Practice Essentials
Spina bifida is a treatable spinal cord malformation that occurs in varying degrees of severity. Classified as a defect of the neural tube (ie, the embryonic structure that develops into the spinal cord and brain), it was recognized as long as 4000 years ago. The term myelodysplasia has been used as a synonym for spina bifida. (See Pathophysiology and Etiology.)
Neural tube defects have a range of presentations, from stillbirth to incidental radiographic findings of spina bifida occulta. Myelomeningocele, a form of spina bifida, is visible at birth (see the images below). Patients with myelomeningocele present with a spectrum of impairments, but the primary functional deficits are lower limb paralysis and sensory loss, bladder and bowel dysfunction, and cognitive dysfunction. (See Clinical Presentation.) [1]
 The lumbar region of a newborn baby with myelomeningocele. The skin is intact, and the placode-containing remnants of nervous tissue can be observed in the center of the lesion, which is filled with cerebrospinal fluid.
The lumbar region of a newborn baby with myelomeningocele. The skin is intact, and the placode-containing remnants of nervous tissue can be observed in the center of the lesion, which is filled with cerebrospinal fluid.
Blood tests, amniocentesis, or both can be used to screen for neural tube defects. These typically are used in combination with fetal ultrasonography. (See Workup.) Prenatal detection and postatal closure in the first few days of life are clinically associated with lower levels of care and fewer complications in spina bifida. [2]
Treatment advances have allowed an increasing number of patients with neural tube defects to participate and be productive in mainstream society. However, medical, surgical, and rehabilitation issues arise in the patient with myelomeningocele, from birth through adulthood. [3] (See Treatment and Medication.)
The need for a team approach is recognized in contemporary treatment of spina bifida. [4] Bringing together a number of medical and surgical specialists can help to spare parents the strain and exhaustion of coordinating with multiple doctors and can ensure the availability of necessary services. Transitioning from pediatric to adult care has been reported to maintain quality-of-life measures. [5, 6] The physical medicine and rehabilitation specialist assumes a significant role in coordinating the many treatment components that together allow patients to gain maximum function and, particularly, independence. (See Treatment.)
Participation in the care of patients with major, chronic physical disabilities requires commitment, coordination, and access to extensive clinical resources. Improved survival rates in patients with spina bifida can be expected with treatment; quality of life is at least partially dependent on the speed, efficiency, and comprehensiveness of that treatment from birth. (See Prognosis.)
Classification of spina bifida
Spina bifida is a variable defect in which the vertebral arch of the spinal column is either incompletely formed or absent. The term bifida is from the Latin bifidus, or "left in 2 parts." Although the condition has also been referred to as myelodysplasia and myelomeningocele, spina bifida generally has been accepted as the preferred term, specifically by the American Academy of Orthopaedic Surgeons. Rachischisis posterior, the equivalent Greek term, is derived from rachis, meaning spine, and schisis, meaning division (spondyloschisis in Latin).
Spina bifida cystica
Spina bifida cystica can occur anywhere along the spinal axis but most commonly is found in the lumbar region. In this condition, the spine is bifid and a cyst forms. A meningocele, a cystic swelling of the dura and arachnoid, protrudes through the spina bifida defect in the vertebral arch. A person with a meningocele may have no neurologic sequelae.
Spina bifida cystica causes a problem when cord tissue extends into the meningocele, in which case the cyst is called a myelomeningocele. According to Menelaus, the myelomeningocele form of spina bifida cystica is the most significant and common type of spina bifida, accounting for 94% of cases. (Spina bifida occulta is not included in this figure.)
A child born with myelomeningocele requires specialty care and transfer to a center where neonatal surgery and closure can be performed. Surgery involves freeing lateral muscles and skin for coverage and attempting to form a closure of the neural elements with minimal scarring, because the late complication of a tethered cord has frequent and severe consequences.
Another form of spina bifida cystica, the most severe type in fact, is the myelocele, or myeloschisis, variety, in which the open neural plate is covered secondarily by epithelium and the neural plate has spread out onto the surface.
Spina bifida occulta
The term spina bifida does not actually refer to spina bifida occulta, which may exist in a very large number of healthy adults. Some contend that it could be found in up to one third of healthy adults if imaging studies were used to analyze the posterior vertebral arch.
Syringomeningocele
Syringomeningocele is another form of spina bifida. The Greek word syrinx, meaning tube or plate, is combined with meninx (membrane) and kele (tumor). The term thus describes a hollow center, with the spinal fluid connecting with the central canal of the cord enclosed by a membrane with very little cord substance.
Syringomyelocele and syringomyelia
Syringomyelocele is a type of spina bifida in which protrusion of the membranes and spinal cord lead to increased fluid in the central canal, attenuating the cord tissue against a thin-walled sac. Syringomyelia, or hydrosyringomyelia, is the presence of cavities in the spinal cord, which may result from the breakdown of gliomatous new formations.
