Practice Essentials
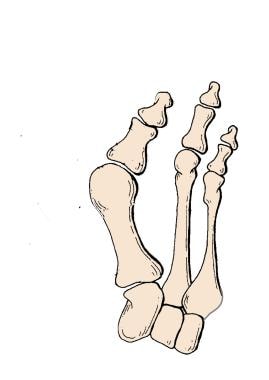
Hallux valgus (HV), with its accompanying bunion, is a common deformity of the forefoot involving the first ray, with first-phalanx abduction and pronation, as well as first-metatarsal (MT) adduction, pronation, and elevation, along with capsular and ligamentous derangement. [1] (See the image below.)
A directed history should be taken and physical examination performed to address vascular status, possible neuropathies, and medical comorbidities. Patients should be examined standing because this position often increases the HV and associated deformities.
A standing foot radiograph in the anteroposterior (AP) and lateral planes is mandatory in determining the type of surgery needed for bunion correction. In additional, an oblique nonstanding film can be obtained to gain a different perspective of the MT head and hindfoot. A sesamoid view, though seldom necessary, also should be obtained if a special problem with the sesamoids appears to be present. This information is then combined with the clinical picture to help determine the optimal surgical approach.
Understanding and characterizing each component of the deformity are the keys to treating it successfully. (See Treatment.) Many treatments have been proposed; the best choices are those that directly address the location of the deformity. Nonoperative treatment should be the initial option discussed. If footwear modifications fail to relieve the pain that comes with the deformity, surgical correction may be offered to the patient.
Successful treatment requires careful definition of the deformity, with appropriate consideration of its three-dimensional (3D) nature. Failure to accomplish such definition is probably the most common reason for recurrence and suboptimal results. If the deformity is not carefully defined, the surgical procedure chosen may not address all of its components.
For patient education resources, see the Foot, Ankle, Knee, and Hip Center, as well as Chronic Pain.
Anatomy
Deformities encountered in HV surgery involve the first metatarsophalangeal (MTP) joint. However, when assessing this deformity, one must also analyze the interphalangeal (IP) joint, the first metatarsocuneiform (MTC) joint, the hindfoot, and the ankle. The deformity may involve all of these levels, and such involvement can affect the success of a chosen operation. [2]
Early in the disease, the medial supporting structures of the first MTP joint (ie, the medial collateral ligaments and medial sesamoid) are typically the first structures to fail. Several other parts of the anatomy begin to fail as well. Once the medial supporting structures fail, the MT head can move medially, off the sesamoid apparatus, and the proximal phalanx (PP) falls into a valgus position. The PP remains attached by the deep transverse ligament and the adductor hallucis tendon.
Once the MT head has moved laterally over the sesamoid complex, the medial sesamoid can erode the crista and plantar-facing cartilage. The bursa over the medial aspect of the joint can thicken secondary to the increased pressure, worsening the condition. The extensor hallucis longus (EHL) and flexor hallucis longus (FHL) tendons are now in position to worsen the HV as they “bowstring” across the joint. The abductor hallucis attachments on the medial and plantar surface change position as the hallux pronates, and the force of the abductor hallucis then contributes to the pronation. [3]
First metatarsophalangeal joint
The first MTP joint receives the most attention in HV surgery. [4] It is a complex joint consisting of the PP, the first MT head, and the medial and lateral sesamoids. The variations in the bony anatomy and the soft tissues that cross this joint determine the stability of the joint and its tendency to deform into a valgus alignment. [2]
The rounded head of the first MT articulates with the concave base of the PP. The shape of the MT head plays a large role in the tendency to produce a valgus deformity. A more rounded first MT head is unstable and therefore more subject to deformity when acted on by external forces, such as narrow-toed shoes. This is compounded when combined with other commonly associated deformities of the foot, such as pes planus, hindfoot valgus, and congenitally tight heel cord. Flatter MT heads are more stable and less likely to contribute to HV.
Distal metatarsal articular angle
The second characteristic that contributes to HV is the orientation of the articular surface of the MT head in relation to the long axis of the first MT (see the image below). The distal metatarsal articular angle (DMAA) describes the lateral slope of the articular surface in relation to the long axis of the first MT. Normally, the DMAA is less than 10°. Surgical decision-making must take into account an increased DMAA.
Proximal phalanx articular angle
The orientation of the great toe is also determined by the proximal phalanx articular angle (PPAA). This is the angle formed by the intersection of a line along the long axis of the PP and a line along the proximal joint surface of the PP (see the image below). Deformity at this level contributes to an increased valgus deformity of the first toe; however, the deformity is expressed at the IP joint rather than the MTP joint.
The importance of the DMAA and PPAA cannot be overstated, because these angles reflect the lateral inclination of the joint. Correction of these angles must be a goal of any surgery chosen to address the bunion deformity.
