Overview
Regional anesthesia refers to the focused delivery of anesthetic agent(s) to a given part of the body. Regional anesthesia is used extensively for various purposes, including as a primary anesthetic technique for surgery, as an analgesic modality to manage pain in the perioperative period, and as an analgesic modality for various other forms of acute and/or chronic pain. This article will focus on the use of regional anesthesia as a postoperative analgesic technique for orthopedic surgery.
Regional anesthesia can be broadly divided into several categories:
-
Neuraxial anesthesia, including intrathecal (aka “spinal”) and epidural techniques
-
Upper and lower extremity blockade for somatic analgesia
-
Autonomic plexus blockade for visceral analgesia
-
Peripheral nerve blockade for somatic analgesia
-
Localized wound infiltration
-
Topical anesthetics
The use of perioperative regional anesthesia has many possible advantages. Regional anesthesia can reduce operative anesthetic requirements and in some cases allow avoidance of general anesthesia altogether. This can be beneficial to a variety of patient populations, including those at risk for cognitive dysfunction after general anesthesia. [1] The use of regional anesthetic and analgesic techniques can offer superior overall pain control and reduced postoperative opioid requirements. [2, 3] In addition, in certain operations, such as total hip arthroplasty (THA), the use of regional anesthesia may be associated with certain positive trends such as reduced blood loss and reduced rates of deep vein thrombosis (DVT). [3, 4]
Various regional analgesia techniques exist that can be used to promote postoperative pain relief. These methods can be categorized into neuraxial local analgesics and opioids, peripheral nerve blocks, and wound infiltration.
Neuraxial Analgesia
Intrathecal analgesia
Intrathecal (IT), often referred to as “spinal,” anesthesia refers to the delivery of anesthetic agents to the subarachnoid layer of the spinal column into cerebrospinal fluid (CSF) surrounding the spinal cord. Commonly used IT analgesic agents specifically in the perioperative setting include local anesthetics, opioids, and adjuncts such as epinephrine.
Opioids administered to the IT space can offer effective postoperative analgesia. These agents bind with opioid receptor sites in the dorsal horn of the spinal cord, resulting in modulation of pain signals at the spinal cord level. IT opioids can be administered as an adjunct to general anesthesia (e.g., for scoliosis surgery) or combined with local anesthetics and administered during spinal anesthesia (e.g., for total hip arthroplasty). For IT morphine, the onset of analgesia is 30–60 minutes, and the duration of analgesia is 18–24 hours, depending on the dose.
Adverse effects of IT opioids include nausea, pruritus, urinary retention, and respiratory depression. Respiratory depression from IT morphine peaks at approximately 7–9 hours after surgery and is dose dependent. The incidence of respiratory depression in one retrospective study was 0.36%. [5] The incidence of nausea and vomiting for IT morphine is approximately 20% and peaks at approximately 4 hours. Pruritus occurs in approximately 40% of patients, but severe cases (requiring treatment) occur in about 9%. [6] The incidence of urinary retention is unclear because many patients receive preemptive urinary catheterization, but it is estimated to occur in 10–40% of patients. [6]
IT anesthesia is typically delivered by a single injection (i.e., a “spinal”). The advantages of IT opioids for analgesia, especially if spinal anesthesia is already planned, include its simplicity, lack of need for catheter care or pumps, low cost, and easy supplementation with low-dose patient-controlled analgesia (PCA) opioids as needed. The main disadvantages of this technique are limited duration of action (in comparison to catheter-based techniques) and the adverse effects discussed above. More frequent respiratory monitoring is recommended because of the risk of late-onset respiratory depression. [7]
Contraindications to use of IT anesthesia include heparinization or other coagulopathy, local or systemic infection, and morphine allergy.
Typical dosing regimens recommended in the literature are as follows:
-
Total hip arthroplasty – Morphine 100-200 mcg
-
Total knee arthroplasty – Morphine 200-300 mcg
-
Spine fusion, scoliosis surgery – Morphine 300 mcg or 3-5 mcg/kg
In the setting of knee and hip arthroplasty, the author limits the dose to 150 mcg, used in conjunction with multimodal analgesics (e.g., celecoxib, acetaminophen, gabapentin) and peripheral nerve blocks. Using a lower dose results in lower incidence of nausea, itching, and respiratory depression.
