Practice Essentials
The cervical spine is the third most common site of rheumatoid arthritis (RA), after the metatarsophalangeal joints and the metacarpophalangeal joints. Rheumatoid spondylitis primarily affects the cervical spine; involvement of the thoracic or lumbar spine is rare. (In contrast, ankylosing spondylitis primarily involves the sacroiliac joints and lumbosacral spine. [1] ) The anatomic abnormalities occur as a consequence of the destruction of synovial joints, ligaments, and bone.
Rheumatoid abnormalities of the cervical spine generally can be grouped into the following 3 categories, which may be seen in isolation or in combination:
-
Atlantoaxial instability (AAI)
-
Superior migration of the odontoid (SMO)
-
Subaxial subluxation
AAI, or atlantoaxial subluxation (AAS), is the most common abnormality (see the image below). AAS can be a fixed deformity or can be partially or fully reducible.
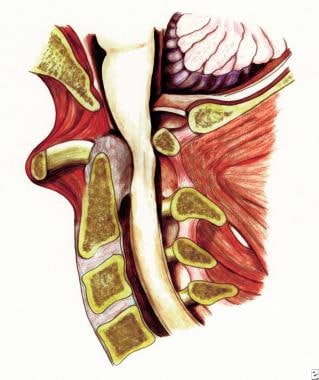 Rheumatoid spondylitis. Depiction of anterior subluxation of C1 on C2, retrodental pannus, and osseous erosions; the spinal cord is compressed between the pannus anteriorly and the posterior arch of the atlas.
Rheumatoid spondylitis. Depiction of anterior subluxation of C1 on C2, retrodental pannus, and osseous erosions; the spinal cord is compressed between the pannus anteriorly and the posterior arch of the atlas.
Superior migration of the odontoid (SMO), the second most common abnormality, has alternately been referred to as cranial settling, pseudobasilar invagination, or vertical/upward translocation of the odontoid. [2] (See the following images.)
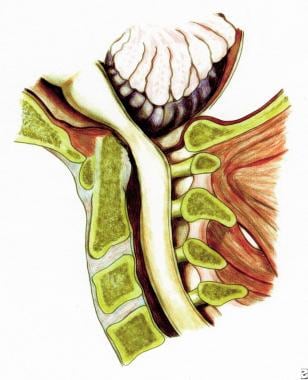 Rheumatoid spondylitis. Depiction of superior migration of the odontoid into the foramen magnum with compression of the spinal cord.
Rheumatoid spondylitis. Depiction of superior migration of the odontoid into the foramen magnum with compression of the spinal cord.
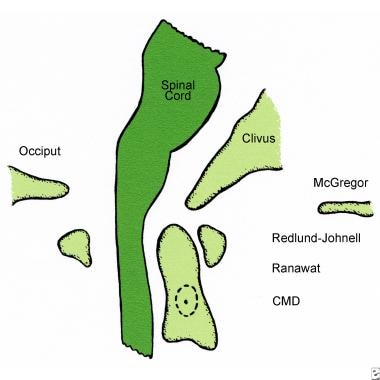 Rheumatoid spondylitis. Pertinent measurements of superior migration of the odontoid; cranial migration distance (CMD).
Rheumatoid spondylitis. Pertinent measurements of superior migration of the odontoid; cranial migration distance (CMD).
Subaxial subluxation, the least common deformity, may be seen at multiple levels. It produces a stepladder deformity.
Surgical management of cervical spine RA is indicated when it results in symptoms from biomechanical instability or a neurologic deficit. The surgical approach varies with the tyoe of deformity. [3]
See Rheumatoid Arthritis and Ankylosing Spondylitis and Undifferentiated Spondyloarthropathy for more information on these topics.
See Rheumatoid Arthritis: In and Out of the Joint, a Critical Images slideshow, to help identify the distinguishing features of RA as well as the signs of extra-articular manifestations of this disfiguring disease.
For patient education information, see Rheumatoid Arthritis and Rheumatoid Arthritis Medications.
Pathophysiology
Although the pathogenesis of rheumatoid arthritis remains incompletely understood, current theories suggest that the synovial cells of these patients chronically express an antigen that triggers the production of rheumatoid factor (RF), an immunoglobulin molecule directed against other autologous immunoglobulins. An inflammatory response is initiated, involving immune complex formation, activation of the complement cascade, and infiltration of polymorphonuclear leukocytes.
