Practice Essentials
The posterior cruciate ligament (PCL) of the knee has been the subject of many debates. The role of the PCL has become a topic of interest across the subspecialties of trauma, sports medicine, [1] and knee arthroplasty. What, if any, treatment is required for a PCL-deficient knee is still a widely debated topic.
Isolated PCL injuries are defined by the degree of posterior translation of the tibia with respect to the distal femoral condyles with the knee in 90° of flexion. These injuries can be tears in continuity or complete ruptures of the PCL.
The consequences of an isolated PCL injury are poorly understood. PCL reconstruction has been advocated to restore knee kinematics to normal, which decreases the perceived risk of early degenerative joint disease.
Many procedures have been described that are no longer in general use and are mentioned here only for the sake of completeness and historical interest. These were nonanatomic reconstructions using transfers of various structures, including the medial head of the gastrocnemius, the popliteus, and the semimembranosus. [2] Current reconstruction is anatomic and attempts to recreate the PCL in the same manner as is done in anterior cruciate ligament (ACL) reconstruction.
Although the development of early degenerative disease is controversial and has not been proved with clinical studies, the ability to restore normal knee kinematics with PCL reconstruction has also not been demonstrated in vivo. Thus, the PCL continues to be a topic of research and debate.
Anatomy
The PCL originates from the junction of the femoral notch roof and the medial femoral condyle roughly 1 cm proximal to the articular surface. [3] The insertion of the PCL is on the posterior aspect of the proximal tibia at the fovea, a depression between the tibial plateaus 1 cm distal to the articular surface. [4] (See the images below.)
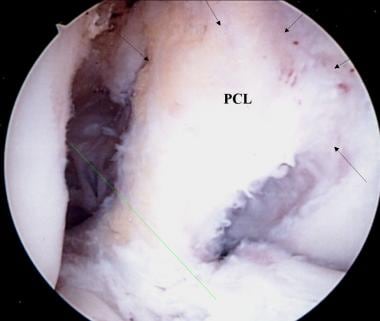 A view of the broad origin of the posterior cruciate ligament (PCL) on the medial femoral condyle of a left knee. The anterior cruciate has been removed for surgical reconstruction. Image courtesy of Janos P. Ertl, MD.
A view of the broad origin of the posterior cruciate ligament (PCL) on the medial femoral condyle of a left knee. The anterior cruciate has been removed for surgical reconstruction. Image courtesy of Janos P. Ertl, MD.
 An additional view of the posterior cruciate ligament (PCL) broad origin and insertion in a knee pending anterior cruciate ligament (ACL) reconstruction. Image courtesy of Janos P. Ertl, MD.
An additional view of the posterior cruciate ligament (PCL) broad origin and insertion in a knee pending anterior cruciate ligament (ACL) reconstruction. Image courtesy of Janos P. Ertl, MD.
The PCL is an intra-articular ligament but remains extrasynovial. [5, 6] The PCL is just medial to the center of the knee and averages 38 mm in length and 13 mm in thickness. [7] At its origin, the PCL averages 32 mm thickness, is narrowest at its mid substance, and then fans out to an average of 13 mm at its insertion. [7]
The PCL consists of two bundles, the anterolateral and posteromedial bundles. The anterolateral bundle originates anteriorly and inserts laterally. It is largest at the mid substance and is taut in flexion. The posteromedial bundle originates posteriorly and inserts medially. It is tight in extension and contains a small component that is isometric. [7, 8]
The vascular supply of the PCL depends in large part on the middle geniculate artery. A small component of the nutrient supply of the PCL is contributed by the synovium. Capsular branches of the inferior geniculate and popliteal arteries supply the PCL insertion. [9]
Fibers of the posterior articular nerve, a branch of the tibial nerve, are in the posterior capsule and the synovium lining the cruciate ligaments. [10] At the insertion of the cruciate ligaments, Golgi tendon–like organs are found and may play a role in proprioception. [11, 12]
The meniscofemoral ligaments contribute to the function of the PCL. The ligament of Humphrey is less than a third of the size of the PCL. It traverses anterior to the PCL origin and attaches to the posterior horn of the lateral meniscus. The ligament of Wrisberg is nearly half the size of the PCL. It traverses posterior to the PCL origin and inserts onto the posterior horn of the lateral meniscus. [13]
Pathophysiology
The PCL is stronger than its counterpart, the ACL, and it is less frequently injured. [14, 15] The PCL is the primary restraint to posterior tibial translation between 30° and 90°. At 90°, the PCL accepts 95% of posterior translational forces. [16] The in-situ forces of the PCL are 36 N in knee extension and 112 N in knee flexion. [17] Quadriceps and popliteus loading and weightbearing decreases the in-situ PCL forces, whereas hamstring loading increases the forces. [18, 19, 20]
Gollehon et al applied a 100 N posterior load to cadaver knees at 90° of flexion and reported that the normal posterior translation was 5 mm. [21] After isolated PCL sectioning, the posterior translation increased to 16 mm, whereas isolated lateral collateral ligament (LCL) and deep ligament complex sectioning increased the posterior translation by less than 3 mm. Sectioning of the PCL combined with sectioning of the LCL and deep ligament complex resulted in 25-30 mm translation; this amount was consistent throughout all positions of knee flexion.
