertebral disk and facet joints. The intervertebral disk consists of a gelatinous core held in place by a fibrous ring. The facet joints cascade along the posterior spine and allow motion between the segments.
The bony canal provides protection and support to the fragile spinal cord and nerve roots within the dural sac. The soft tissues surrounding the bony spine vary by location from the thick dorsal paraspinous musculature to the vital organs and vessels within the mediastinal, thoracic, peritoneal, and retroperitoneal spaces.
Pathophysiology
In general, tumors (neoplasms) are considered to be either primary or metastatic. Primary tumors arise from the tissue itself— for example, a chordoma is a tumor formed from tissues of the spinal column. In contrast, metastatic tumors form in other tissues and either directly invade nearby structures or travel distantly through the body via the blood stream or lymphatic drainage. The spine is highly vascularized, with many slow-flowing channels, and is in intimate proximity with large venous and lymphatic systems; these characteristics make the spine a fertile location for metastatic disease. Approximately 97% of the tumors found in the spine are metastatic. [3, 4]
Local destruction of the bony spinal column can lead to pain as a consequence of instability of the spine. Similarly, tumors may expand out of the bony spine and impinge on the neural elements. Injury to the neural elements can present as pain, altered sensation, muscular weakness, spasticity, or other neurologic derangements. Metastatic tumors can travel to the spine via the epidural venous plexus, growing in the epidural space and causing neurologic symptoms. Primary tumors of the neural elements may be transmitted through the cerebrospinal fluid and cause similar compression of the neural elements from within the thecal sac itself. [4]
Epidemiology
Primary tumors of the spine are far rarer than metastatic tumors: In the United States, there are an estimated 7500 new cases of primary spinal tumors per year, compared with 90,000 metastatic cases. [5] Of these rare tumors, hemangioma is the most common, with benign lesions accounting for approximately 30% of all cases. Most of these are asymptomatic and may be found incidentally on imaging of the spine. Plasmacytoma is the most common malignant tumor of the spine, accounting for 20-30% of cases.
As many as 10% of cancer patients may develop symptomatic metastases to the spine. [6, 4] Adenocarcinomas of the breast, prostate, and lung are among the most common cancers metastasizing to the spine, with a slightly higher prevalence of bony metastases in men. The latter is likely due to the slightly higher prevalence of prostatic disease as compared with breast disease. [4]
Prognosis
Chang et al conducted a study to evaluate local control rate and to identify prognostic factors after stereotactic radiosurgery for treatment of primary malignant spinal tumors (N = 29; median age, 46 y; age range, 11-68 y). [7] Histologic diagnoses included chordoma (n = 1), chondrosarcoma (n = 5), osteosarcoma (n = 3), synovial sarcoma (n = 3), plasmacytoma (n = 2), Ewing sarcoma (n = 2), malignant peripheral nerve sheath tumor (n = 2), and malignant fibrous histiocytoma (n = 1). Mean follow-up was 50 months (range, 8-126).
Initial treatment consisted of surgical resection (n = 25) or percutaneous biopsy (n = 4). [7] Stereotactic radiosurgery was used as primary treatment (n = 14) or as salvage treatment for progressive lesions (n = 15). Eleven patients had undergone previous conventional external-beam radiation therapy before stereotactic radiosurgery. Median tumor volume was 14 cm3 (range, 2.0-235). Delivered radiation doses were 12-50 Gy in two to six sessions. The mean radiation dose converted into a biologic effective dose (BED) was 60 Gy (range, 43-105).
Mean overall survival was 84 months for chordoma patients and 104 months for sarcoma patients. [7] The investigators found no factors that affected overall survival. The mean local progression-free survival was 56 months for chordoma patients and 73 months for sarcoma patients. The recurrent mode of presentation was predictive of local progression of spinal sarcomas. For patients with chordoma, no factors were found to correlate with local recurrence.
Kose et al conducted a study of the effect of early rehabilitation on neurofunctional outcome after surgery in children with spinal tumors. [8] The investigators reviewed medical charts and radiographic records of 70 pediatric patients (age range, 1-17 y) who underwent surgery for the removal of spinal tumor. The patients received rehabilitation treatment beginning an average of 4 days (range, 2-7) after surgery and continued for an average of 10 days (range, 7-23).
Results were assessed on the basis of scoring on the Modified McCormick Scale, the Functional Independence Measure for Children, the American Spinal Injury Association Impairment Scale, and the Karnofsky Performance Status Scale. [8] Sensory function, motor function, and activity of daily living were significantly improved for the patients who received early rehabilitation. Tumor setting, the level of localization, and the patients' clinical symptoms had no bearing on neurofunctional outcomes.