The proliferating fibroblasts and inflammatory cells produce granulation tissue, known as rheumatoid pannus, within the synovium. The pannus produces proteolytic enzymes capable of destroying adjacent cartilage, ligaments, tendons, and bone. The destructive synovitis results in ligamentous laxity and bony erosion with resultant cervical instability and subluxation. [4, 5, 6]
Atlantoaxial subluxation results from erosive synovitis in the atlantoaxial, atlanto-odontoid, and atlanto-occipital joints and the bursa between the odontoid and the transverse ligament (see the image below). Damage to the transverse ligament alone leads to approximately 3-4 mm of subluxation. [7]
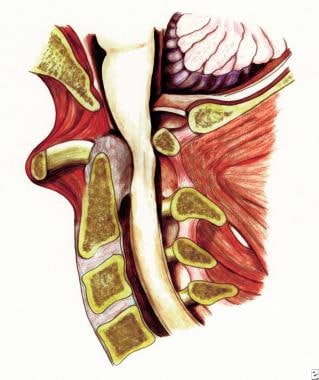 Rheumatoid spondylitis. Depiction of anterior subluxation of C1 on C2, retrodental pannus, and osseous erosions; the spinal cord is compressed between the pannus anteriorly and the posterior arch of the atlas.
Rheumatoid spondylitis. Depiction of anterior subluxation of C1 on C2, retrodental pannus, and osseous erosions; the spinal cord is compressed between the pannus anteriorly and the posterior arch of the atlas.
The superior migration of the odontoid is attributed to erosion and bone loss in the occipitoatlantal and atlantoaxial joints (see the following images).
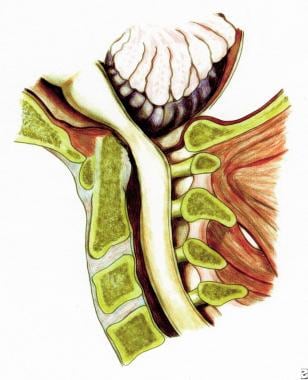 Rheumatoid spondylitis. Depiction of superior migration of the odontoid into the foramen magnum with compression of the spinal cord.
Rheumatoid spondylitis. Depiction of superior migration of the odontoid into the foramen magnum with compression of the spinal cord.
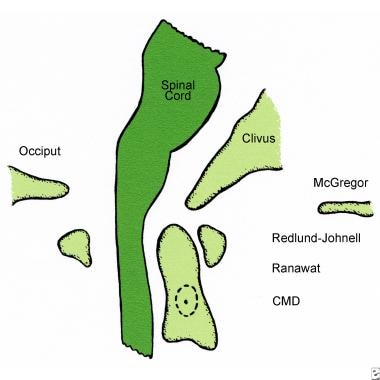 Rheumatoid spondylitis. Pertinent measurements of superior migration of the odontoid; cranial migration distance (CMD).
Rheumatoid spondylitis. Pertinent measurements of superior migration of the odontoid; cranial migration distance (CMD).
Subaxial subluxation results from destruction of the facets, intervertebral discs, and interspinous ligaments. In contrast to degenerative disik disease, involvement of C2-C3 and C3-C4 is common, and osteophytes are seldom seen.
Epidemiology
Numerous investigators have attempted to elucidate the natural history of rheumatoid arthritis (RA) as it affects the cervical spine, with wide variation in their findings. [8, 9, 10, 11, 12] With the increasing number of disease-modifying drugs available for treatment of RA, spine surgeons have anecdotally noted decreased rates of cervical spine surgical procedures in this patient population. [13]
Of the 0.8% of the white population in the United States and Europe affected by RA, neck pain is reported in 40-88% of patients. The prevalence of cervical spine involvement in RA ranges from 25% to 80%, depending on the diagnostic criteria applied. [14] However, only 7-34% of patients with RA have a neurologic deficit. A substantial number of patients with radiographic instability or neck pain do not develop neurologic deficits. [15]
Involvement of the cervical spine typically begins early in the disease process and often parallels the extent of peripheral disease. Of the 3 types of involvement, atlantoaxial instability (AAI) is the most common, occurring in up to 49% of patients. [16] Most of these subluxations are anterior, while approximately 20% are lateral and approximately 7% are posterior. Superior migration of the odontoid (SMO) is seen in up to 38% of patients with RA. Subaxial subluxation is seen as a discrete pathologic entity in 10-20% of patients.
