Practice Essentials
Osteochondroma is a benign, cartilaginous neoplasm that is found in any bone that undergoes enchondral bone formation in its development. The World Health Organization (WHO) defines osteochondroma as a cartilage-capped bony projection on the external surface of a bone. [1] It is found most commonly around the knee and the proximal humerus; however, it can occur in any bone.
Osteochondroma is the most common benign bone tumor. Osteochondromas account for 20-50% of benign bone tumors [2] and 9% of all bone tumors. Most are asymptomatic, but they can cause mechanical symptoms depending on their location and size.
As benign lesions, osteochondromas have no propensity for metastasis. In fewer than 1% of solitary osteochondromas, malignant degeneration of the cartilage cap into secondary chondrosarcoma has been described and is usually heralded by new onset of growth of the lesion, new onset of pain, or rapid growth of the lesion. [3, 4, 5]
Historically and currently, most osteochondromas are incidental findings and are treated solely with observation. If they remain asymptomatic, they can be ignored. Lesions that create mechanical symptoms, become painful, begin to enlarge, or cause growth disturbance have historically been treated with surgical removal, and this remains the mainstay of treatment. (See Treatment.) Biologic therapies for osteochondromas may be possible in the future.
Anatomy
Osteochondromas can occur in many different locations in the body. Thus, a complete understanding of local anatomy is paramount to ensure that local structures are not harmed during surgical resection. Because these lesions arise from the metaphysis, particular care must be taken to avoid damage to the growth plate in the skeletally immature patient.
The osteochondroma may have a stalk and be defined as pedunculated, or it may have a broad base of attachment and be considered sessile. Whether the neoplasm is sessile or pedunculated, the medullary canal of the stalk and the bone are in continuity by definition. [6]
Pathophysiology
Osteochondroma is a hamartoma, and patients most commonly present in the second decade of life. Osteochondromas are located adjacent to growth plates and develop away from the growth plate with time because they are essentially isolated growth plates. They are affected by, and respond to, various growth factors and hormones in the same manner as epiphyseal growth plates.
Osteochondromas grow until skeletal maturity; growth generally stops once the growth plates fuse. [7] Slow growth from the cap may continue over time, as described by Virchow, but this usually stops by age 30 years.
Etiology
Although the exact etiology of these growths is not known, a peripheral portion of the physis is thought to herniate from the growth plate. This herniation may be idiopathic or may be the result of trauma or a perichondrial ring deficiency. Whatever the cause, the result is an abnormal extension of metaplastic cartilage that responds to the factors that stimulate the growth plate and thus results in exostosis growth.
This island of cartilage organizes into a structure similar to the epiphysis (see Histologic Findings). As this metaplastic cartilage is stimulated, enchondral bone formation occurs, developing a bony stalk. The histology of the cartilage cap reflects the classic defined zones observed in the growth plate—namely, proliferation, columniation, hypertrophy, calcification, and ossification.
This theory is thought to explain the classic finding of the osteochondroma associated with a growth plate and growing away from the physis while maintaining its medullary continuity. It is also thought to explain the clinical behavior of the exostosis growing only until skeletal maturity.
Genetic karyotyping has suggested that reproducible genetic abnormalities are associated with these benign growths and that they may actually represent a true neoplastic process, not a reactive one. [8] This research is ongoing, and further investigation is warranted.
Heinritz et al reported on the clinical findings and results of molecular analyses of the EXT1 and EXT2 genes—mutations of which lead to multiple osteochondroma—in 23 patients. [9] In 17 of the 23 patients, novel pathogenic mutations were identified (11 in the EXT1 gene; six in the EXT2 gene). According to the authors, findings of this study extend the mutational spectrum and understanding of the pathogenic effects of EXT1 and EXT2 mutations.
There is also evidence that various microRNAs (miRNAs) are abnormally expressed in osteochondroma tissues; some of them also participate in several major signaling pathways. [10] Thus, it is possible that regulation of miRNA expression may eventually become part of the treatment of osteochondroma.
Epidemiology
Osteochondromas are the most common benign bone tumors, representing 20-50% of all benign tumors [2] and 9% of all bone tumors. However, their actual frequency is not known, because many osteochondromas are not diagnosed. About 85% of osteochondromas are solitary, with the remainder occurring in the context of hereditary multiple exostoses. [11]
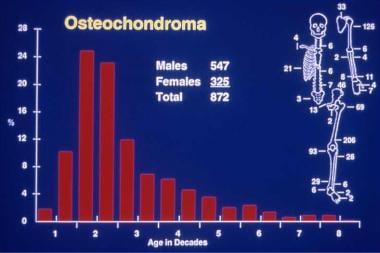
Osteochondromas can occur in any bone that undergoes enchondral bone formation, but they are most common around the knee. Spinal osteochondromas can occur but are rare. [12] Most osteochondromas are diagnosed in patients younger than 20 years (see the image below). A marked predilection for males exists (male-to-female ratio, 3:1). [13] Survivors of childhood cancer may be more likely to have these lesions. [14]
Prognosis
For solitary osteochondromas, the outcome and prognosis after surgery are excellent, with excellent local control and a local recurrence rate of less than 2%. [15, 16, 17, 18, 11] The process is a benign one; thus, the prognosis is usually one of complete recovery. Poorer outcomes usually are related to the morbidity associated with the exposure required to remove the lesion or associated with secondary bone deformity, but the latter is usually observed in the multiple hereditary form of the disease.
Florez et al performed a retrospective study of 113 solitary osteochondromas (most frequently located in the distal femur) that were treated between 1970 and 2002. [16] Six patients had a recurrence after treatment, and in two patients, the lesions became malignant and developed into chondrosarcoma. The authors noted that relapse of the exostosis is rare, occurring in approximately 2% of resections, and that growth of an osteochondroma or the presence of pain in older patients suggests a possible malignancy.
-
Solitary osteochondroma. Anteroposterior radiograph of a pedunculated osteochondroma of the distal femur.
-
Solitary osteochondroma. Lateral radiograph of a pedunculated osteochondroma of the distal femur. Orientation is away from the growth plate, and medullary continuity is clear.
-
Solitary osteochondroma. Lateral radiograph of a sessile osteochondroma of the distal femur.
-
Solitary osteochondroma. Anatomic and age distribution of solitary osteochondromas.
-
Solitary osteochondroma. CT scan of the pelvis depicting a massive solitary osteochondroma.
-
Solitary osteochondroma. Anteroposterior radiograph of sessile osteochondroma of the humerus.
-
Solitary osteochondroma. CT scan of the same sessile osteochondroma of the humerus as in Image 6.
-
Solitary osteochondroma. MRI of sessile osteochondroma of the femur demonstrating the thickness of the cartilage cap.
-
Solitary osteochondroma. Gross osteochondroma specimen at the time of resection. Bone stalk and overlying membrane on cartilage cap.
-
Solitary osteochondroma. Cut surface of surgical osteochondroma specimen. Cartilage cap and underlying bone with medullary continuity.
-
Solitary osteochondroma. Histology of cut osteochondroma specimen. Cartilage cap and orientation of enchondral bone formation.
-
Solitary osteochondroma. High-power view of benign cartilage cells arranged in vertical growth plate pattern.
-
Solitary osteochondroma. Radiograph demonstrating the deformation of the distal tibiofibular joint in a patient with a solitary osteochondroma.