Epidural analgesia
Epidural analgesia refers to the delivery of anesthetics to the epidural space for purposes of pain control. Commonly used agents include opioids and local anesthetics. Opioids can be administered by bolus or infusion. Adverse effects are the similar to those of IT opioids (see Intrathecal analgesia, above). Epidural local anesthetics, typically diluted solutions of bupivacaine or ropivacaine, are typically administered by infusion. Adverse effects of epidural local anesthetics include urinary retention, motor blockade (i.e., weakness), and a “sympathectomy” mediated decrease in blood pressure. Epidural local anesthetics and opioids are frequently combined in lower dosages to decrease the risk of each drug's associated adverse effects.
The duration of epidural infusion depends on several factors. To varying degrees depending on drug-concentration and patient characteristics, epidural infusions may complicate patient mobility, voiding, and rehabilitation therapy. Additionally, the infectious risks for epidural catheters is thought to increase with time. Generally speaking, epidural catheters are removed within a matter of days to minimize microbial colonization of indwelling catheters. Moreover, the risk of epidural hematoma increases in the presence of anticoagulants and drugs known to affect hemostasis (i.e., non-steroidal anti-inflammatory drugs [NSAIDs]). Use of such drugs are not contraindicated per se, but must be used with caution, ideally aligned with practice guidelines such as those published by the American Society for Regional Anesthesia (ASRA). [8]
A wide variety of dosing regimens for regional anesthesia are in use. Opioid and local anesthetic drugs can be combined in the same infusion. Intravenous (IV) PCA opioid can be administered as an adjunct to local anesthetic infusions.
Some common examples of epidural infusion components include:
-
Morphine (0.01%) – 5–10 mL/h
-
Fentanyl (0.001%) – 5–10 mL/h
-
Hydromorphone (0.005%) – 5–10 mL/h
-
Bupivacaine (0.05-0.1%) – 5–10 mL/h
-
Ropivacaine (0.1%) – 5–10 mL/h
It should be noted that the interplay and additive effect of neuraxial and IV opioids is difficult to fully predict. For this reason, practitioners may consider pure local anesthetic epidural solution when frequent dosing of adjuvant IV opioid (i.e., opioid PCA) will be used.
An extended-release form of morphine is available for epidural use (DepoDur; morphine sulfate extended-release liposome injection; Endo Pharmaceuticals Inc, Chadds Ford, Pa). DepoDur is reported to provide 48 hours of analgesia. This drug possess an adverse effect profile common to epidural opioids. DepoDur use has been reported in patients undergoing hip replacement [9] and knee replacement. [10]
Treatment of epidural or IT opioid-induced adverse effects includes the following:
-
Urinary retention – Urinary catheterization
-
Pruritus – use of mixed opioid agonist-antagonists (e.g. nalbuphine 2 mg IV) or naloxone 0.1–0.2 mg IV or subcutaneous (SC) route is effective, although may mitigate analgesic effects of IT opioids. Antihistamine drugs such as diphenhydramine (Benadryl; McNeil-PPC, Inc, Fort Washington, Pa) 25–50 mg IV or intramuscular (IM) route is often used, which is likely effective by virtue of sedation as opioid-induced pruritus is not known to be histamine mediated.
-
Nausea/vomiting – Metoclopramide (Reglan; Baxter Healthcare Corp, Deerfield, Ill) 10 mg IV; ondansetron (Zofran; GlaxoSmithKline, Research Triangle Park, NC) 4 mg IV; or naloxone 0.1–0.2 mg IV/SC
-
Respiratory depression – Naloxone 0.2–0.4 mg IV
Neuraxial blocks and anticoagulation
ASRA has published its fourth edition of recommendations regarding the practice of regional anesthesia including neuraxial techniques in the presence of anticoagulation. [8] These recommendations have evolved with continued safety data collection as with the advent of new generations of anticoagulation therapy, such as direct thrombin inhibitors (e.g. Xarelto©; rivaroxaban; Janssen Pharmaceuticals Inc., Titusville NJ) and direct factor Xa inhibitors such as fondaparinux.