The authors concluded that the PCL is the only primary restraint to posterior translation throughout the entire knee range of motion (ROM). Secondary restraints have a decreased role between 60° and 90° of knee flexion. With isolated PCL sectioning, external rotation and varus stability of the knee remained unchanged. [21]
The tensile strength of the PCL is greater than that of the ACL. [14] The ultimate load of the PCL, averaging 1627 N, is also greater than that of the ACL. [15, 22] The contributions to the PCL ultimate load of the anterolateral and posteromedial bundles remains controversial. [22, 23] The stiffness of the PCL averages 204 N/mm. [15]
The importance of the posteromedial bundle in bearing forces throughout knee ROM has been established. [18, 24, 25] Posteromedial-bundle forces have been found to exceed anterolateral-bundle forces in all angles of knee flexion. [18] Codominance of the anterolateral and posteromedial bundles has gained acceptance, instead of anterolateral bundle dominance. [24]
Etiology
Several mechanisms are responsible for PCL injuries. A direct posterior force on the proximal tibia with the knee flexed is commonly described. This mechanism occurs in dashboard injuries and in falls in which the foot is plantarflexed such that the tibial tubercle strikes the ground first. Hyperextension injuries of the knee are the most common cause of PCL tears from sports participation. Another mechanism related to sports injuries involves the combination of valgus and external rotation forces on a planted but unloaded lower extremity. The axial load of weightbearing is protective. [26, 27]
Epidemiology
The incidence of PCL injury is thought to be one tenth to one twentieth of that of ACL injury. [28] PCL injuries are present in 3.3-6.5% of all acute knee injuries. [29, 30]
Also, 40% of PCL injuries, including grade 1 and grade 2, are isolated injuries. [31] Some have estimated that 51% of PCL injuries are combined with other ligament injuries of the knee, most commonly the medial collateral ligament (MCL). [32, 33, 34] Grade 3 injuries are more likely to be combined injuries. However, many isolated PCL injuries are believed to be undiagnosed. About 2-5% of the participants at a National Football League Combine event were found to have isolated PCL laxity, and most could not recall having a significant injury. [35]
Prognosis
No series of acute isolated PCL reconstruction exists. The results in the literature are difficult to interpret because of variations in case selection and methods of evaluation. Techniques of reconstruction and the lengths of follow-up also vary. Consequently, the reported results vary.
Lipscomb et al reported the results for 25 patients with isolated acute or chronic PCL injuries treated with single-tunnel technique. At an average of 7 years after surgery, 60% had degenerative changes identified on radiographs.
Degenerative joint disease of the medial compartment is the most common late sequelae of PCL injury. Degeneration of the patellofemoral compartment also occurs, but less often.
Stannard et al reported the results of 30 multiligament knee injuries with PCL ruptures. This was the first reported series of PCL reconstructions using the combination of the tibial inlay technique and the double-tunnel technique. At a mean follow-up of 25 months, no statistical difference was found between injured knees and normal knees.
The outcome following PCL reconstruction for chronic PCL insufficiency has been worse than that of reconstruction for acute injuries. Postoperative posterior tibial laxity is greater after reconstruction for chronic PCL insufficiency than it is after acute PCL insufficiency, and patients with this injury cannot safely return to athletics. The diminished results of PCL reconstruction in patients with chronic knee insufficiency are thought to be the result of attenuation of the secondary restraints over time. PCL reconstruction inevitably fails if the posterolateral corner is insufficient or if the patient has developed a lateral thrust and the other pathology is not addressed.