Metatarsophalangeal joint congruence
MTP joint congruence is another factor that is considered in choosing a procedure for bunion correction. The congruence of the joint is determined by combining the PPAA and the DMAA. The lines drawn parallel to the joint surface of both the PP and the first MT head should be parallel (see the image below).
When the lines are parallel, a congruent joint exists; when they are not, an incongruous or subluxed joint exists. This relation is important to consider in choosing the surgical procedure. Intra-articular procedures (eg, distal soft-tissue realignment [DSTR]) should not be used with a congruent joint that has an increased DMAA, an increased PPAA, or both.
Congruent joints with an increased DMAA must be addressed with extra-articular procedures (ie, osteotomies) in order to prevent converting a congruent joint to an incongruent one. An incongruent joint, because of the unusual stresses on it, would be more prone to develop osteoarthritic changes.
Hallux valgus and intermetatarsal angles
The two angles most commonly used to describe the HV deformity are the HV angle (HVA) and the angle formed by the first and second MTs (1-2 intermetatarsal angle [IMA]) (see the image below).
The HVA is formed by the intersection of the lines along the long axis of the PP and the first MT. This angle is measured easily. Normally, it should be less than 15°. The next important measurement is the angle formed by the intersecting long axis lines along the first and second MTs. Normally, this angle should be less than 9°.
Metatarsocuneiform joint
The final joint that must be assessed carefully is the MTC joint. The shape and orientation of this joint vary and affect the medial inclination for the first MT. Reliable radiographic measurements of this joint are difficult to obtain, because these measurements can vary depending on the plane of the radiographic beam.
Excessive obliquity is associated with hypermobility instability of the first MTC joint. Hypermobility of the first MT as it moves through its oblique axis from dorsomedial to plantar lateral is believed to contribute to the deformity and is accentuated by the obliquity of the joint.
Excessive medial obliquity is associated with instability. In an in-vitro biomechanical study, Khaw et al [5] were able to demonstrate that whereas the first intermetatarsal ligament is important in stabilizing the first MT in all directions, the plantar aponeurosis is a secondary stabilizer that resists medial and dorsal rotation of the first MT after the first intermetatarsal ligament is divided. It is important to recognize that both the first intermetatarsal ligament and the plantar aponeurosis stabilize the first MT head.
Sesamoids
The final bony anatomic considerations involve the sesamoids. The sesamoids are located in the flexor hallucis brevis (FHB) tendon and lie under the first MT head. They have an important function for weightbearing and improve the biomechanical axis of the FHB action.
The plantar aspect of the first MT head has a longitudinal intersesamoid ridge in its center, termed the crista. The sesamoids lie on either side of this ridge as they articulate with the plantar surface of the first MT head. Normally, they should be centered under the first MT head on the standing anteroposterior (AP) radiograph of the foot. As the great toe develops a valgus deformity, the first MT head deviates medially, and rotation occurs at the MTP joint. The great toe pronates, the intrinsic musculature rotates laterally, and the first MT head displaces medially, subluxing off the sesamoids.
Normally, the sesamoids should be centered under the first MT head, and corrective procedures that restore this relation should be chosen.
Other considerations
Other considerations in assessing the deformity include associated pes planus deformity, pronation of the great toe, and Achilles tendon (AT) contraction. The AT has a dynamic effect on ambulation. A contracted AT compromises the ability to dorsiflex the foot. During gait, the result is external rotation, with increased demands placed on the medial structures of the forefoot. HV deformity is believed to be a result of this repetitive stress. A contracted AT can be idiopathic or can result from neuromuscular disease. Which of these it derives from should be noted during the physical examination because the presence of contracted AT, if not addressed, can contribute to recurrence of deformity.
In addition to the bony anatomy of the deformity, the soft-tissue envelope at the first MTP joint plays a role in the HV deformity. Because the first MT head has no direct muscle attachments, its position is influenced greatly by the alignment of the PP.
Essentially, four groups of muscles and tendons cross the first MTP joint and attach on the proximal aspect of the PP. The balance of these structures and the bony contour of the joint determine whether the PP stays aligned on the MT head. Dorsally, the EHL and the extensor hallucis brevis (EHB) insert centrally on the distal and proximal phalanges, respectively. They are kept in a central position by the hood ligaments, a fibrous band of tissue that is anchored to the collateral ligaments.
On the plantar surface, the FHL runs centrally between the sesamoids and inserts on the distal phalanx. The FHB has two tendon slips, which insert onto the medial and lateral sesamoids. The sesamoids then connect onto the PP through the plantar plate. Medially, the abductor hallucis tendon inserts onto the plantar medial PP and plantar medial joint capsule. The capsule becomes much thinner dorsally.
A similar relation exists on the lateral side of the joint, with the adductor hallucis tendon inserting onto the lateral sesamoid and plantar lateral joint capsule. The adductor hallucis has two muscle bellies, the transverse head and the oblique head. These come together in the conjoined tendon and insert on the lateral sesamoid. Comparatively, more muscle mass is present in the adductor hallucis when the muscle bellies are combined, creating a natural tendency to pull the PP into valgus.