The most commonly encountered scenario related to this topic involves the administration of a neuraxial anesthetic (epidural or spinal) in the context of planned perioperative DVT prophylaxis. Perioperative DVT prophylaxis is a highly variable practice and may involve a variety of techniques, including non-pharmacologic strategies such as early ambulation and mechanical techniques (e.g., pneumatic sequential compression devices). Relevant to this article, commonly used pharmacologic agents include:
-
Aspirin
-
Unfractionated Heparin (UFH)
-
Low Molecular Weight Heparin (LMWH) including enoxaparin and fondaparinux
-
Vitamin K antagonists (VKA) including warfarin
-
Direct thrombin inhibitors including rivaroxaban and apixaban
Placement of a neuraxial anesthetic (epidural or spinal) in the context of planned pharmacologic DVT prophylaxis should be done with knowledge of widely accepted clinical guidelines and practice recommendations. A condensed, pertinent summary from the ASRA guidelines as it pertains to this specific anesthetic technique appears in Table 1 below.
Table 1. (Open Table in a new window)
Hold Before Placement / Removal |
Dose After Placement / Removal |
|
NSAIDs |
No restrictions |
No restrictions |
Clopidogrel |
5–7 days |
Immediate (no loading dose) |
Low-Dose Subcutaneous UFH |
4–6 hrs |
1 hr |
Treatment UFH |
IV 4–6 hrs SC 12 hrs |
1 hr |
Low-Dose LMWH |
12 hrs |
4 hrs |
Treatment LMWH |
24 hrs |
4 hrs |
Warfarin |
INR ≤ 1.4 |
immediate |
Rivaroxaban ≤10 mg/d |
26 hrs |
6 hrs (avoid indwelling catheters) |
Rivaroxaban >10 mg/d |
44–65 hrs |
6 hrs (avoid indwelling catheters) |
Apixaban 2.5 mg BID |
26–30 hrs |
6 hrs |
Apixaban >5 mg/d (and/or age >80 yrs / Cr >1.5 mg/dL / wt < 60 kg) |
40–75 hrs |
6 hrs |
Table 1. Selected Recommendations for Management of Neuraxial Anesthetic Technique in the Setting of Pharmacologic Prophylaxis of Deep Vein Thrombosis. Adapted from: “Regional Anesthesia in the Patient Receiving Antithrombotic or Thrombolytic Therapy: American Society of Regional Anesthesia and Pain Medicine Evidence-Based Guidelines (Fourth Edition)” Regional Anesthesia and Pain Medicine. 2018 April. 43(3), 263-309.
Peripheral Nerve Blocks
Peripheral nerve blockade is an effective and safe technique for providing post-operative analgesia and, in many cases, a surgical anesthetic. Commonly used local anesthetics include long-acting medications such as ropivacaine and bupivacaine, with durations of action of approximately 7–15 hrs and 9–20 hours, respectively. [11] Certain additives have been demonstrated to prolong the duration of nerve blocks. For example, the addition of dexamethasone or methylprednisolone may provide an additional several hours of analgesia. [12, 13] The addition of dexmedetomidine to peripheral nerve blocks has been shown to significantly prolonged analgesia, although the mechanism of this effect remains unclear. [14]
The longest duration of action for peripheral nerve blocks is achieved by perineural catheter placement, with continuous infusion or intermittent bolus of local anesthetic. Peripheral nerve catheters may be left in for several days, although it should be noted the risk of abscesses requiring surgical drainage increases the longer a peripheral catheter is left in place. [15]
Advantages of peripheral nerve blockade include avoidance of sympathectomy-induced decrease in blood pressure, as well as of opioid-related adverse effects such as urinary retention, nausea, or itching. However, some degree of motor block is observed with the sensory block. This result may limit the usefulness of some peripheral blocks in certain situations. For example, prolonged femoral blocks are a good choice for pain control when postoperative ambulation is avoided (e.g., anterior cruciate ligament [ACL] reconstructions). However, such a block is a poor choice in knee arthroscopy because the quadriceps motor block would prevent safe ambulation. Successful use of nerve blocks depends not only on clinical knowledge of the site of incision innervation but also on knowledge of the innervation for the underlying bone and muscular tissue.
Serious adverse effects of peripheral nerve blocks are rare. In addition to infection (see above), adverse effects include local anesthetic toxicity, complications from needle placement, and unintended spread of local anesthetic.
Local Anesthetic Systemic Toxicity (LAST) can occur from a variety of mechanisms including inadvertent intravascular injection, delayed systemic absorption/intravenous update, and repeated high-dose topical and mucosal administration. [16] In addition to iatrogenic causes, certain patient characteristics increase the risk of LAST, including extremes of age, end-organ dysfunction, and pregnancy. [17, 18, 19, 20] Symptoms of LAST range from tinnitus and dizziness to convulsions and cardiac arrest. Familiarity with detection and treatment of this life-threatening complication is essential before administering a regional anesthetic.