Signs and symptoms of spina bifida
In general, infants with spina bifida cystica present with the following:
-
Lethargy
-
Poor feeding
-
Irritability
-
Stridor
-
Ocular motor incoordination
-
Development delay
Older children may present with the following:
-
Cognitive or behavioral changes
-
Decreased strength
-
Increased spasticity
-
Changes in bowel or bladder function
-
Lower cranial nerve dysfunction
-
Back pain
-
Worsening spinal or lower extremity orthopedic deformities
For the sake of general functional prognosis and anticipation of specific musculoskeletal complications, myelomeningocele patients frequently are classified as belonging to one of the following groups, based on the neurosegmental level of the lesion:
-
Thoracic - In the thoracic group, innervation of the upper limb and neck musculature and variable function of trunk musculature are present, with no volitional lower limb movements; patients with thoracic malformations tend to have more involvement of the central nervous system (CNS) and associated cognitive deficits
-
High lumbar - In the high-lumbar group, variable hip flexor and hip adductor strength is characteristic; absence of hip extension, hip abduction, and all knee and ankle movements is noted
-
Low lumbar - In the low-lumbar group, hip flexor, adductor, medial hamstring, and quadriceps strength is present; the strength of the lateral hamstrings, hip abductors, and ankle dorsiflexors is variable; the strength of the ankle plantar flexors is absent
-
Sacral - In the sacral-level group, strength of all hip and knee groups is present; ankle plantar flexor strength is variable
Workup in spina bifida
Lab studies
Laboratory screening tests for neural tube defects can be performed through blood tests, amniocentesis, or both.
The fetal presence of an open neural tube defect is marked by an elevated alpha-fetoprotein (AFP) level in the amniotic fluid. Peak concentrations of AFP in the 13th to 15th weeks of pregnancy permit diagnosis, and ultrasonographic confirmation with amniocentesis generally is possible at 15-18 weeks. Encephaloceles or skin-covered myeloceles are unlikely to be detected by AFP measurement.
Perform urinalysis, urine culture, and a serum urea nitrogen creatinine test at birth to evaluate renal function in neonates with spina bifida. Recommend regular bacterial urinary cultures for children who have vesicoureteral reflux or signs and symptoms of urinary tract infection.
Psychometric assessment
Psychometric assessments of intelligence and cognitive function are indicated for patients with hydrocephalus and for those who display deficits in speech and language functions and/or cognitive or academic skills.
Imaging studies
These include the following:
-
Fetal ultrasonography - Some centers use fetal ultrasonography as the primary screening tool for neural tube defects, usually at approximately 18 weeks’ gestational age
-
Computed tomography (CT) scanning - A CT scan of the head is appropriate to evaluate for possible recurrent hydrocephalus or a change in the size or function of the ventricles, which may be affected even with normal pressure hydrocephalus
-
Magnetic resonance imaging (MRI) - Magnetic resonance imaging (MRI) of the spine and brain is helpful in neurologic assessment and provides a baseline for comparison in future investigations, especially in the context of progressive neurologic deterioration
-
Radiography - Radiographs of the vertebrae provide information for early evaluation when an infant is born with myelomeningocele; after delivery, the criterion standard for determining the level of the lesion is a plain film radiograph
Management of spina bifida
In the United States, antibiotics, sac closure, and ventriculoperitoneal shunt placement are the standard of care for spina bifida and are implemented in the perinatal period in 93-95% of patients. Supportive care alone may be recommended in cases associated with an irreparable sac, active gross CNS infection or bleeding, and/or other gross congenital organ anomalies causing life-threatening problems.
In addition to physical therapy, rehabilitation for spina bifida includes occupational and recreational therapy; speech therapy may be indicated for patients with speech and/or swallowing difficulties. [7, 8, 9, 10]
Physical therapy programs are designed to parallel the normal achievement of gross motor milestones. Occupational therapy should be initiated early to compensate for motor skill deficits and should progress along the normal developmental sequence. Recreational therapy is helpful for promoting independence by enhancing play and recreational opportunities.
Pathophysiology
Neural tube defects are the result of a teratogenic process that causes failed closure and abnormal differentiation of the embryonic neural tube. Neural tube defects occur between the 17th and 30th day of gestation, at a time when the mother may not be aware that she is pregnant and the fetus is estimated to be about the size of a grain of rice.
The most common neural tube defects are anencephaly and myelomeningocele. Anencephaly results from failed closure of the rostral end of the neural tube, resulting in incomplete formation of the brain and skull.
Myelomeningocele
Spina bifida cystica causes a problem when the meningeal cyst (meningocele) includes cord tissue extending into the cyst (in which case, it is a myelomeningocele). The condition is also of particular concern when the neural tube is completely open and the ependymal layer is exposed as a myelocele (or myeloschisis). A meningocele alone may cause no neurologic problems if the cord is confined to the vertebral canal.
