Practice Essentials
Iliotibial band (ITB) friction syndrome (ITBFS) is a common cause of lateral knee pain, particularly among runners, military personnel, and cyclists. [1, 2, 3, 4] Biomechanical and training factors play a large role in the development of ITBFS, but its exact etiology is somewhat elusive. [5]
With the increasing understanding of human biokinetics, health professionals are able to spot flaws in training, environment, and biomechanics quickly and avert significant disability with ITBFS. Biomechanical screenings can be used to identify predisposing factors and correct them before symptoms ever develop. Aggressive intervention, particularly with athletes and industrial workers, can resolve the problem before it becomes disabling.
Most persons with ITBFS are treated by means of conservative therapy. When conservative therapy does not resolve the pain, surgery may be indicated. Conservative therapy should be employed for 3 months before surgery, but most patients for whom surgery is necessary have had symptoms for more than 9 months.
Surgery is rarely indicated. When surgical treatment is called for, the most common procedure for ITBFS is resection of the posterior portion of the ITB and, if desired, the adventitial bursa deep to the band. Surgery is performed with the knee held in 30° of flexion and consists of a limited resection of a small triangular or elliptical piece of the posterior part of the ITB covering the lateral femoral epicondyle. The bursa may be removed in certain cases as well. Arthroscopic techniques are being employed more frequently.
For patient education resources, see the Osteoporosis Center, as well as Knee Pain and Knee Injury.
Anatomy
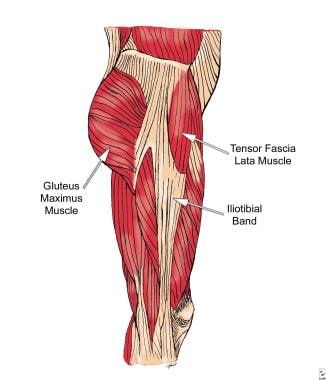
The ITB originates from the outer lip of the anterior iliac crest, the anterior border of the ilium, and the outer surface of the anterior superior iliac spine. The tensor fasciae latae (TFL) originates here also, and its fascia blends with the ITB at the lateroanterior thigh one third of the way distally. (See the image below.)
The intermuscular septum connects the ITB to the linea aspera femoris until inserting just proximal to the lateral femoral condyle. From there, it passes in its broad expansion between the lateral aspect of the patella and the biceps femoris to insert into the Gerdy tubercle, off the lateral tibial plateau. This expanse helps the lateral collateral ligament and posterolateral capsule to stabilize the knee.
The primary synergistic muscles are the hip abductors. These muscles are the gluteus medius, the gluteus minimus, and the upper fibers of the gluteus maximus. Their nerve supply comes from the superior gluteal nerve, which is a branch off of the L4, L5, and S1 nerve roots. [6]
Pathophysiology
ITBFS typically is observed in people who exercise vigorously. The overuse creates stress that the body cannot repair, and soft-tissue breakdown occurs. When the knee flexes, the ITB moves posteriorly along the lateral femoral epicondyle. Contact against the condyle is highest between 20° and 30° (average, 21°); thus, when the band is excessively tight or stressed, the ITB rubs more vigorously.
A small recess is formed between the lateral femoral epicondyle and the ITB as it travels along the lateral thigh to the tibial plateau. This space was believed to have a separate bursa lying deep to the band, but studies revealed it to be synovium that is a lateral extension and invagination of the actual knee joint capsule (lateral synovial recess [LSR]). The LSR lies underneath the ITB and acts as an interface between the ITB and the lateral femoral epicondyle.
Histologic analysis demonstrates inflammation and hyperplasia in the synovium, whereas magnetic resonance imaging (MRI) studies have demonstrated diffuse signal abnormality below the band and in the synovium but not in the ITB. This suggests that this syndrome is not a tendinopathy. Variance is observed in the congenital thickness of the band; patients with thicker bands may be predisposed to ITBFS.
In runners, friction occurs near or just after foot strike during the contact phase of the gait cycle. Downhill running reduces the knee flexion angle and can aggravate ITBFS, whereas sprinting and fast running increase the knee flexion angle and are less likely to cause the syndrome. [4, 7, 8] The friction point at the lateral epicondyle prominence is illustrated in the image below.
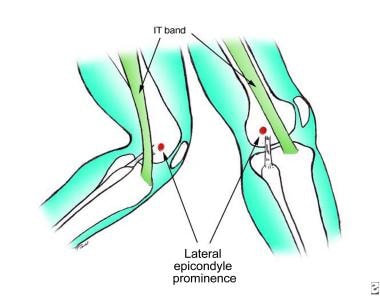 Illustration of the friction point at the lateral epicondyle prominence. Note the shift in position of the iliotibial band from anterior to posterior as the knee moves into flexion, drawing the iliotibial band across the prominence.
Illustration of the friction point at the lateral epicondyle prominence. Note the shift in position of the iliotibial band from anterior to posterior as the knee moves into flexion, drawing the iliotibial band across the prominence.
An alternative explanation advocated by some deemphasizes friction as a cause and postulates that excessive tension in the ITB leads to compression and inflammation of the underlying structures. [9, 10]
Etiology
The etiology of ITBFS is multifactorial. Many causative factors have been postulated, few with overwhelming evidence supporting them.