Complications of needle placement can include hematomas, tissue bruising, and nerve injury ranging from paresthesia to self-limited dysesthesia to permanent nerve dysfunction. The incidence of serious nerve injury following peripheral nerve block is so rare that exact risks are difficult to determine. Transient resolving paresthesia in the days after peripheral nerve block may occur in up to 8–10% of cases [21] with virtually all being self-limited. [22] The incidence of any permanent neurologic sequelae from peripheral nerve blockade is reported as 0.01%. [23] The mechanism for peripheral nerve blockade is thought to be inadvertent intrafascicular injection, and strategies to minimize this include minimizing patient sedation to detect severe pain during injection, standardizing equipment and techniques to ensure “easy compliance” during injection, and use of ultrasound and evoked motor responses when possible to inform clinical decision making. [24]
Unintended spread of local anesthetic can cause neural blockade of nearby, non-targeted nerves. Common examples of this include phrenic nerve palsy and Horner’s syndrome during certain brachial plexus blockade techniques (i.e., interscalene block) and motor weakness during adductor canal blockade. [25, 26] Though unintentional, these occurrences are not unexpected and should be considered as part of medical decision making when planning a regional anesthetic.
Brachial plexus blocks
The brachial plexus can be anesthetized at sites above the clavicle (interscalene and supraclavicular approaches) or below the clavicle (infraclavicular and axillary approaches). The interscalene brachial plexus block anesthetizes the brachial plexus (C5-T1 distribution) and due to proximal and superficial spread of injectate also anesthetizes supraclavicular branches of the cervical plexus. [27] For this reason, it is a popular choice for shoulder and upper arm surgery. However, interscalene brachial plexus blocks often inadequately anesthetize the C8 and T1 nerve roots, and for this reason it is generally a suboptimal approach for lower arm and hand surgery. The supraclavicular approach can result in successful coverage of the arm and hand. The infraclavicular or axillary approaches are used for surgery of the elbow, lower arm, and hand.
Interscalene and supraclavicular brachial plexus blockade have particular risks that set them apart from other approaches. Phrenic nerve dysfunction occurs in 100% of interscalene blocks and 25–50% of supraclavicular blocks. [23, 28] Consequently, these blocks may not be well tolerated in patients with preexisting respiratory compromise. Research suggests that pulmonary function can be preserved by using lower-volume, lower-concentration, and lower-level (C7) ultrasound-guided approaches. [29, 30] Case reports describe epidural [31] or IT injections [32] with interscalene blocks. Pneumothorax has been reported to occur in up to 5% of supraclavicular blocks, but the incidence is probably now well below 1% with the advent of ultrasound-guided techniques. Horner syndrome and hoarseness commonly occur from spread of anesthetic to the sympathetic chain and recurrent laryngeal nerve, respectively.
In 2018, the Federal Drug Administration (FDA) approved the use of a long-acting, liposomal bupivacaine forumation (Exparel®) for use in interscalene brachial plexus block. This medication provides sustained pain-relief for up to 72 hours. At present, Exparel® is not approved for use in other peripheral nerve blocks. [33]
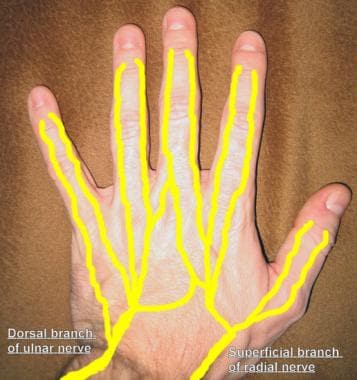
Digital nerve blocks
For hand surgeries, more distal blocks can also be performed to provide analgesia. Block of the radial, median, and ulnar nerves at the wrist or block of the digital nerves of the fingers (see the images below) can be performed.