Myelomeningocele results from failed closure of the caudal end of the neural tube, resulting in an open lesion or sac that contains dysplastic spinal cord, nerve roots, meninges, vertebral bodies, and skin (see the image below). The anatomic level of the myelomeningocele sac roughly correlates with the patient's neurologic, motor, and sensory deficits. [11]
Myelomeningocele is associated with abnormal development of the cranial neural tube, which results in several characteristic CNS anomalies. The Chiari type II malformation is characterized by cerebellar hypoplasia and varying degrees of caudal displacement of the lower brainstem into the upper cervical canal through the foramen magnum. This deformity impedes the flow and absorption of cerebrospinal fluid (CSF) and causes hydrocephalus, which occurs in more than 90% of infants with myelomeningocele. (See the image below.)
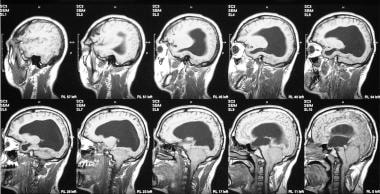 Coronal, T1-weighted magnetic resonance imaging (MRI) scans of the brain show a Chiari II malformation. Note the stretching of the brainstem, aqueduct, and fourth ventricle.
Coronal, T1-weighted magnetic resonance imaging (MRI) scans of the brain show a Chiari II malformation. Note the stretching of the brainstem, aqueduct, and fourth ventricle.
Cerebral cortex dysplasia, including heterotopias, polymicrogyria, abnormal lamination, fused thalami, and corpus callosum abnormalities, also occurs frequently. In addition, mesodermal structures surrounding the neural tube, such as the vertebra and ribs, may be malformed.
Unprotected neural elements are at severe risk during delivery. The sequelae of the neural tube defect follow directly from this lack of protection, occurring mechanically or resulting from desiccation, scarring with closure, and/or a lack of vascular support or from other insults to the delicate neural elements.
The neurologic damage generally results in a neurogenic bowel and bladder, which leads to incontinence. With a lack of neural input, a contracted bladder causes hydronephrosis, along with infections and renal failure, which may be the prime determinant of longevity in patients with spina bifida.
As a pattern, neurologic innervation is not symmetrical between lower-limb flexors and extensors; the corresponding levels are lower (caudal) for the extensors than for the flexors. Generally, muscular imbalance is present in patients with myelomeningocele, which results in joint contractures and developmental problems, such as hip dislocation and spinal deformities.
Normal intelligence can be expected with aggressive shunting for hydrocephalus, although seizure activity secondary to the neural tube defect may be noted. In addition, subtle defects in coordination may be associated with the cerebellar deficiency from the Arnold-Chiari malformation, which is a malformation of the cerebellum, with elongation of the cerebellar tonsils and with the cerebellum drawn into the fourth ventricle. The condition also is characterized by smallness of the medulla and pons and by internal hydrocephalus. In fact, all patients with spina bifida cystica (failure to close caudally) have some form of Arnold-Chiari malformation (failure to close cranially).
Myelomeningocele often occurs along with multiple system congenital anomalies. Commonly associated anomalies are facial clefts, heart malformations, and genitourinary tract anomalies. Urinary tract anomalies, such as solitary kidney or malformed ureters, may contribute to increased morbidity in the presence of neurogenic bladder dysfunction.
A study by Flores et al indicated that in children with myelomeningocele, greater movement quality and trunk control predict functional ambulation in the patient, with more optimal spatiotemporal gait parameters. The investigators found good correlation between the Pediatric Neuromuscular Recovery Scale (Peds NRS) summary score and the modified Hoffer Functional Ambulation Scale score. They also determined that sit-to-stand and three standing/walking items were strongly associated with cadence and with swing and stance time. In addition, two Peds NRS standing items and the modified Hoffer scale score correlated well with velocity. [12]
Embryology
During prenatal development, neuroectoderm thickens into the neural plate, which then folds into a neural groove by the time somites appear. The groove deepens to become the neural tube, and dorsal fusion begins centrally, extending cephalad and caudally, with the cephalad pole fusing at the 25th day. The ventricle becomes permeable at the 6th to 8th week of gestation but this apparently does not proceed normally in patients with myelomeningocele.
Some studies suggest that an increased amount of neural crest material in the defect prevents neural tube closure. Another hypothesis is that an already closed tube ruptures; increased permeability of the rhombic groove leads to greater CSF secretion and increased luminal pressure, with the tube then expanding and essentially splitting the neural element at its weakest areas (ie, the cephalic and caudal ends).
Research by McLone and Knepper supports the latter hypothesis and details the implications of this defect on the entire CNS. [13]
Obesity
Obesity is prevalent in children with myelomeningocele, especially those with high-lumbar and thoracic-level lesions, because of reduced capacity for caloric expenditure. The decreased muscle mass of the lower body musculature results in a lower basal metabolic rate. In addition, activity levels generally are lower than in unaffected children as a direct result of lesion-related mobility deficits and as an indirect result of decreased opportunities for disabled children to participate in physical play.