-
Spinal tumors. Chordoma histology.
-
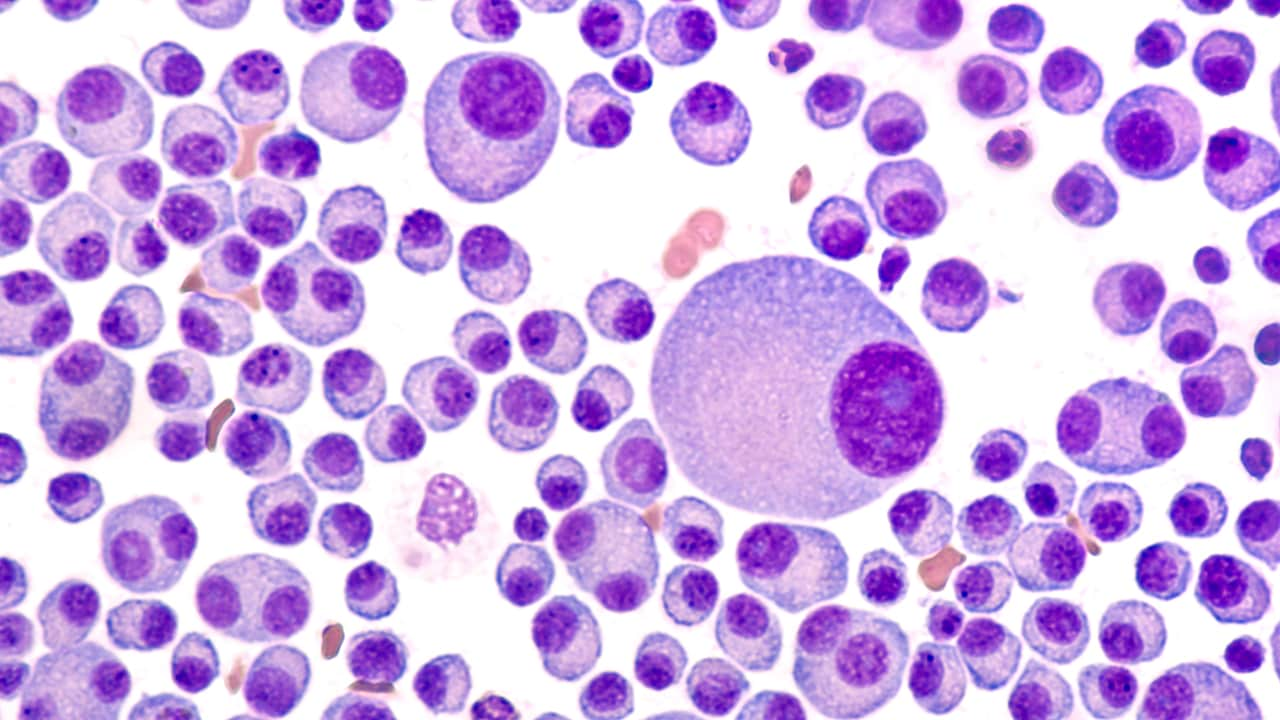
Spinal tumors. Higher magnification of chordoma histology demonstrates characteristic physaliferous cells.
-
Spinal tumors. Aneurysmal bone cyst histology.
-
Spinal tumors. Coned-down view of lateral thoracic spine in patient with chondrosarcoma.
-
Spinal tumors. Axial CT scan at level of chondrosarcoma seen on previous x-ray image.
-
Spinal tumors. T2-weighted MRI scan of chondrosarcoma in same patient.
-
Spinal tumors. Photograph of patient's back at time of surgery, exhibiting course of definitive incision to excise chondrosarcoma en bloc with previous biopsy tract included with resection.
-
Spinal tumors. Histology of chondrosarcoma at 40 times magnification.
-
Spinal tumors. Lateral cervical spine x-ray demonstrating osteoblastoma in posterior elements of C3 and C4.
-
Spinal tumors. MRI of osteoblastoma in posterior elements of C3 and C4 seen on previous x-ray image.
-
Spinal tumors. Histology of osteoblastoma at low magnification.
-
Spinal tumors. Higher magnification of osteoblastoma.
-
Spinal tumors. Coned-down view of hemangioma in thoracic spine.
-
Spinal tumors. Axial CT scan of hemangioma in lumbar vertebra.
-
Spinal tumors. Axial CT scan of thoracic vertebra, which demonstrates nidus of osteoid osteoma in posterior elements.