A meta-analysis of 2750 patients with RA found that the following are significant risk factors for cervical spine involvement in in RA [17] :
-
Female sex
-
Positive rheumatoid factor
-
Long‐term corticosteroid treatment
-
Peripheral joint erosions
-
Younger age
-
Long duration of RA
-
Markers of higher disease activity (ie, elevated erythrocyte sedimentation rate [ESR], C-reactive protein [CRP] level, Disease Activity Score [DAS])
Subaxial subluxation (SAS) also develops after previous upper cervical fusions. [18] In one series of 25 patients, 48% developed SAS following atlantoaxial fusion. However, further surgery was not needed for SAS up to 5 years after the initial surgery. [19]
Prognosis
The likelihood of cervical involvement appears to increase with the duration of rheumatic disease. Many patients with pain and radiographic criteria for instability do not develop neurologic sequelae; neurologic deficit is seen only in 7-34% of cases. However, 10% of patients with atlantoaxial subluxation (AAS) from rheumatoid arthritis may die from brainstem compression that is unrecognized before their sudden death. [20]
Rheumatoid arthritis is a systemic disorder, and patients may have varying degrees of generalized debilitation. [21] The postoperative course of such patients can be complicated by fragile skin and poor wound healing. Poor preoperative nutritional status and corticosteroid dependence may potentiate wound-healing problems and predispose toward infection. [22]
Age, sex, duration of paralysis, preoperative atlantodental interval (ADI), and percentage of slippage in subaxial subluxations all have been found to have no correlation with neurologic recovery. The degree of preoperative neurologic deficit has been shown to correlate with neurologic recovery. The results appear to be less favorable in patients with more advanced preoperative neurologic deficits. Casey and colleagues reported that in patients classified as Ranawat class III, 58% of ambulatory patients (grade IIIA) attained a grade I or grade II after surgery. Conversely, only 20% of nonambulatory patients (grade IIIB) improved to grade I or grade II postoperatively. [23]
Radiographic parameters also have been shown to predict postoperative neurologic recovery. Boden et al reported that patients with AAS whose posterior ADI (PADI) was less than 10 mm before surgery had poor return of motor function. [24] With superimposed SMO, clinically significant neurologic recovery was seen only when the PADI was at least 13 mm before surgery. For patients with subaxial subluxations, less recovery was seen in those with a residual postoperative subaxial canal diameter of less than 14 mm.
Cervical fusion in patients with rheumatoid spondylitis has a clinical success rate of 60-90%. [25, 26, 27, 28, 29, 30, 31] This wide range is partly due to the definition of clinical success and by variation in disease severity at the time of surgery. Rates of neurologic improvement also vary widely, ranging from 27-100%. [25, 26, 27, 28, 29, 32, 33, 34] Peppelman et al reported that 95% of 90 patients treated surgically for AAS improved by at least one Ranawat grade, 76% of patients with combined AAS and superior migration of the odontoid (SMO) had neurologic improvement, and 94% of those surgically treated for isolated subaxial subluxation also showed neurologic improvement. [35]
A study of the National Readmission Database found that in RA patients who underwent cervical spine fusion from 2013 to 2014, 691 of the 5597 patients (12.3%) were readmitted within 90 days. Readmission was most often due to postoperative infection (septicemia, urinary tract infection, pneumonia, wound infection). [36]
A study comparing surgical outcome between transarticular screw fixation (TAF) and C1 lateral mass-C2 pedicle screw fixation (C1LM-C2P) in 58 patients with atlantoaxial instability found no statistical significance in fusion rate, clinical outcomes, or complications. Bone fusion was achieved in 97% of patients who received TAF and 100% of patients who underwent C1LM-C2P. Complications (regardless of neurologic deterioration) were cable loosening and screw malposition in the TAF group and violation into the vertebral canal and spinal canal in the C1LM-C2P group. [37]
Nonunion rates in this population have been estimated at 5-20%. Many of these nonunions may be asymptomatic, so management should be individualized.
Some airways are difficult to intubate. Excessive trauma during intubation may be responsible for postoperative breathing problems. In a review of 128 consecutive posterior operations on the cervical spine for problems related to rheumatoid arthritis, Wattenmaker et al reported a 14% incidence of upper airway obstruction after extubation in patients intubated without fiberoptic assistance, compared with a 1% incidence in patients intubated fiberoptically. [38]
The perioperative mortality rate has been reported to be as high as 5-10%. However, the mortality rate may relate to the severity of the underlying disease and not to the surgery itself. [39]
Presentation
Rheumatoid involvement of the cervical spine is just one element in a systemic disease process. Cervical involvement often correlates with the degree of hand and wrist erosion. Cervical involvement also has been associated with the presence of rheumatoid nodules and the use of corticosteroids. Classically, craniocervical neck pain often is associated with occipital headaches.
Symptoms
Compression of the C2 sensory fibers supplying the nucleus of the spinal trigeminal tract can cause facial pain. Compression of the C2 sensory fibers supplying the greater auricular nerve may result in ear pain. Occipital neuralgia results from compression of the C2 sensory fibers supplying the greater occipital nerve.
A history of myelopathic symptoms should be sought carefully. Patients may experience weakness, decreased endurance, gait difficulty, paresthesias of the hands, and loss of fine dexterity. Limb paresthesias and bowel and/or bladder disturbance may develop.
Vertebrobasilar insufficiency may be found, particularly in patients with atlantoaxial instability (AAI). Complaints may include vertigo, loss of equilibrium, visual disturbances, tinnitus, and dysphagia. Similar symptomatology can also be caused by mechanical compression of the brainstem.
In some patients with AAI, neck flexion produces crepitation or a sensation of the head “falling forward”. This may be reproduced on physical examination, in which a palpable “clunk" may be appreciated on neck flexion, [40] Neck motion may also elicit shocklike sensations through the torso or into the extremities (ie, Lhermitte sign).