A report by Polfuss et al attributed obesity in patients with spina bifida to multiple factors, including individual ones (ie, body composition and measurement issues, energy needs, eating patterns, physical activity, sedentary activity), parenting/family, peers, community factors (ie, culture, built environment, and factors related to healthcare, healthcare providers, and school), and societal factors (ie, policy issues). [14]
Obesity can exert negative impact on self-image and further perpetuate a cycle of inactivity and overeating. Excessive weight impedes maximal independence and ambulation.
Bone involvement
Bone mineral density is decreased in patients with myelomeningocele. [15] Markers of bone reabsorption have been found more frequently in limited ambulators and nonambulators than in children who ambulate regularly.
Children with myelomeningocele are at higher risk of lower extremity fractures. Reduced muscle activity in the paralyzed limb and decreased weight-bearing forces result in decreased bone mass. In addition, many fractures occur after orthopedic interventions, especially after procedures associated with cast immobilization. Fractures in myelomeningocele tend to heal quickly, and excessive callus formation often is seen.
Urinary tract dysfunction
The main determinant of upper urinary tract deterioration is the intravesical pressure in storage and voiding situations. A high incidence of vesicoureteral reflux and ureteral dilation has been found in patients with myelomeningocele whose leak-point pressures are greater than 40 cm water.
High pressures may result from increased outlet resistance or decreased bladder wall compliance. Increased outlet resistance may be caused by sphincter dyssynergia or fibrosis of a denervated sphincter. Decreased bladder wall compliance is associated with areflexia of the detrusor. Any of these urologic dysfunctions can occur in myelomeningocele, but manifestations may vary over time because of the changing neurologic status in some of these patients.
Abnormalities in sexual development and function
Females with myelomeningocele go through puberty 1-2 years earlier than their unaffected peers. Sexual precocity is associated with hydrocephalus and obesity. Abnormal genital sensation is typical, but some female patients with myelomeningocele are able to achieve orgasm. Fertility is not affected in females with myelomeningocele; however, pregnancy carries increased risk of urinary tract infection, back pain, and perineal prolapse postpartum.
Young men with myelomeningocele have abnormal genital sensation, decreased ability to achieve and sustain erections, and decreased fertility. However, the potential for ejaculation and reproduction must be assessed for each individual patient. Implantable penile prosthetic devices, vacuum tumescence devices, and electrical stimulation have been used for some patients unable to achieve erections.
Latex sensitization
Latex sensitization is more common in patients with myelomeningocele, likely due to a genetic predisposition and a higher degree of exposure. The number of surgical interventions (particularly orthopedic and urologic procedures), the presence of a ventriculoperitoneal shunt, and total serum immunoglobulin E (IgE) levels have been associated with latex allergy in children with myelomeningocele. Establishment of a latex-free environment for surgery, however, has resulted in a decrease in sensitization of these patients to latex.
Etiology
The etiology in most cases of myelomeningocele is multifactorial, involving genetic, racial, and environmental factors, in which nutrition, particularly folic acid intake, is key. Cytoplasmic factors, polygenic inheritance, chromosomal aberrations, and environmental influences (eg, teratogens) have all been considered as possible causes. A small number of cases are linked to specific etiologic factors.
Most infants born with myelomeningocele are born to mothers with no previously affected children. However, other offspring in a family with 1 affected child are at greater risk for neural tube defect than are children without affected siblings. The risk is 1 in 20-30 for subsequent pregnancies, and if 2 children are affected, the risk becomes 1 in 2. An increase in the risk of myelomeningocele has also been reported for second- and third-degree relatives of affected individuals.
Up to 10% of fetuses with a neural tube defect detected in early gestation have an associated chromosome abnormality. Associated chromosome abnormalities include trisomies 13 and 18, triploidy, and single-gene mutations.
In women with pregestational diabetes, the risk of having a child with a CNS malformation, including myelomeningocele, is 2-10 fold higher than the risk in the general population. The mechanism underlying this teratogenic effect is not well defined but is related to the degree of maternal metabolic control. The risk in women who develop gestational diabetes is lower than the risk in women with pregestational diabetes, but it might not be as low as in the general population.
Other risk factors for myelomeningocele include maternal obesity, hyperthermia (as a result of maternal fever or febrile illness or the use of saunas, hot tubs, or tanning beds), and maternal diarrhea. Identified risk factors also include intrauterine exposure to antiepileptic drugs, particularly valproate and carbamazepine, and to drugs used to induce ovulation. [16, 17, 18]
The risk of having a child with myelomeningocele has also possibly been associated with maternal exposures to fumonisins, electromagnetic fields, hazardous waste sites, disinfection by-products found in drinking water, and pesticides.