Lower extremity blocks
Femoral Nerve
The knee joint is innervated by the femoral (anteriorly), sciatic (posteriorly), obturator (medially), and lateral femoral cutaneous nerves (laterally). Femoral nerve blocks are frequently used for analgesia after knee surgery; however, the degree of analgesia depends on the amount of surgical extension into other nerve distributions. Thus patients undergoing arthroscopic ACL and patellar surgery obtain excellent pain relief after femoral block, whereas patients undergoing knee replacement surgery frequently have severe posterior pain of sciatic origin. Unless the knee is properly braced, weight bearing and ambulation may need to be restricted until quadriceps function recovers in patients with femoral nerve blocks.
Sciatic nerve
The sciatic nerve can be blocked from a variety of approaches, including transgluteal (e.g., the classic Labat technique), subgluteal, anterior, and popliteal fossa. Popliteal fossa blocks are performed to provide analgesia after foot and ankle surgery. At the level of the popliteal fossa, the sciatic nerve divides into the tibial and common peroneal nerves. The advantage of a popliteal fossa block over standard sciatic blocks is that hamstring function is maintained. For surgeries involving the saphenous dermatome along the medial aspect of the lower extremity, popliteal fossa blocks are often supplemented with a saphenous nerve block.
Other
For some foot or toe surgeries, more distal nerve blocks can also be performed to provide analgesia. Blocks of the deep peroneal, superficial peroneal, tibial, sural, and saphenous nerves can be performed at the ankle level. Alternatively, blocks of the digital nerves of the toes can be used.
Wound Infiltration
The infiltration of wounds with local anesthetics not only provides analgesia, but, when performed ahead of surgery, can be part of a more comprehensive plan for preemptive analgesia. Preemptive analgesia, in theory, reduces local inflammatory responses, decreases central sensitization, and in turn aims to reduce risk for development of pathologic pain. [34] Local anesthetics have been administered incisionally, intraarticularly, and as higher volume infiltration of the wound.
Incisional
Local anesthetic can be administered in skin incision sites or on bone wounds (iliac crest graft sites). Bupivacaine or ropivacaine provides approximately 6 hours of analgesia. Incisional catheters and local anesthetic infusions have been reported for use in general, thoracic, and cardiac surgeries, but appear to be less frequently reported in orthopedic surgery. In 2011, the FDA approved bupivacaine liposome injectable suspension (Exparel®) for use in surgical pain. It is in effect a slow-release form of bupivacaine, which can provide analgesia for up to 72 hours and has repeatedly demonstrated a reduction in postoperative opioid consumption. In 2018, the Federal Drug Administration (FDA) approved Exparel® for use in interscalene brachial plexus nerve blocks. At present, Exparel® is not approved for other peripheral nerve blocks. [33]
See the image below.
Intra-articular local anesthetics
Single intra-articular injections of local anesthetics have been used for a long time in knee and shoulder arthroscopy, with presumed benign effect. A more recent innovation is to place an intra-articular catheter and to send the patient home with a disposable local anesthetic infusion pump. However, there have now been multiple case reports of glenohumeral cartilage damage (chondrolysis) after shoulder intra-articular infusions. [35, 36] More recently, intra-articular infusions have also been associated with chondrolysis of the elbow and knee. [37, 38] Local anesthetics have now been shown to have cartilage toxicity issues in both animal in vivo and human cartilage in vitro studies. [39, 40]
The potential toxicity appears to depend on the concentration of local anesthetic, duration of exposure, and possibly other factors such as pH and the presence of other additives. [41] Home-going intra-articular infusions can no longer be considered a safe practice. The risk of significant cartilage toxicity from single injections of low-dose local anesthetics is thought to be low.
Intra-articular opioids
Peripherally located opioid receptors have been discovered in animals. Animal studies suggest that intra-articular inflammation induces the development of synovial opioid binding sites. In addition, intra-articular opioid administration appears to have an anti-inflammatory effect. Based on these observations, intra-articular opioids are administered in knee and shoulder surgery. [42]
The effect of intra-articular morphine in knee arthroscopy has been examined in multiple studies. A meta-analysis concluded that a mild analgesic effect of intra-articular morphine is observed, but a systemic effect cannot be excluded completely. [43] Whether a dose-response effect is observed and what the optimal dose is are still in question. Morphine doses of 1–5 mg have been used.