Physical findings
Inventory of these patients' condition frequently is confounded by the severity of their peripheral rheumatoid involvement. Weakness in these patients can also be due to tenosynovitis, tendon rupture, muscular atrophy, peripheral nerve entrapment, or articular involvement, making neurologic impairment less obvious. Signs of myelopathy should raise suspicion of cervical involvement. Rarely, cranial nerve dysfunction can occur secondary to compression of the medullary nuclei by the odontoid. Other rare findings in patients with advanced brainstem compression include vertical nystagmus and Cheyne-Stokes respirations.
Classification of Neurologic Deficits
The Ranawat classification can be used to categorize patients with rheumatoid myelopathy on the basis of their clinical history and physical findings. [41] This classification has some utility in determining the potential for neurologic recovery following surgery and is categorized as follows [41] :
-
Class I - No neural deficit
-
Class II - Subjective weakness, dysesthesias, and hyperreflexia
-
Class IIIA - Objective weakness and long-tract signs; patient remains ambulatory
-
Class IIIB - Objective weakness and long-tract signs; patient no longer ambulatory
Workup Overview
Rheumatoid factor seropositivity has been correlated with more extensive cervical involvement. The use of rheumatoid factor as a predictor of neurologic involvement has not been established; therefore, it does not have a role in the surveillance of patients with rheumatoid arthritis with cervical involvement.
All patients with rheumatoid arthritis should have radiographic examination of the cervical spine because cervical involvement can remain asymptomatic. Imaging modalities include plain radiography, magnetic resonance imaging (MRI), polytomography, and computed tomography (CT) scanning. [42] Although prediction of the onset of myelopathy in any particular patient is difficult, studies of large populations of patients have sought to establish parameters for predicting neurologic involvement via imaging studies. [15, 43, 44]
Plain Radiography
The initial imaging assessment in suspected rheumatoid spondylitis should consist of plain radiographs of the cervical spine, including lateral flexion and extension views. Several measurements that can help direct management can be made on plain radiographs. [45]
AADI measurement
Traditionally, the anterior atlantodental interval (AADI) has been used to monitor patients with rheumatoid arthritis over time. The AADI is the distance from the posterior margin of the anterior ring of C1 to the anterior surface of the odontoid. An AADI of more than 3 mm in an adult or 4 mm in a child is considered abnormal. Various authors have recommended surgery for values of more than 8 mm, 9 mm, or 10 mm (see Surgical Management).
Although the AADI was used commonly to monitor patients with cervical involvement, a number of investigations have shown that the AADI does not reliably discriminate between patients who are neurologically intact from those with neural deficit. [46] This is due in part to the 3-dimensional changes that take place with progressive subluxation. As the deformity progresses, the anterior arch of the atlas displaces in an anteroinferior direction as superior migration of the odontoid (SMO) combines with atlantoaxial instability (AAI). With continued SMO, the AADI decreases, although this vertical translocation is associated with a more unfavorable prognosis.
Boden and associates demonstrated this pitfall by examining the sensitivity, specificity, accuracy, and positive and negative predictive values of the AADI in predicting paralysis based on varying critical intervals (see the table below). [24] For example, raising the cut-off value for the AADI from 8 mm to 10 mm increases the specificity from 58% to 90% but decreases the sensitivity from 59% to 35%.
PADI measurement
Anterior atlantoaxial subluxation may also be assessed by the posterior atlantodental interval (PADI), as measured from the posterior aspect of the odontoid to the anterior margin of the lamina of C1. Because the synovial pannus may occupy 1-3 mm of the retro-odontoid space, this interval does not represent the true space available for the cord. The PADI has been recommended as a more reliable predictor of whether neurologic compromise will develop.
The PADI was compared with the traditional AADI in a long-term series involving 73 patients. [24] Using a critical PADI of 14 mm or less resulted in a sensitivity (ability to detect those with paralysis) of 97%, a level superior to that using the AADI. More importantly, the negative predictive value, using a critical PADI of 14 mm, rises to 94%. Therefore, if the PADI is greater than 14 mm, there is a 94% chance that the patient will not have paralysis. Such a high negative predictive value makes the PADI extremely reliable as a screening test.
For comparison of the AADI and the PADI, see the table below.