Folic acid deficiency
Research in the 1980s showed correction of folic acid deficiency as an effective means of primary and recurrent prevention. [19] At least half of cases of neural tube defects are related to a nutritional deficiency of folic acid or increased requirement and, thus, are potentially preventable. (An elevated risk of neural tube defects has also been linked to higher levels of folate receptor autoimmunity, in a dose-response manner. [20] )
In September 1992, the US Public Health Service (USPHS) recommended intake of folic acid at a dosage of 0.4 mg (400 mcg) per day for all women anticipating pregnancy. (Currently, the US Centers for Disease Control and Prevention [CDC] also recommends 400 mcg/day, while the US Preventive Services Task Force recommends 400-800 mcg/day.) In January 1998, the mandatory fortification of enriched cereal grain products with folic acid went into effect in the United States; this measure that was expected to increase the daily intake of folic acid in women of reproductive age by approximately 100 mcg/day.
According to the CDC, the prevalence of spina bifida from October 1995 to December 1996 (before mandatory fortification) was 2.62 per 10,000 live births, while the prevalence from October 1998 to December 1999 was 2.02 per 10,000 live births, a 22.9% reduction. Later declines were smaller, however, with the prevalence of spina bifida falling just 6.9% between the surveillance periods 1999-2000 and 2003-2005; for reasons that remain unclear, this included a significant decrease in prevalence within the black population but not within the white and Hispanic populations. [19, 21]
Epidemiology
Occurrence in the United States
The incidence of spina bifida has been estimated at 1-2 cases per 1000 population, with certain populations having a significantly greater incidence based on genetic predilection. Folate fortification of enriched grain products has been mandatory in the United States since 1998; research indicates that folate can reduce the incidence of neural tube defects by about 70% and can also decrease the severity of these defects when they occur. [18, 22, 23, 24]
Neural tube defects are the second most common type of birth defect after congenital heart defects, and myelomeningocele is the most common form of neural tube defect. In the United States, approximately 1500 infants are born with myelomeningocele each year.
Birth incidence of the disease was reported to be 4.4-4.6 cases per 10,000 live births from 1983-1990. Rates varied by region, with the incidence being higher on the East Coast than on the West Coast and with the highest rates occurring in Appalachia. The rate of myelomeningocele and other neural tube defects has declined since the late 20th century. This is attributed to the widespread availability of prenatal diagnostic services and to improved nutrition among pregnant women.
International occurrence
The average worldwide incidence of spina bifida is 1 case per 1000 births, but marked geographic variations occur. Neural tube defects occur at frequencies (per 10,000 births) ranging from 0.9 in Canada and 0.7 in central France to 7.7 in the United Arab Emirates and 11.7 in South America.
The highest rates of spina bifida are found in parts of the British Isles, mainly Ireland and Wales, where 3-4 cases of myelomeningocele per 1000 population have been reported, along with more than 6 cases of anencephaly (both live births and stillbirths) per 1000 population. The reported overall incidence of myelomeningocele in the British Isles is 2-3.5 cases per 1000 births.
In France, Norway, Hungary, Czechoslovakia, Yugoslavia, and Japan, a low prevalence is reported, being just 0.1-0.6 cases per 1000 live births.
A study by Blencowe et al estimated that in 2015, there were 260,100 birth outcomes worldwide impacted by neural tube defects, with about half ending in elective pregnancy termination (owing to the presence of fetal anomalies) or in stillbirth. [25]
Low socioeconomic status is associated with higher risk of neural tube defects in many populations. Since approximately 1940, epidemics of myelomeningocele have occurred in Boston, Mass; Rochester, NY; Dublin, Ireland; The People's Republic of China; and Jamaica. [26]
Race-related demographics
According to the CDC, the prevalence of spina bifida in the United States is higher in the white and Hispanic populations (2 and 1.96, respectively, per 10,000 live births) than in the black population (1.74 per 10,000 live births). [27, 28, 29, 21]
Sex-related demographics
Data from state and national surveillance systems from 1983-1990 found the birth prevalence rate of myelomeningocele to be slightly higher in females than in males (1.2:1). A higher proportion of females than males exhibit thoracic-level malformations.
Prognosis
Studies of children with prenatally diagnosed myelomeningocele suggest that less severe ventriculomegaly and a lower anatomic level of lesion on prenatal ultrasonograms predict better developmental outcomes in childhood. Aggressive treatment with closure in the neonatal period leads to survival in most cases of spina bifida.
Cognitive function
As a group, patients with myelomeningocele have intelligence scores below the population average but within the normal range. Cognitive dysfunction is most strongly correlated with the presence of hydrocephalus, along with hydrocephalus-related illness parameters (ie, the necessity of shunting, number of shunt revisions, shunt infections, and additional structural abnormalities of the CNS). [30]
Aggressive shunting of hydrocephalus can permit the retention of near-normal intelligence in the majority of patients. Children who do not require shunt revisions are more likely to be employed, live independently, and drive as adults. [31]
Cognitive function has also been related to the level of the lesion. Upper-level lesions have been associated with a higher frequency of mental retardation and lower scores on measures of intelligence, academic skills, and adaptive behavior.