Grade 1 and 2 PCL injuries have been reported to heal without any progression of posterior tibial laxity. Grade 3 tears do not heal and progressive laxity may develop as secondary and tertiary posterior tibial stabilizers are stressed over time.
-
Lateral radiograph of a normal knee. In a normal knee, a line drawn along the posterior femoral condyle does not intersect the posterior tibial condyle. Image courtesy of Janos P. Ertl, MD.
-
Lateral radiograph of a knee with a posterior cruciate ligament injury. Note that the same line as in the image above bisects the posterior tibial condyle due to a posterior sag and an incompetent PCL. Image courtesy of Janos P. Ertl, MD.
-
The photo on the left demonstrates the clinical finding of the posterior tibia sag sign. A line drawn parallel to the patella accentuates the posterior tibia sag. The photo on the right demonstrates the quadriceps active drawer test described by Daniels; with the knee in 70-90° of flexion, the extensor mechanism is contracted, pulling the tibia anteriorly into a reduced position. Image courtesy of Janos P. Ertl, MD.
-
Close-up view of a posterior tibia sag with an incompetent posterior cruciate ligament (PCL). Image courtesy of Janos P. Ertl, MD.
-
A view of the broad origin of the posterior cruciate ligament (PCL) on the medial femoral condyle of a left knee. The anterior cruciate has been removed for surgical reconstruction. Image courtesy of Janos P. Ertl, MD.
-
An additional view of the posterior cruciate ligament (PCL) broad origin and insertion in a knee pending anterior cruciate ligament (ACL) reconstruction. Image courtesy of Janos P. Ertl, MD.
-
A right knee pending posterior cruciate ligament (PCL) reconstruction. A minimal notchplasty is completed. Two guide pins are advanced into the medial femoral condyle for tunnel placement to reconstruct the two bundles of the PCL. Image courtesy of Janos P. Ertl, MD.
-
The two femoral tunnels are created by reaming from outside in; 8- to 9-mm tunnels are made depending on the patient size and graft used. Image courtesy of Janos P. Ertl, MD.
-
Two red Robinson catheters are advanced through the femoral tunnels. Image courtesy of Janos P. Ertl, MD.
-
The catheters have premade holes that are used for suture retrieval. Image courtesy of Janos P. Ertl, MD.
-
The catheters are advanced and threaded out the posterior knee. In this case, a posterior tibial inlay graft from an Achilles tendon allograft is used. The two bundles are secured to the catheters and advanced into the joint through the tunnels. Image courtesy of Janos P. Ertl, MD.
-
The two Achilles tendon bundles are secured with a baseball whipstitch, threaded through the catheter holes, and advanced into the femoral condyle tunnels. Image courtesy of Janos P. Ertl, MD.
-
Additional view of the placement and advancement of the Achilles allograft. Image courtesy of Janos P. Ertl, MD.
-
Completion and seating of the femoral allograft reconstruction. The two bundles are secured or stabilized by suturing over a post and washer. Note the re-establishment of the broad surface area for the reconstructed posterior cruciate ligament (PCL) origin. Image courtesy of Janos P. Ertl, MD.
-
Completion of the tibial inlay two-bundle Achilles tendon allograft/posterior cruciate ligament (PCL) reconstruction. The bony calcaneus remnant is secured to the posterior tibia with one or two interfragmentary compression screws into a trough into the posterior tibia at the level of the PCL insertion. Care is taken not to penetrate the anterior tibial cortex with these screws. Note the intact original anterior cruciate ligament (ACL). Image courtesy of Janos P. Ertl, MD.
-
Posterior sag of the left posterior cruciate ligament–deficient knee in comparison to the right knee. Note the posterior subluxation of the tibia relative to the femur of the left knee. Image courtesy of Robert Bronstein, MD.
-
Clinical examination photograph of a ruptured posterior cruciate ligament (PCL) confirmed on a posterior sagittal radiograph. Image courtesy of Mervyn J. Cross, MBBS, FRACS.
-
Radiograph depicting a chronic avulsed posterior cruciate ligament (PCL). Image courtesy of Mervyn J. Cross, MBBS, FRACS.
-
An MRI showing a torn posterior cruciate ligament (PCL). Image courtesy of Mervyn J. Cross, MBBS, FRACS.
-
Sagittal view radiograph showing a posterior cruciate ligament (PCL) rupture. Note the posterior positioning of the tibia in relation to the femur. Image courtesy of Mervyn J. Cross, MBBS, FRACS.