Regarding shoulder surgery, in a study of patients undergoing open rotator cuff repairs, patients receiving a combination of 1 mg of morphine with 20 mL of 0.25% bupivacaine had better postoperative pain relief than those patients receiving bupivacaine alone. [44]
Local infiltration analgesia
In 2008, Kerr and Kohan described their technique of systematic infiltration of a mixture of ropivacaine, ketorolac, and epinephrine into the tissues around the surgical field in total knee and hip arthroplasty, and named it "local infiltration analgesia" (LIA). [45] They described low pain scores, low opioid requirements, early immobilization, and earlier hospital discharge. This was a nonrandomized uncontrolled case series. Since that first report, multiple other studies have examined the effectiveness of this technique or variations thereof.
In 2011, Kehlet and Andersen published a review of this topic. [46] They thought that many studies had design problems by not being placebo-controlled or with comparable systemic analgesia provided in the investigated groups. They concluded that little evidence supports the use of the technique in hip replacement, provided multimodal, oral non-opioid analgesia is given. However, they did believe this technique has a place in knee replacement surgery.
It may be that this technique is best used to complement traditional regional anesthetic techniques. For example, in 2012, Mahadevan et al compared femoral and sciatic nerve blocks versus femoral and periarticular infiltration with levobupivacaine for total knee arthroplasty. [47] No significant difference was noted between the groups in pain scores, morphine consumption, or range of motion. Thus, by avoiding sciatic nerve block, more motor function of the leg is preserved in the early postoperative period.
Analgesic Options for Specific Surgeries
For any specific surgery type, several regional anesthetic pain management options may be present. The choices may include the above-mentioned wound infiltration, neuraxial or peripheral nerve block techniques, or a combination of techniques. Analgesic techniques are selected based on the surgical trauma, goals for physical therapy, expected length of patients' hospital stay, and avoidance of adverse effects.
Spine surgery
IT morphine has been used as an adjunct in complex spine surgery such as scoliosis surgery. [48] Iliac crest harvest site infiltration with morphine and local anesthetic is an option.
Shoulder/arm/hand surgery
Shoulder surgery can be performed under interscalene nerve block or a combination of general and interscalene block. Complete pain relief can be achieved (for the duration of the block) unless the incision extends close to the axilla or there are posterior arthroscopy portals out of the block territory.
Interscalene catheters can be placed and infused for prolonged analgesia. Mariano et al compared continuous versus single-injection interscalene blocks. In a randomized, triple-masked, placebo-controlled study, interscalene catheters were placed preoperatively in 30 patients using an ultrasound-guided, in-plane posterior approach. All subjects received an initial bolus of ropivacaine. Postoperatively, the patients were discharged with oral opioid analgesics and a portable infusion device containing either ropivacaine 0.2% or normal saline; the devices were programmed to deliver a perineural infusion over 2 days. Patients who received the ropivacaine infusion experienced greater pain relief, used less oral opioids, suffered fewer sleep disturbances, and rated their satisfaction with analgesia higher. [49]
Other pain management options include subacromial or intra-articular morphine and local anesthetic.
Posimir (bupivacaine) was FDA-approved for administration into the subacromial space under direct arthroscopic visualization to produce postsurgical analgesia following arthroscopic subacromial decompression. The drug contains a sucrose-based biodegradable matrix (sucrose acetate isobutyrate) to form a depot that will release bupivacaine into adjacent tissues over 72 hours. The product label has a boxed warning indicating the potential risk of adverse embolic effects from inadvertent intravascular injection. This product must not be injected intravasculary. [66]
Interscalene, axillary, and infraclavicular catheters can be placed for prolonged pain relief or arm surgery. Besides pain relief, the arm sympathectomy may be of value in certain operations involving vascular repairs.
Hip surgery
IT morphine is very effective for pain control after hip surgery in the first 12–24 hours. [50] Extended-release epidural morphine can provide analgesia for 48 hours. [6]
Epidural local anesthetic and opioid can be infused. The duration of the infusion is limited by perioperative anticoagulation for DVT prophylaxis and by the need to terminate motor nerve block so that physical therapy can be performed.
Lumbar plexus blocks and catheters are used in some institutions to provide postoperative analgesia. Marino et al compared continuous lumbar plexus block with patient-controlled analgesia, continuous femoral block with patient-controlled analgesia, and patient-controlled analgesia alone in 225 patients who underwent unilateral total hip arthroplasty for osteoarthritis. [51] Compared with continuous femoral nerve block and patient-controlled analgesia alone, continuous lumbar plexus block significantly reduced pain scores during physiotherapy on postoperative day 1 and day 2 and was associated with fewer opioid-related adverse effects, greater distances walked, and enhanced patient satisfaction. Additionally, both regional anesthesia techniques provided significantly greater reductions in total hydromorphone consumption and delirium than patient-controlled analgesia alone.