Children with myelomeningocele tend to demonstrate generalized deficits in visual memory and auditory/verbal memory. Verbal subtest scores usually exceed performance subtest scores, with visual-spatial organizational deficits that may be explained in part by upper limb discoordination and/or memory deficits.
The term "cocktail personality" has been applied to a subgroup of patients with hydrocephalus who appear to have advanced expressive language skills. The speech of these individuals typically is verbose, but it tends to lack content and contains jargon and many clichés. This pattern often is associated with poor comprehension skills and reflects significant cognitive impairments and functional deficits.
Approximately 75% of children with myelomeningocele have an IQ higher than 80. Among those whose intelligence is normal, 60% are learning disabled, with the most common feature being a nonverbal learning disability. Particular deficits are seen in mathematics, sequencing, visual perceptual skills, and problem solving. Prevalence of attention problems has been estimated to be 30-40%.
Ambulation
The ability to ambulate depends on, and directly correlates with, the functional sensorimotor level. The patient’s motor level is difficult to assess in the neonate, but the sensory level in infancy is easier to evaluate. Children with sensory levels below L3 are more likely to ambulate as adults and are less likely to have pressure sores or need daily care. [31, 32, 33, 34]
Studies have shown that approximately 50-60% of young adult patients ambulate household or community distances, with about 20% of these patients using some orthotic or assistive device. The other 50% of patients use wheelchairs as their primary form of mobility. Approximately 20% of these individuals ambulate with orthotics and assistive devices as a form of therapeutic exercise. [35]
Several studies have shown that ambulation in patients with myelomeningocele is related to the strength of certain key muscles, including the iliopsoas, gluteus medius, hamstrings, and/or quadriceps. Specifically, a motor neurologic level of L5 or quadriceps strength graded as good (4 out of 5) in the first 3 years of life is predictive of a good prognosis for community ambulation. Gluteus medius strength was the best predictor of a need for gait aids and orthoses. In a 25-year follow-up study of young adults with myelomeningocele, no patient with a lesion at L3 or above ambulated a majority of the time. [36]
Maximal ability to ambulate usually is achieved by the time the child reaches age 8-9 years. Studies have shown that a majority of preadolescent patients, even those with higher-level lesions, are community ambulators when they receive aggressive multidisciplinary interventions. After adolescence, however, community ambulation decreases to approximately 50%.
The ability to ambulate tends to decline in the second decade of life because of increased body dimensions and higher energy requirements. Lower-extremity muscle deterioration also may play a role. Functional decline with aging in patients with myelomeningocele also can be exacerbated by obesity, decubitus ulcers, and psychological issues.
For example, a retrospective study by Dicianno et al found that depressive symptoms in adult patients with spina bifida were significantly associated with lower mobility scores on the Craig Handicap Assessment and Reporting Technique-Short Form (CHART-SF). The study, of 190 adults with spina bifida, also suggested that depressive symptomatology was common in this cohort, determining that 49 of the patients (25.8%) had Beck Depression Inventory-II (BDI-II) scores of over 14 and that 69 patients (36.3%) were taking antidepressants for the treatment of depressive symptoms. [37]
Activities of daily living
Except for sphincter control, independence in activities of daily living (ADL) is likely for children born with myelomeningocele without hydrocephalus. Similarly, for children born with myelomeningocele and hydrocephalus, those with a level of lesion of L4/5 (quadriceps grade of good) or below are likely to be independent for almost all ADL except sphincter control. Those with higher-level lesions are at significant risk for dependence in ADL.
Continence
The data on continence from the literature is variable, which in part reflects inconsistencies in the definition of social continence. Studies report 40-85% achievement of bladder continence and 50-85% achievement of bowel continence. Approximately 25% of patients are continent of both bowel and bladder. The likelihood of social continence improves when training is instituted before age 7 years. The psychosocial consequence of bowel and bladder incontinence can have a dramatic impact on children with myelomeningocele, especially in adolescence.
Employment, independence, and quality of life
Studies of adults with myelomeningocele have shown that about 20-30% secure gainful employment. In one study, employment status was related to lesion level and motor independence. However, motor independence was not found to be related to self-reported quality of life or range of life experiences. [38]
Several studies have shown a greater number of shunt revisions to be associated with reduced independence and achievement in adulthood. [39] This suggests that close medical management in order to minimize episodes of increased intracranial pressure may improve adult employment and quality of life.
Perceived family environment may explain different levels of participation of patients with myelomeningocele in employment, community mobility, and social activity as an adult, even beyond what can be explained by lesion level and intelligence. A positive correlation exists between perceived family encouragement of independence and outcomes in young adults with myelomeningocele.
