Practice Essentials
Coccygodynia (also referred to as coccydynia, coccalgia, coccygalgia, or coccygeal pain) is a painful syndrome affecting the tailbone (coccygeal) region. [1, 2] The word coccyx is derived from the Greek word kokkyx ("cuckoo"), on the basis of this structure’s resemblance to the shape of a cuckoo’s beak (see the image below).
Coccygodynia is a rare condition but can be highly unpleasant when it does occur. Patients' chief complaint is pain, which typically is triggered by or occurs while sitting on hard surfaces. The pain often varies and sometimes is aggravated by arising from the sitting position.
For most patients with coccygodynia, conservative therapy (eg, massage, injection, and ganglion impar block) appears to play a vital role in management. [3] For those with intractable pain that does not respond to conservative therapy, coccygectomy is typically effective. However, optimal specific therapy for each specific type of coccyx in coccygodynia is still a matter of debate, and no final consensus has yet been reached.
For patient education resources, see Tailbone (Coccyx) Injury and Low Back Pain.
Pathophysiology
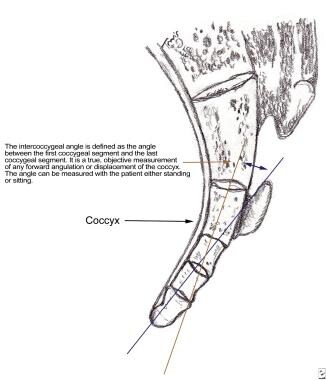
The coccyx consists of three to five rudimentary vertebral units that are fused, except for the first coccygeal segment, which in turn articulates with the sacral cornu of the inferior sacral apex at S5 (see the image below). The sacrococcygeal articulation is either a symphysis or a true synovial joint.
Postacchini and Massobrio [4] classified coccygeal configurations into four types (see the image below).
 Coccygeal configuration types I, II, III, and IV (from left to right). Type I: Coccyx is curved slightly forward, with its apex directed downward and caudally. Type II: Forward curvature is more marked, and apex extends straight forward. Type III: Coccyx most sharply angulates forward. Type IV: Coccyx is subluxated at sacrococcygeal joint or at intercoccygeal joint.
Coccygeal configuration types I, II, III, and IV (from left to right). Type I: Coccyx is curved slightly forward, with its apex directed downward and caudally. Type II: Forward curvature is more marked, and apex extends straight forward. Type III: Coccyx most sharply angulates forward. Type IV: Coccyx is subluxated at sacrococcygeal joint or at intercoccygeal joint.
The majority of cases of coccygodynia occur in conjunction with either a subluxated or a hypermobile coccyx (often referred to as a culprit lesion). It has been proposed that the pathologic instability may give rise to chronic inflammatory changes and pain. [5] However, the study by Postacchini and Massobrio showed that there was no statistical difference between asymptomatic patients and those with coccygodynia in terms of the numbers of coccygeal segments or the incidence of fusions between the segments. [4]
Etiology
Several possible causes of coccygodynia have been described. The most common of these is a single axial trauma, such as occurs with a fall directly onto the coccyx or during childbirth. However, Maigne et al suggested that only a traumatic event that occurs within 1 month of onset is significant in increasing the risk of instability and subsequent coccygodynia. [6]
Obesity is another possible cause of coccygodynia. A body mass index (BMI) higher than 27.4 in women or 29.4 in men is a risk factor for the development of both idiopathic and posttraumatic coccygodynia. [6] As high-BMI individuals attempt to sit down, the coccyx tends to jut out posteriorly as a result of inadequate sagittal pelvic rotation. This results in increased exposure to the intrapelvic pressure that occurs with sitting, ultimately causing subluxation of the coccyx.
The coccygeal configuration (see Pathophysiology) also appears to influence the cause of pain. Types II, III, and IV are more painful than type I. [4]
Coccygodynia may also occur in individuals with a normal coccyx. In such cases, the pain may derive from secondary causes, such as tumor, infection, bursitis, or posttraumatic arthritis.
Epidemiology
Coccygodynia accounts for fewer than 1% of all back pain conditions. [7, 8, 9] It is five times more prevalent in women than in men, [10] presumably because the bone is more prominent in women than in men. [11] Although coccygodynia can occur over a wide age range, the mean age of onset is around 40 years. [10]
Prognosis
Several studies have reported good-to-excellent outcomes in patients undergoing coccygectomy. [12, 13, 14]
In an analytic review of 671 patients with coccygodynia who underwent coccygectomy for failed conservative management, Karadimas et al found that the procedure provided pain relief in as many as 85% of cases. [15] The overall complication rate was 11%, including superficial as well as deep infections, delayed wound healing, infection, hematoma, and wound dehiscence.
In a study evaluating the results of 26 coccygectomies at a median follow-up of 37 months (range, 2-133 mo), Kerr et al reported excellent clinical results in 13 patients, good results in nine, fair results in two, and poor results in two. [16] The overall favorable outcome rate was 84.6%, with a complication rate of 11.5% (mainly attributable to infection).
Ramieri et al reported the results of 28 consecutive coccygectomies for acute traumatic instability of the coccyx, of which 21 were total and seven were partial. [17] Of the 25 patients assessed at a mean follow-up of 33 months, 19 experienced complete pain relief, two experienced incomplete relief, and four experienced no relief. Partial coccygectomies were associated with poor results.
A single-institution retrospective study by Mulpuri et al (N = 173; 77% women; mean age, 46.56 y; mean follow-up, 5.58 y) evaluated outcomes of coccygectomy for coccygodynia, comparing values for the preoperative and postoperative Oswestry Disability Index (ODI), visual analogue scale (VAS), Patient-Reported Outcomes Measurement Information System-29 (PROMIS-29), and EuroQol-5D (EQ-5D). [18] ODI, VAS, and several PROMIS-29 domains improved postoperatively. Older age predicted continued postoperative disability; prior spine surgery, trauma etiology, and female sex predicted inferior outcomes. No outcome differences were demonstrated among coccyx morphologies.
-
Coccyx is usually formed of 3-5 rudimentary vertebrae.
-
Coccyx as compared with cuckoo's beak.
-
Coccygeal configuration types I, II, III, and IV (from left to right). Type I: Coccyx is curved slightly forward, with its apex directed downward and caudally. Type II: Forward curvature is more marked, and apex extends straight forward. Type III: Coccyx most sharply angulates forward. Type IV: Coccyx is subluxated at sacrococcygeal joint or at intercoccygeal joint.
-
Dynamic radiographs obtained from patient with coccygodynia.