Knee arthroplasty
IT morphine can be used for pain control after knee arthroplasty in the first 12-24 hours. Extended-release epidural morphine can provide analgesia for 48 hours. [7]
As with hip surgery, epidural local anesthetic and opioid can be infused, but the infusion duration is limited by perioperative anticoagulation for DVT prophylaxis. Other issues include potential for sympathectomy and bilateral leg motor weakness, both of which have potential to interfere with the performance of physical therapy.
Femoral nerve blocks and perineural infusions offer very effective analgesia of the anterior knee after knee replacement surgery. Multiple studies have shown the effectiveness of this technique. [52]
With femoral nerve blocks, patients typically have improved range of motion, but quadriceps weakness can increase the risk of falling. Sharma et al determined the complication rate associated with preoperative femoral nerve block for total knee arthroplasty. [53] In 1018 total knee arthroplasties, 709 femoral nerve blocks were used by single-injection technique. Twelve patients treated with femoral nerve block sustained falls, 3 of whom required reoperation. The authors recommended that postoperative protocols be modified for patients who have femoral nerve block, because of decreased quadriceps function in the early postoperative period.
Preliminary reports describe that performing femoral block more distally (in the adductor canal) may have a motor-sparing effect and still provide good analgesia. [54, 55] Because early ambulation and early physical therapy have become an increasing focus after joint replacement surgery, many centers have switched from traditional femoral blocks to using adductor canal blocks for analgesia after knee arthroplasty.
Approximately 80% of patients with femoral nerve blocks have posterior knee pain that is of sciatic origin. There are multiple strategies to deal with this, each with pros and cons, such as (1) sciatic nerve single injection or catheter, (2) surgeon-performed local anesthetic injections, and (3) transcapsular injection.
Sciatic nerve single injection or catheter
A sciatic catheter provides the longest and most effective posterior pain relief. The downsides include an extra catheter and pump for the patient to deal with, potential for motor block and decreased ability to participate in physical therapy, and increased falls risk. In addition, a preoperative block reduces the ability to make an early diagnosis of any surgery-related peroneal nerve injury. Sciatic nerve block does not appear to allow earlier hospital discharge or change any functional outcomes. [56, 57] Sinha recently compared selective tibial nerve block to sciatic nerve block performed at the popliteal fossa. [58] The tibial nerve block group had similar (and excellent) analgesia, but without complete peroneal motor block.
Surgeon-performed local anesthetic injections
Multiple variations in technique are described, including posterior capsular injections, [59] transcruciate injections into the space behind the joint capsule, [60] and intra-articular catheters. These techniques have the advantage of being easy to perform and, in general, have no associated motor block. The duration of analgesia is probably limited to the day of surgery.
Transcapsular injection
A transcapsular injection, which is a modification of the previously mentioned transcruciate injection technique, can also be used. It is performed by the surgeon after preparation of the distal femoral and proximal tibia at the time of either posterior cruciate retaining or substituting total knee replacement.
With the knee flexed to 90°, the landmarks in the area of the intercondylar notch are identified. Flexing the knee and avoidance of any external compression in the area of the popliteal fossa allows the neurovascular structures in the area to fall away from the site of injection. An 18-gauge Tuohy needle is inserted in the anterior-medial corner of the intercondylar notch and carefully directed cephalad in line with the posterior cortex of the distal femur. Insertion of the needle in this position, rather than directly through the substance of the posterior cruciate ligament, increases the distance between the injection site and the popliteal neurovascular structures and reduces the risk of intravascular injection.
A distinctive loss of resistance is typically noted as the needle penetrates the posterior capsule of the knee if the capsule has been undisturbed during the surgery. After the capsule is penetrated with the Tuohy needle, the site is aspirated to verify that the needle is not intravascular and the area injected with 20 mL of 0.25% Marcaine without epinephrine. If any resistance is encountered during the injection, the needle can be advanced slightly, reaspirated, and the injection completed.
This transcapsular injection appears to block the terminal articular fibers of the posterior joint, without any of the typical sensory and motor block seen when the sciatic nerve is anesthetized.
