Practice Essentials
The prevalence of low back and neck pain, which are thought to be associated with degenerative changes in the intervertebral disk, represents a major epidemiologic problem. In the United States, back pain is the second leading symptom that prompts visits to physicians. As many as 80% of adults in the United States experience at least one episode of low back pain during their lifetime, and 5% experience chronic problems. [1] An understanding of degenerative disk disease is important for managing these patients. (See the images below.)
The cascade of degenerative changes seen in degenerative disk disease can be subdivided into the following three stages (see Presentation):
-
Dysfunction
-
Instability
-
Restabilization
The duration of the stages varies greatly, and distinguishing the signs and symptoms from one stage to the next is difficult.
Conservative treatment of degenerative disk disease includes the following (see Treatment):
-
Back education and back school
-
Exercise
-
Medications
-
Physical modalities
-
Injections
Surgical treatment is used in approximately 5% of patients and includes the following:
-
Lumbar procedures
-
Cervical procedures
Anatomy
Vertebral anatomy
The spine is composed of seven cervical vertebrae, 12 thoracic vertebrae, five lumbar vertebrae, and a fused set of sacral and vestigial coccygeal vertebrae. Spine stability is the result of three columns in one, as described by Dennis. Fracture or loss of two columns results in instability.
The anterior column consists of the anterior longitudinal ligament and the anterior portion of the vertebral body. The middle column consists of the posterior wall of the vertebral body and the posterior longitudinal ligament. The posterior column is formed by the posterior bony arch; this consists of transverse processes, facets, laminae, and spinous processes.
Intervertebral disks form one quarter of the total length of the spinal column. Each vertebra has the potential for 6° of freedom, translation in all three axes of movement, and rotation around each axis. Not all vertebrae are created equal; the cervical vertebrae have the greatest freedom of flexion, extension, lateral rotation, and lateral flexion. This is because they are larger, they have concave lower and convex upper vertebral body surfaces, and they have transversely aligned facet joints.
Thoracic vertebrae have restricted flexion, extension, and rotation but freer lateral flexion because they are attached to the rib cage, are smaller, have flatter vertebral surfaces, have frontally aligned facet joints, and have larger overlapped spinous processes. The lumbar spine has good flexion and extension and free lateral flexion because its disks are large, the spinous processes are posteriorly directed, and the facet joints are sagittally directed. Lateral lumbar rotation is limited because of facet alignment.
Sensory innervation
The sensory of intervertebral disks is complex and varies according to their location within the spinal column. In the cervical spine, studies by Bogduk [2] and Mendel [3] demonstrated the presence of both nerve fibers and mechanoreceptors within the anulus fibrosus. Impulses from these structures are transmitted via the sinuvertebral nerves and branches of the vertebral nerves. Another study by Bogduk [4] found that the sensory innervation of the lumbar intervertebral disks, like that of the cervical disks, is derived from the sinuvertebral nerves but also from branches of the ventral primary rami and rami communicantes.
Pathophysiology
Of all connective tissues, the intervertebral disk undergoes the most serious age-related changes. By the third decade of life, the nucleus pulposus (NP) becomes replaced with fibrocartilage, and the distinction between the nucleus and the anulus becomes blurred. The proteoglycan, water, and noncollagenous protein concentrations decrease, while the collagen concentration increases. The increase in collagen concentration is more pronounced in the nucleus and in the posterior quadrants of the disk. It is more pronounced with age and moves caudally in the lumbar spine (similar to the Wolff law).
Biochemically, aging increases the ratio of keratin sulfate to chondroitin sulfate, and it also changes the proportion of chondroitin-4-sulfate to chondroitin-6-sulfate, with a parallel decrease in water content. Proteoglycan synthesis decreases, which decreases the osmotic swelling and the traffic of oxygen and nutrients to the disk. Because of this decreased traffic, breakdown products of link and noncollagenous proteins stagnate in the disk. Nonenzymatic glycosylation of these breakdown products accounts for the brown discoloration of the aging connective tissues.