A study by Davis et al indicated that in adults with spina bifida, those with a higher level of education and no stool incontinence are less likely to experience permanent disability. [40]
Complications
Neurologic complications
Neurologic complications in patients with myelomeningocele are related to a variety of CNS and spinal cord pathologies. Approximately 25-35% or more of children with myelomeningocele are born with hydrocephalus, and an additional 60-70% of patients with myelomeningocele develop hydrocephalus after closure of the myelomeningocele lesion. Hydrocephalus can cause expansion of the ventricles and loss of cerebral cortex and is associated with an increased risk of cognitive impairment.
Seizures occur in 10-30% of affected children and adolescents. These can be related to brain malformation, or they may be a sign of shunt malfunction or infection.
The Chiari type II malformation is present anatomically in almost all patients with myelomeningocele and can result in hindbrain and/or upper cervical spinal cord dysfunction. Clinical manifestations of the Chiari II malformation are more common during infancy and, overall, are seen in 20-30% of affected children. However, symptoms can develop at any age and can manifest acutely or chronically.
Urologic complications
Myelomeningocele is the most common cause of neurogenic bladder dysfunction in children. The nature of the urinary tract dysfunction in myelomeningocele depends on the level and extent of the spinal cord lesion.
Disruption of the neural axis between the pons and the sacral spinal cord by the myelomeningocele may cause uninhibited detrusor contractions or dyssynergia, a lack of coordination of the external bladder sphincter that causes involuntary sphincter activity during detrusor contraction. Myelomeningocele in the sacral area can produce a lower motor neuron lesion, resulting in detrusor areflexia.
These abnormalities may occur singly or in combination and typically result in incontinence and impaired bladder emptying that can lead to vesicoureteral reflux and high voiding pressures. [41] If untreated, such dysfunction can lead to potentially more serious complications, including frequent infections, upper urinary tract deterioration, and, ultimately, renal failure.
Skin breakdown
Skin breakdown occurs in 85-95% of children with myelomeningocele before young adulthood, and recurrent decubitus ulcers can lead to prolonged morbidity and functional disability. Healing can occur if the precipitating mechanical factors are eliminated. Plastic surgical correction may be necessary in severe cases and may involve orthopedic correction of underlying postural abnormalities.
The sites and causes of skin breakdown vary by age and lesion level. Skin breakdown on the lower limb occurs in 30-50% of cases in all lesion-level groups.
The most common areas of breakdown in the thoracic-level group are the perineum and above the apex of the kyphotic curve. Overall, tissue ischemia from pressure necrosis is the most common etiology.
Older children may have higher risk of skin breakdown, because of increased pressure of a larger body habitus, asymmetrical weight-bearing from acquired musculoskeletal deformities, and lower limb vascular insufficiency or venous stasis.
Frequent causes of skin breakdown that are more prevalent in younger children include casts or orthotic devices, skin maceration from urine and stool soiling, friction, shear, and burns.
Ulcers from bracing are prominent in the lower extremities, in the pelvis, and, particularly, over the bony prominences as a result of sitting. Carefully inspecting the skin on a routine basis is important because the area may be subjected to pressure for a couple of hours. The skin subsequently may be reddened, and although the patient may have no pain, the skin can develop significant full-thickness problems after only a brief period of neglect.
Mortality
In general, survival and degree of neurologic impairment depend on the level of the spinal segment involved, the severity of the lesion, and the extent of associated abnormalities. [42]
The mortality rate for infants with myelomeningocele is increased over the general population risk in the first year of the life. Mortality rates reported for untreated infants range from 90-100%, based on several studies dating from the turn of the century through recent years. Most untreated infants die within the first year of life. Death in the first 2 years of life for those untreated usually results from hydrocephalus or intracranial infection. An infant aged 2 months with untreated myelomeningocele has only a 28% likelihood of living 7 years. [43]
Survival rates for infants born with myelomeningocele have improved dramatically with the introduction of antibiotics and developments in the neurosurgical treatment of hydrocephalus. Early death in treated and untreated patients is associated with advanced hydrocephalus and multiple system congenital anomalies.
Renal compromise occurs because of problems related to neurogenic bladder. Despite advances in the management of neurogenic bladder, renal failure is still the leading cause of death in patients with myelomeningocele after the first year of life.
Longevity may depend on the careful use of clean intermittent catheterization and compliance with a bowel and bladder regimen. Long-term survival into adulthood and advanced age is now common with aggressive treatment and an interdisciplinary clinical approach. With proper urologic management, more than 95% of children with myelomeningocele continue to have normal renal function. In addition, bladder augmentation has been reported to have a positive impact on urologic infections and mortality in spina bifida. [44]
Patient Education
Institute measures to avoid development of soft tissue contractures in the neonatal period. Physical and/or occupational therapists provide caregivers with instruction in handling and positioning techniques. In the first several years of life, recommend incorporation of stretching and strengthening exercises into a home program performed by the caregivers and later into play and physical education activities at school.