At our institution, we generally do the following:
Use multimodal analgesics, which includes perioperative acetaminophen and ketorolac.
Spinal anesthesia.
Adductor canal block.
Intraoperative transcapsular injections and wound infiltration by the surgeon.
Postoperative parenteral or oral opioids as needed.
On rare occasions, a postoperative sciatic block is performed to deal with significant posterior pain.
Knee arthroscopic procedures
Femoral block can provide excellent analgesia for anterior cruciate ligament repairs with patella tendon grafts. [61] For more prolonged analgesia, femoral nerve catheters can be placed and infused at home via disposable pump. [62] If a quadriceps tendon graft is used, there may be significant posterior pain that is amenable to sciatic nerve block.
For patient pain control in arthroscopy/meniscectomy, intraarticular local anesthetic and morphine are used routinely. Long-acting femoral blocks are avoided so that patient ambulation is not impeded.
Foot
Foot and ankle pain can be controlled with a popliteal fossa block. The saphenous nerve may also need to be blocked if the surgical incision is on the medial aspect of the foot or ankle.
Other Aspects of Pain Management
Peripheral nerve blocks can provide excellent pain relief but have the problem of limited duration. An example of this scenario is a rotator cuff operation performed with a bupivacaine interscalene block. The sudden return of pain 12-18 hours after the bupivacaine interscalene block can be very distressing to the patient and result in the need for large doses of opioids to control the patient's pain. Strategies to manage such a need include the following:
Perioperative oral analgesics
It is a good strategy for the patient to receive a dose of oral analgesic medication before the expected time of nerve-block resolution. The appropriate choice of oral analgesic depends on multiple factors, including type of surgery, subjective pain levels, as well as the presence of any chronic pain comorbidities that may complicate postoperative pain management (i.e., opioid tolerance, hyperalgesic states, central pain syndromes, etc.). As-needed rescue opioids may be necessary for adequate pain control once the nerve block has terminated. Opioid exposure may be minimized by managing patient expectations for both acceptable levels of pain as well as preemptive treatment with non-opioid analgesics (e.g., acetaminophen, non-steroidal anti-inflammatory medications) before regression of regional anesthesia.
Multimodal analgesia
Many centers supplement regional anesthesia techniques with a regimen of oral or IV analgesic medications, with the following goals in mind:
-
Preemptive analgesia – The theory that certain medications may help reduce the up-regulation of nociceptors at peripheral or central locations when pain does occur [63]
-
Improved analgesia during the block – Some techniques reduce pain but do not completely eliminate it; multimodal analgesia helps cover this breakthrough pain and helps reduce opioid requirements
-
Reduced intensity of pain when the block wears off, because the patient already has analgesics in his or her system
Typical regimens include scheduled administration of IV or oral acetaminophen, NSAIDs (IV ketorolac or oral celecoxib ), and neuropathic pain relievers such as gabapentin or pregabalin. A preincisional dose of dexamethasone may also be of benefit. [64]
Perioperative non-steroidal anti-inflammatory drugs (NSAIDs)
As mentioned, NSAIDs can be used as a supplement to opioids. Intravenous ketorolac (Toradol; Roche Laboratories Inc, Nutley, NJ) 15–30 mg IV every 6 hours is a very effective pain reliever of orthopedic pain, and without respiratory depressant effects. As an NSAID, it does have antiplatelet effects and has the potential to increase wound drainage, especially in patients who are receiving postoperative thromboembolic prophylaxis.
Another alternative is the oral cyclooxygenase-2 (COX-2)–inhibitor drug celecoxib (Celebrex; Pfizer Inc, New York, NY). Celecoxib can be administered preoperatively as a 200–400 mg load, then continued with a dose of 200 mg orally once a day. The advantage of this drug is that it does not cause significant platelet dysfunction, so it is less likely to contribute to excessive wound drainage. However, there is controversy regarding the use of celecoxib in patients with known cardiac disease or with risk factors for cardiac disease.
The potential adverse effects associated with the use of NSAIDs include platelet dysfunction, renal dysfunction, and gastric ulceration (especially in patients receiving oral anticoagulants). Of special concern in orthopedic surgery, there is potential for decreased bone growth and healing, which might have an impact on fusion success rates following spinal surgery or bone healing after fracture surgery. [65]
-
Skin infiltration with local anesthetic.
-
Palmar digital nerves.
-
Dorsal digital nerves.