Table. Reliability of the Anterior (AADI) and Posterior (PADI) Atlantodental Intervals in Predicting Paralysis in Patients with Rheumatoid Arthritis (Open Table in a new window)
Test |
Result |
Sensitivity (%) |
Specificity (%) |
Accuracy (%) |
PPV (%) |
NPV (%) |
AADI |
8 mm or greater |
59 |
58 |
58 |
61 |
56 |
9 mm or greater |
41 |
77 |
58 |
67 |
55 |
|
10 mm or greater |
35 |
90 |
62 |
80 |
56 |
|
11 mm or greater |
18 |
97 |
55 |
86 |
52 |
|
PADI |
12 mm or less |
76 |
90 |
83 |
90 |
78 |
13 mm or less |
91 |
71 |
82 |
78 |
88 |
|
14 mm or less |
97 |
52 |
75 |
69 |
94 |
|
These numbers were calculated from a series of 73 patients. NPV = negative predictive value; PPV = positive predictive value. (Reprinted with permission from Boden SD, Dodge LD, Bohlman HH, Rechtine GR. J Bone Joint Surg Am. Sep 1993;75(9):1282-97. [24] ) |
||||||
SMO assessment
A variety of measurements have been used to assess SMO. All of these measurements attempt to identify and grade the degree of odontoid encroachment on space normally occupied by the spinal cord and brainstem. Unfortunately, many of these are difficult to reproduce. The image below depicts a few pertinent measurements.
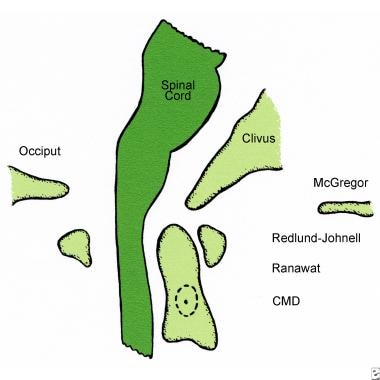 Rheumatoid spondylitis. Pertinent measurements of superior migration of the odontoid; cranial migration distance (CMD).
Rheumatoid spondylitis. Pertinent measurements of superior migration of the odontoid; cranial migration distance (CMD).
The McGregor line has become the most consistent reference, because it connects the posterior margin of the hard palate to the most caudal point of the occiput. Vertical settling is defined here by migration of the odontoid by more than 4.5 mm above this line.
The Redlund-Johnell line assesses the occiput-to-C2 complex. The value measures the distance between the midpoint of the inferior margin of the body of the axis to the McGregor line. Values less than 34 mm in males and 29 mm in females are considered abnormal and correlate with increased risk of neurologic injury. [47]
The Ranawat index targets disease in the C1-C2 segment by utilizing a lateral radiograph. A line is drawn from the pedicles of C2 superiorly along the vertical axis of the odontoid until it intersects a line connecting the anterior and posterior arches of C1. A value less than 13 mm is diagnostic of vertical settling.
The McRae line connects the front of the foramen magnum to the back. The upper tip of the odontoid process should not project above this line and should normally be 1 cm below the anterior margin of the foramen magnum.
The Chamberlain line is drawn from the posterior margin of the hard palate to the posterior margin of the foramen magnum. Projection of the tip of the odontoid 6 mm above this line is considered pathologic. However, the margins of the foramen magnum are frequently difficult to delineate without a tomogram.
Subaxial vertebral subluxations
Plain radiographs are also useful in detecting subaxial vertebral subluxations. Historically, these subluxations have been quantitated on lateral cervical radiographs as translation forward in millimeters or as a percentage slip of the total anteroposterior diameter of the inferior vertebral body. More recently, however, the sagittal diameter of the subaxial canal has been shown to correlate with the presence and degree of paralysis more often than does the percentage of vertebral slip. Patients with canal diameters of 13 mm or less are at higher risk for neurologic involvement.
The following image depicts a cervical radiograph from a patient with combined SMO and subaxial subluxation who underwent occipitocervical fusion and lateral mass plating.
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) has provided an increased ability to visualize the extent of spinal cord compression, particularly when due to pannus. [48] Dvorak and colleagues showed that two thirds of patients with atlantoaxial subluxation (AAS) have a pannus of greater than 3 mm in diameter. [49] Therefore, the bony canal diameter measured on plain radiographs may not represent the true space available for the cord. Kawaida et al demonstrated spinal cord compression in all patients with rheumatoid arthritis when the space available for the cord (as measured on MRI) was 13 mm or less. [50]
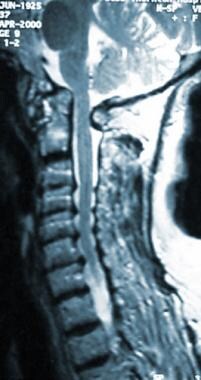
On MRI, the cervicomedullary angle is an effective indicator of cord distortion from superior migration of the odontoid (SMO). This angle incorporates lines drawn along the anterior aspects of the cervical cord and along the medulla. The normal range is 135-175°. Angles less than 135° indicate basilar invagination and have been associated with myelopathy (see the image below for a patient example).
Polytomography and CT Scanning
Historically, tomograms were useful for quantitating the degree of basilar invagination and to measure the anterior (AADI) and posterior (PADI) atlantodental intervals more accurately in patients with abnormal radiographs. However, computed tomography (CT) scanning with sagittal and coronal reformatting has largely supplanted biplanar tomography. A CT scan combined with intrathecal contrast provides excellent bony detail and the ability to detect spinal cord compression from synovial pannus.