Instruct preschool and school-aged children with myelomeningocele in the use of adaptive equipment and alternative methods for self-care and performance of ADL. To become independent by school age, young children with myelomeningocele need to become active participants in skin care, bowel and bladder management, and donning and doffing of orthotics, in addition to traditional ADL tasks such as feeding and dressing.
Acquisition of ADL skills often is influenced by attitudes and expectations, so the multidisciplinary team members need to emphasize carryover of ADL skills in the home and school environments by providing anticipatory guidance to parents and caregivers.
Strategies for prevention of skin breakdown first are directed at parents and caregivers, but children with myelomeningocele should be encouraged from an early age to take responsibility for their own skin care. Parents must first be made aware of the areas of abnormal sensation. Necessary precautions include daily skin inspections, pressure relief, avoidance of exposure to extreme temperatures and harmful surfaces, and frequent monitoring of shoes and orthotics.
Self-catheterization techniques should be introduced during the later preschool years to promote normal progress toward independence. Mastery of self-catheterization in patients with myelomeningocele usually is achieved by age 6-8 years, depending on the severity of cognitive and motor involvement.
A functional environment should be created for the patient at home and school to facilitate efficient independent functioning.
A study by Vaccha and Adams indicated that family environment can influence language skills in children with myelomeningocele. [45] The investigators studied 75 children with myelomeningocele, aged 7-16 years, along with 35 age-matched controls, and found a positive association between language performance in children with myelomeningocele and a focus on intellectually and culturally enhancing activities by their families.
Sex education
Sex education and counseling should begin early to help adolescents with myelomeningocele make a positive adjustment to adolescence and to help them avoid misinformation. Sex education, including accurate information about safe sex, should be included in the routine health-care maintenance of the older child and adolescent with myelomeningocele.
Studies of young people with myelomeningocele have shown that, although many are involved in intimate relationships, most had inadequate knowledge about sexuality and reproductive health issues related to their condition. A report indicated that young people with spina bifida face difficulties in obtaining answers to questions concerning romantic relationships, fertility, and sexuality and encouraged medical providers to educate these patients with regard to sexual health. [46, 47]
For patient education information, see the Brain and Nervous System Center, as well as Spina Bifida and Bladder Control Problems.
-
The lumbar region of a newborn baby with myelomeningocele. The skin is intact, and the placode-containing remnants of nervous tissue can be observed in the center of the lesion, which is filled with cerebrospinal fluid.
-
Myelomeningocele in a newborn.
-
Coronal, T1-weighted magnetic resonance imaging (MRI) scans of the brain show a Chiari II malformation. Note the stretching of the brainstem, aqueduct, and fourth ventricle.
-
Neonate with a lumbar myelomeningocele with an L5 neurologic level. Note the diaphanous sac filled with cerebrospinal fluid and containing fragile vessels in its membrane. Also, note the neural placode plastered to the dorsal surface of the sac. This patient underwent closure of his back and an untethering of his neural placode. The neural placode was circumnavigated and placed in the neural canal. A dural sleeve was fashioned in a way that reconstructed neural tube geometry.
-
Sagittal, T1-weighted magnetic resonance imaging (MRI) scan of a child after closure of his myelomeningocele. Child is aged 7 years. Note the spinal cord ends in the sacral region far below the normal level of T12-L1. It is tethered at the point at which the neural placode was attached to the skin defect during gestation. The MRI scan showed dorsal tethering, and the child complained of back pain and had a new foot deformity on examination. By definition, all children with a myelomeningocele have a tethered cord on MRI, but only about 20% of children require an operation to untether the spinal cord during their first decade of life, during their rapid growth spurts. Thus, the MRI scan must be placed in context of a history and examination consistent with mechanical tethering and a resultant neurologic deterioration.
-
Axial, T1-weighted MRI scan of a 15-year-old girl who was born with thoracic myelomeningocele, hydrocephalus, and Arnold-Chiari II syndrome. She was treated with a ventriculoperitoneal shunt. The ventricular system has a characteristic shape, with small frontal and large occipital horns, which are typical in patients with spina bifida. The shunt tube is shown in the right parietal region.
Tables
What would you like to print?
- Overview
- Presentation
- DDx
- Workup
- Treatment
- Approach Considerations
- Bladder Management
- Bowel Management
- Bracing and Orthotics
- Physical Therapy
- Occupational Therapy
- Recreational Therapy
- Myelomeningocele Closure
- Shunting for Hydrocephalus and Syringomyelia
- Chiari Malformation Repair
- Orthopedic Procedures
- Consultations
- Long-Term Monitoring
- Prevention
- Show All
- Medication
- Media Gallery
- References