ITBFS usually is caused by overuse, which is mostly due to errors in training. Single-session errors cause ITBFS as often as repetitive deficiencies. Sudden changes in surface (ie, from soft to hard or from flat to uneven or a decline), speed, distance, shoes, and frequency can break down the body faster than it can heal, causing injury. Other factors frequently reported are the following:
-
Limb-length discrepancy
-
Genu varum
-
Overpronation
-
Hip abductor weakness
-
Myofascial restriction
Studies examining limb-length discrepancies have yielded conflicting conclusions regarding whether a direct correlation exists. Some noted that limb-length inequalities cause changes in hip abduction during the gait cycle, sacral leveling, and pelvic tilt, which is believed to increase tension on the ITB and the TFL. However, other studies did not find a direct correlation between limb-length inequality and ITBFS. Still, the postulate merits consideration in examination of the hip and pelvis. [11, 12]
However, most limb-length discrepancies are not actual anatomic variations but physiologic changes related to malalignment of the pelvis. For example, a superior shear of the left or right innominate (ilium) in relation to the sacrum would cause the leg on the ipsilateral side to migrate in the superior direction as well, thus creating a shorter leg in comparison to the right. Attempts to correct this difference with a heel lift would only reinforce the dysfunction in the pelvis.
Genu varum is considered a risk factor because of increased tension on the ITB as it is stretched more over the lateral femoral epicondyle. This concept is widely accepted, though with little empiric support.
Overpronation is controversial as well. In the running cycle, the lower limb strikes the ground with a rigid supinated foot. As the leg moves forward, the tibia internally rotates over the planted foot, "unlocking" it into a pronated-everted position, which allows for weightbearing. Pronation and internal rotation stress the ITB. Excessive pronation causes quicker tibial internal rotation and increased hip adduction, stressing the ITB over the lateral femoral condyle.
James implicated a combination of genu varum, heel varus, forefoot supination, and compensatory pronation in the development of ITBFS, but further videography studies led to dispute of that claim. Most studies have supported overpronation as a potential cause. [8]
Hip abductor weakness is an important factor as well. [13, 14] When the foot strikes the ground, the femur adducts against the eccentric load of the abductors (gluteus medius and TFL). These muscles move from eccentric to concentric through the support phase and into the propulsive phase of gait. The gluteus medius also externally rotates the hip, while the TFL internally rotates.
When the hip abductors are weakened or fatigued, runners have increased adduction and internal rotation at midstance. This generates more valgus force at the knee, which Fredericson postulated as increasing tension and friction on the ITB. [13, 15] Hip abductor weakness is often seen with core instability or malalignment and greater trochanteric bursitis. [16]
Myofascial restrictions and inflexibility can increase stress in the posterior ITB, particularly with the TFL. Tightness in the hip flexors (iliopsoas), extensors (gluteal muscles), and rotators (particularly piriformis) can shift more load to the abductors and adductors. Weaker hip abductors eventually fail under continuous stress.
A matched case-control study by Everhart et al suggested a relation between greater lateral epicondyle prominence and ITBFS. [17]
In rare instances, ITBFS can be related to surgical changes to the knee from other pathology, such as anterior cruciate ligament tears. [18] Cases of ITBFS after total knee arthroplasty (TKA) have been reported. [19]
Epidemiology
The overall incidence of ITBFS in the general population has not been well reported. Depending on which population is examined, the incidence has been in the range of 1.6-52%, varying with the target population's type and intensity of activity.
For instance, Linenger et al reported that in 12 weeks of US Marine Corps basic training, ITBFS was the most common specific injury and accounted for 22.2% of all lower-extremity injuries. [20] Runners experience 12% of all running-related overuse injuries from ITBFS. In a Central European study of running-related injuries (N = 178), ITBFS accounted for 12.3% of the injuries. [21]
Prognosis
Most patients with ITBFS recover with conservative therapy and enjoy good prognoses. Those for whom surgery is eventually performed typically are patients who are motivated to return to a specific activity in which ITBFS limits or prohibits their participation.
Individuals with ITBFS who require surgery often do well. Surgical release of the ITB is typically successful in eliminating pain. Athletes are able to return to their normal activities with a rehabilitation program in 3-7 weeks. Nemeth et al described 17 cases of ITBFS recalcitrant to conservative therapy, of whom 11 had excellent results from surgical treatment at 2-year follow-up. [22] Firer reported 94% excellent or good results in 64 runners surgically treated after failure of conservative therapy. [23]
-
Illustration of the friction point at the lateral epicondyle prominence. Note the shift in position of the iliotibial band from anterior to posterior as the knee moves into flexion, drawing the iliotibial band across the prominence.
-
Lateral hip stabilizers.
-
Iliotibial band noted prominently along the lateral thigh.
-
Iliotibial band at the lateral femoral epicondyle, with the posterior fibers denoted.
-
The Thomas test can be used to evaluate restriction in the iliotibial band, hip flexors, and rectus femoris.
-
Resection of lateral synovial fold through arthroscopic knee procedure. Courtesy of Elsevier, Inc (Cowden CH 3rd, Barber FA. Arthroscopic treatment of iliotibial band syndrome. Arthrosc Tech. Feb 2014;3(1):e57-60).