Although the noninvasive nature of magnetic resonance imaging (MRI) has made it the preferred modality for this type of evaluation, CT myelography is useful for patients with contraindications to MRI.
Treatment Overview
An approach to surgical and nonsurgical management for rheumatoid arthritis and for rheumatoid spondylitis can be developed based on the natural history of rheumatoid involvement of the cervical spine and radiographic predictors of paralysis.
As suggested by Boden, 3 goals should be kept in mind. [51] The first goal is to avoid the development of an irreversible neurologic deficit, as patients with more severe deficits have less recovery and higher morbidity. A second goal is to prevent sudden death from unrecognized neural compression, as has been reported in up to 10% of deaths in rheumatoid arthritis. [20] Finally, as one half of patients with rheumatoid arthritis with radiographic evidence of instability remain asymptomatic, it is best to avoid surgery if the patient can be identified as being one who will most likely not develop neurologic problems.
Nonsurgical Management
Nonoperative treatment of rheumatoid involvement of the cervical spine is supportive. Early aggressive medical management is important in the global sense, as cervical involvement has been correlated with disease activity. Collars can be used for comfort purposes. Rigid cervical collars most likely do not prevent subluxation; however, they may prevent reduction of a deformity by limiting extension. [52, 53] Skin sensitivity in this population also causes problems with rigid orthoses. Patients being monitored need careful surveillance for long-tract signs or for radiographic findings suggesting impending neurologic compromise (see Plain Radiography).
Surgical Intervention
The identification of a subset of patients with impending neurologic deficit has been elusive due to the poor correlation of neurologic symptoms with radiographic indicators of instability. Therefore, universally accepted surgical indications have been slow to develop. However, patients with rheumatoid arthritis or, particularly, rheumatoid spondylitis, who have refractory pain, clearly evident neurologic compromise, or intrinsic spinal cord signal changes on magnetic resonance imaging (MRI) are generally candidates for surgical intervention.
Controversy surrounds treatment for patients with little or no pain, no neural deficit, and radiographs suggestive of instability. To facilitate understanding of the operative indications and perioperative details, categorization of these patients by their pathologic lesion is helpful. [54, 55, 56, 57, 58, 40]
Contraindications to surgery for rheumatoid spondylitis include medical conditions that suggest the patient would not tolerate the stress of surgery, such as unstable angina or a recent myocardial infarction or stroke. [59] Active infection with likely bacteremia would also be a relative contraindication to surgery, especially in the setting of planned instrumentation. The patient's medical condition should be optimized before proceeding with any planned surgical intervention.
Atlantoaxial subluxation
Patients with AAS and no symptoms or signs of myelopathy can be observed when their lateral cervical radiograph shows a posterior atlantodental interval (PADI; the interval from the posterior aspect of the odontoid to the anterior margin of the lamina of C1) greater than 14 mm. Patients whose PADI measures less than 14 mm should have a magnetic resonance imaging (MRI) study to determine the true space available for the spinal cord. MRI findings of less than 13 mm of space available for the spinal cord and a cervicomedullary angle of less than 135° are generally indications for surgical stabilization.
The type of procedure performed is determined by whether or not the subluxation is reducible, the individual surgeon's preference and experience, and the patient's condition. If the deformity is reducible, posterior atlantoaxial fusion can be accomplished by a variety of techniques. [60]
Gallie reported a technique for posterior atlantoaxial arthrodesis in 1939, a technique that has been used with different modifications since then. [61] In essence, the procedure consists of a block of autologous bone graft fixed by wire loop to the posterior arch of the atlas and the spinous process of the axis. Although technically straightforward to perform, rotational stability and translational stability are inferior to other techniques. The image below depicts a modified Gallie fusion.
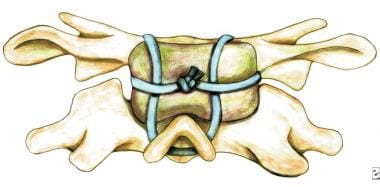 Rheumatoid spondylitis. Modified Gallie fusion. Note the H-shaped bone block wired over the spinous process of C2.
Rheumatoid spondylitis. Modified Gallie fusion. Note the H-shaped bone block wired over the spinous process of C2.
The Brooks fusion uses 2 posterior paramedian autologous structural grafts, usually attached with sublaminar wires. The bilateral fixation improves rotational stability. Multistrand titanium cables are increasingly favored over monofilament stainless steel wires because of greater strength and ease of contouring, as well as postoperative magnetic resonance imaging (MRI) and computed tomography (CT) scan imaging qualities. However, all techniques that use sublaminar wire or cable fixation have the potential risk of spinal cord injury during passage or from late failure of the implants. Additionally, the posterior arch of the atlas may be osteoporotic or partially deficient, thereby limiting its use. The image below depicts a Brooks-type fusion.