These four groups of attachments create a delicate balance for keeping the PP centered on the first MT head. This balance is enhanced greatly when the first MT head is relatively flat. When the head is rounded, it is much easier for the PP to deviate. Once a deviation is created, the forces are quickly unbalanced.
The insertion of the adductor hallucis onto the lateral plantar base of the PP becomes the primary deforming force as the HV increases. Because its insertion is on the plantar half of the capsule and sesamoid, it tends to pronate the toe. As the rotation occurs, the abductor hallucis becomes more plantar and the only medial restraint left is the thin dorsal joint capsule, which readily becomes attenuated.
Once an angular deformity exists, the EHL and extensor digitorum brevis (EDB) are no longer centered on the PP and bowstring across the lateral side of the deformity, creating further imbalance. In considering the treatment of HV, one must address both the bony deformity and the soft-tissue balance, because both contribute to the pathologic condition.
Etiology
A connection has been found between shoes that are too narrow and forefoot complaints in women. [6] Risks for HV include the following [7] :
-
Female sex
-
Heel-wearing women
-
Overweight men
-
Men with pes planus
Obesity was found to be protective in women. [7] In addition, a longer first MT correlates with more severe HV in elderly persons. [8] Children who wear footwear of insufficient length have an increased rate of HV; the relative risk for an HVA angle of 4° or greater is 1.1171 if indoor shoes are one shoe size too short. [9]
Inheritable factors that may play a role in HV include the following:
-
Metatarsal formula
-
Arch height
-
Hypermobility
Additional evidence showed that 90% of 350 White patients with HV had at least one affected relative and that the most common associated inheritance pattern was autosomal dominant with incomplete penetrance. [10]
Epidemiology
In the United States, the number of forefoot operations for the three most common forefoot ailments (HV, hammertoe, and intermetatarsal perineural fibrosis) is markedly higher in females than in males. The prevalence of HV is markedly higher in females, with studies reporting a female-to-male ratio of 8-9:1 and even as high as 15:1. [11] This discrepancy is attributed to differences in footwear. [6]
With regard to age, the peak onset of HV is between the ages of 30 and 60 years, though it is likely that the initial changes occur during adolescence or even earlier in the case of juvenile HV. [12]
Prognosis
In a 2-year follow-up study evaluating the effect of three different types of HV surgeries, Thordarson et al [13] reported that patients who had HV surgery had significant improvements in four of their Short Form (SF)-36 scores, in four of five American Academy of Orthopaedic Surgeons (AAOS) lower-extremity scores, and in four of five American Orthopaedic Foot and Ankle Society (AOFAS) scores. The degree of deformity, amount of correction, and type of operation did not influence outcome.
When treatment addresses each component of the deformity, satisfactory results are possible. However, patients must have realistic expectations. Recurrent deformity, HV, and stiffness are the most common complications. Even with good corrections, some limitations still exist in 30% of patients.
-
Akin proximal phalanx closing-wedge osteotomy to correct high proximal phalangeal articular angle (PPAA).
-
Distal chevron metatarsal osteotomy fixed with Kirschner wire (K-wire).
-
Proximal chevron osteotomy fixed with two screws. Note Akin proximal phalanx osteotomy fixed with Kirschner wires (K-wires) and hammertoe correction held with K-wire.
-
Proximal chevron osteotomy fixed with two screws.
-
22-year-old woman with hypermobile first ray, first and second intermetatarsal angle (IMA) of 18°. Lapidus procedure preoperative image (left) and 6 months' postoperative image (right).
-
Proximal phalanx articular angle (PPAA; normal, <10°). This deformity is within proximal phalanx.
-
Distal metatarsal articular angle (DMAA; normal, <10°, average in normal feet, 7°).
-
Metatarsophalangeal joint congruence.
-
Intermetatarsal angle (IMA; normal, <9°).
-
Hallux valgus angle (HVA; normal, <15°).
-
Severe bunion deformity.
-
50-year-old woman with bilateral severe hallux valgus deformity.
-
Postoperative films after Lapidus procedures in 50-year-old woman with bilateral severe hallux valgus deformity.
-
Preoperative line diagram demonstrating hallux valgus. Courtesy of Rajul Gupta, MBBS, MS.
-
Minimally invasive surgery (MIS) distal metatarsal linear osteotomy. After medial displacement, the osteotomy has been fixed with a provisional K-wire. Courtesy of Rajul Gupta, MBBS, MS.
-
Fixation of osteotomy with beveled headless screws. Courtesy of Rajul Gupta, MBBS, MS.
-
Minimally invasive surgery (MIS) Akin osteotomy fixed with a single screw. Courtesy of Rajul Gupta, MBBS, MS.