Differentiating aging from degeneration is difficult. According to Pearce et al, "[a]ging and degeneration may represent successive stages within a single process that occurs in all individuals but at markedly different rates." [5] Aging and degeneration have in common decreased water and proteoglycan content in the disks, combined with increased collagen.
This loss of proteoglycan content is one step in the positive feedback loop of disk degeneration. Proteoglycans inhibit endothelial cell proliferation. Loss of proteoglycans leads to increased angiogenesis and nerve ingrowth. The increased vascularity then decreases the proteoglycan content further. Increased sensory nerve density has been observed in the vertebral end plates of spines with DDD. The nerve ingrowth associated with this cascade may itself contribute to the pain associated with DDD. [6]
Whereas sagittal alignment, facet joint arthritis, and genetics potentially play a role in intervertebral disk degeneration, the results of one study suggested that the rate of degeneration may be associated with age. Those of African ethnicity also showed a faster rate of degeneration when compared with Whites; sex did not show a significant effect on degeneration. [7]
One study demonstrated that the presence of juvenile disk degeneration was strongly associated with overweight and obesity, low back pain, increased low back pain intensity, and diminished physical and social functioning. An elevated body mass index (BMI) was significantly associated with increased severity of disk degeneration. [8]
Another study found metabolic syndrome to be four times more prevalent in patients with radiographic evidence of severe DDD as defined by degenerative spondylolisthesis or cervical or lumbar stenosis causing neurologic symptoms [9] .
It has been theorized that there is an infectious component to the degenerative cascade. Evidence from multiple in-vitro, animal, and observational studies has suggested that bacterial infection is often present in the degenerated disk and that intradiskal injection of bacteria can lead to Modic changes in animal models. Albert et al studied this in human subjects with type 1 Modic changes on magnetic resonance imaging (MRI) and 6 months of low back pain refractory to conservative interventions. Subjects were divided into two groups: a control group and a group receiving amoxicillin-clavulanate. Patients who received antibiotics had less pain and reduced Modic changes on MRI. [10]
Prognosis
Low back pain due to a lumbar disk herniation is often treated successfully by means of conservative measures. There are four main types of disk herniation, as follows:
-
Bulging
-
Protrusion
-
Extrusion
-
Sequestration
With bulging, the posterior longitudinal ligament (PLL) remains intact. Disk protrusion may extend posteriorly to the PLL, but the anulus fibrosus will remain intact. With disk extrusion, the anulus fibrosus is compromised, allowing the NP to be exposed to the epidural space. With disk sequestration, NP material is separated from the main body of the disk.
A systematic review concluded that 62-66% of lumbar disk herniations are reabsorbed with conservative treatment. [11] There is evidence that the largest disk herniations (ie, extrusions and sequestrations) are the ones most likely to undergo reabsorption. Yu et al found that only 22% of patients who had extruded or sequestered lumbar disk herniation with radicular symptoms eventually went to surgery. [12] They found that conservative treatment and close monitoring for neurologic compromise frequently sufficed.
-
Magnetic resonance image of the lumbar spine. This image demonstrates a herniated nucleus pulposus at multiple levels.
-
Diskogram showing examples of an intact disk and a disrupted disk at the lumbar level.
-
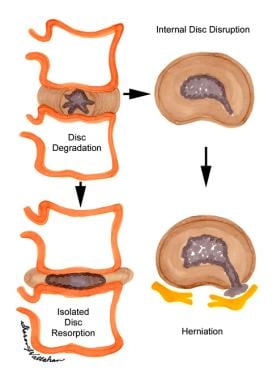
The process of disk degeneration following internal disk disruption and herniation.
-
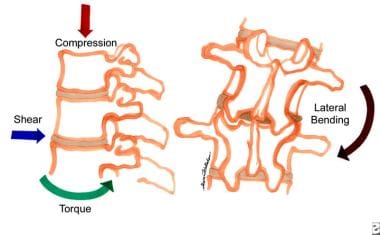
The various forces placed on the disks of the lumbar spine that can result in degenerative changes.