 Rheumatoid spondylitis. Brooks-type fusion. Rectangular structural grafts are beveled to fit between the arches of C1 and C2; then they are secured by bilateral doubled-twisted wires.
Rheumatoid spondylitis. Brooks-type fusion. Rectangular structural grafts are beveled to fit between the arches of C1 and C2; then they are secured by bilateral doubled-twisted wires.
Immediate multidirectional stability can be achieved by C1-C2 transarticular screw fixation, as shown in the following image. [62]
The screws are inserted posteriorly by entering the inferior aspect of the facet of C2, crossing the C1-C2 facet joint, and then entering into the lateral mass of C1. Safe insertion requires thorough understanding of the upper cervical anatomy and exposure of the medial border of the C2 pedicle. [63] A preoperative CT scan should be reviewed carefully, because some C2 pedicles may have a small diameter, the lateral mass may be partially resorbed, or the vertebral artery may course superomedially. These conditions preclude safe transarticular screw placement. If there is good bone in the lateral masses, the patient may require only a cervical collar. However, patients with poor fixation may require a halo device postoperatively.
Patients with irreducible deformity and posterior compression can be treated with a C1 laminectomy and transarticular stabilization. Patients who have irreducible deformity and bony anterior compression may be decompressed by an anterior transoral approach, particularly in end-stage conditions. [64, 65] This route has several difficulties, such as limited opening of the mouth in patients with concomitant temporomandibular disease, postoperative infection, and pharyngeal mucosal edema. However, several authors have reported good results using this procedure. This technique is generally followed by posterior stabilization as a 2-stage, same-day procedure.
Iacoangeli and colleagues reported that endoscopic endonasal odontoidectomy (EEO) with anterior C1 arch sparing provided satisfying long-term results for irreducible ventral craniovertebral junction (CVJ) lesions in 17 patients with rheumatoid arthritis. Moreover, the preservation of anterior C1 arch and the reconstruction of anterior CVJ prevented the need for posterior fusion in 2 patients. [66]
Patients who are healthier (Ranawat class I and class II) (see Classification of Neurologic Deficits) may be treated adequately with atlantoaxial stabilization and fusion alone, even in the presence of irreducible deformity. Some authors recommend that patients with anterior cord compression from a proliferative retrodental pannus be treated with ventral transoral decompression. However, there has been documented resorption of a retrodental pannus if a stable posterior fusion is achieved. [67] Of these options, initial treatment with a posterior fusion followed by MRI and clinical follow-up is the most common. If the pannus does not resorb and neurologic deficit persists, late transoral decompression can be performed.
Superior migration of the odontoid
Even in the absence of neurologic deficit, patients with any degree of basilar invagination should have an MRI study in flexion to evaluate spinal cord compression. Surgical treatment should be considered in any patient with cord compression or neurologic deficit. Preoperatively, cervical traction can be used to attempt a gradual reduction.
Occipitocervical fusion is the procedure of choice in patients with SMO. Several devices have been described, ranging from wire loops securing tricortical bone graft supplemented with cement or metal mesh, contoured rods, and more recently, plates and screws (see the image below). [68, 69]
 Rheumatoid spondylitis. Occipitocervical fusion combined with lateral mass plating for a patient with combined superior migration of the odontoid and subaxial subluxation. Courtesy of Steven R. Garfin.
Rheumatoid spondylitis. Occipitocervical fusion combined with lateral mass plating for a patient with combined superior migration of the odontoid and subaxial subluxation. Courtesy of Steven R. Garfin.
The more rigid fixation afforded by plating has been associated with a lower pseudarthrosis rate when compared with wiring techniques. [70] Occipitocervical fusion with plating generally involves screw placement into the C2 pedicles under fluoroscopic guidance through a precontoured plate. This allows easier subsequent placement of subaxial screws in the lateral masses and in the occiput. Screws are usually not placed above the inion to avoid the intracranial venous sinuses.
Although the inner table can be thin in places, holes drilled 2-3 cm from the midline, halfway between the foramen magnum and the transverse sinus, are generally safe. No matter which implant technique is used, autologous bone grafting should always be performed. If the deformity is irreducible in traction, decompression either posteriorly or anteriorly (based on the location of the compression) should be considered as an adjunct to the fusion, as discussed above. Anterior compression in these patients is predominantly osseous, not from synovial pannus. Therefore, a ventral route provides more reliable decompression.
Subaxial subluxation
Patients with subaxial subluxation and no evidence of neurologic deficit can be observed. Plain radiographs are sufficient for surveillance. Patients with a bony canal diameter less than 14 mm should have an MRI evaluation to assess the true space available for the spinal cord. If the space available for the spinal cord is less than 13 mm or if significant segmental hypermobility is present, surgical consideration is warranted.
Most patients with subaxial subluxation can be treated with posterior cervical fusion using autograft bone. Internal fixation with wires, plate-screw, or rod-screw constructs allows for earlier mobilization and increased rates of fusion. Patients with irreducible subluxations or significant neurologic deficit may best be treated with anterior decompression and fusion alone or in concert with posterior fusion. [71]
Combined subluxations
Some patients may have upper cervical involvement as well as early subaxial subluxation. In these instances, the fusion should be extended to include the involved subaxial segments to avoid early deterioration of borderline subluxations below a rigid upper cervical fusion (see the image below).
 Rheumatoid spondylitis. Occipitocervical fusion combined with lateral mass plating for a patient with combined superior migration of the odontoid and subaxial subluxation. Courtesy of Steven R. Garfin.
Rheumatoid spondylitis. Occipitocervical fusion combined with lateral mass plating for a patient with combined superior migration of the odontoid and subaxial subluxation. Courtesy of Steven R. Garfin.
Postoperatively, the type of orthosis used in those with combined subluxations is often best determined on an individualized basis. Many patients have porotic bone of both the posterior elements and of the structural graft harvested from the iliac crest. Upper cervical fusions in such patients may best be managed postoperatively in a halo. When rigid collars are used, careful surveillance of the skin is mandatory to avoid decubiti. Also, if temporomandibular joint (TMJ) involvement is present, eating (chewing) may be a problem in a cervical-thoracic orthosis (CTO).
Long-term Monitoring
Patients treated nonoperatively need careful surveillance for long-tract signs or for radiographic findings that suggest impending neurologic compromise. Even after achieving a successful fusion, patients with rheumatoid spondylitis must continue to have long-term follow-up. Subaxial instability can develop below upper cervical fusions, so radiographic follow-up should be obtained periodically, even in patients who are asymptomatic.
Questions & Answers
Overview
What is rheumatoid arthritis (RA) of the cervical spine?
What is the prevalence of rheumatoid arthritis (RA) of the cervical spine?
What is the prognosis of rheumatoid arthritis (RA) of the cervical spine?
What are the signs and symptoms of rheumatoid arthritis (RA) of the cervical spine?
Which physical findings are characteristic of rheumatoid arthritis (RA) of the cervical spine?
How are the neurologic deficits of rheumatoid arthritis (RA) of the cervical spine classified?
What is included in the workup to evaluate rheumatoid arthritis (RA) of the cervical spine?
What is the role of radiography in the workup of rheumatoid arthritis (RA) of the cervical spine?
What is the role of SMO assessment in the workup of rheumatoid arthritis (RA) of the cervical spine?
How are subaxial vertebral subluxations assessed in rheumatoid arthritis (RA) of the cervical spine?
What is the role of MRI in the workup of rheumatoid arthritis (RA) of the cervical spine?
What is the role of CT scanning in the workup of rheumatoid arthritis (RA) of the cervical spine?
How is rheumatoid arthritis (RA) of the cervical spine treated?
What is included in supportive care for rheumatoid arthritis (RA) of the cervical spine?
What is the role of surgery in the treatment of rheumatoid arthritis (RA) of the cervical spine?
What is included in the long-term monitoring of rheumatoid arthritis (RA) of the cervical spine?
What is the pathophysiology of rheumatoid arthritis (RA) of the cervical spine?
-
Rheumatoid spondylitis. Depiction of anterior subluxation of C1 on C2, retrodental pannus, and osseous erosions; the spinal cord is compressed between the pannus anteriorly and the posterior arch of the atlas.
-
Rheumatoid spondylitis. Depiction of superior migration of the odontoid into the foramen magnum with compression of the spinal cord.
-
Rheumatoid spondylitis. Pertinent measurements of superior migration of the odontoid; cranial migration distance (CMD).
-
Rheumatoid spondylitis. MRI of a patient with superior migration of the odontoid and subaxial subluxation. Courtesy of Steven R. Garfin.
-
Rheumatoid spondylitis. Modified Gallie fusion. Note the H-shaped bone block wired over the spinous process of C2.
-
Rheumatoid spondylitis. Brooks-type fusion. Rectangular structural grafts are beveled to fit between the arches of C1 and C2; then they are secured by bilateral doubled-twisted wires.
-
Rheumatoid spondylitis. C1-C2 transarticular screw fixation. Courtesy of Steven R. Garfin.
-
Rheumatoid spondylitis. Occipitocervical fusion combined with lateral mass plating for a patient with combined superior migration of the odontoid and subaxial subluxation. Courtesy of Steven R. Garfin.
Tables
What would you like to print?
- Practice Essentials
- Pathophysiology
- Epidemiology
- Prognosis
- Presentation
- Classification of Neurologic Deficits
- Workup Overview
- Plain Radiography
- Magnetic Resonance Imaging
- Polytomography and CT Scanning
- Treatment Overview
- Nonsurgical Management
- Surgical Intervention
- Long-term Monitoring
- Questions & Answers
- Show All
- Media Gallery
- Tables
- References