Indications for Surgical Intervention
Distal tibiofibular ligament sprain with widened ankle mortise
One of the few absolute indications for surgery in patients with a high ankle sprain involving the distal tibiofibular ligament is a third-degree sprain that causes widening or a diastasis of the syndesmosis between the distal fibula and tibia. To restore the ankle mortise, the distal tibiofibular articulation must be brought together with implants, such as screws or synthetic sutures over endobuttons.
The usual postoperative course entails initial protection in a splint, wound check and further protection in a cast, and avoidance of weightbearing for 6 weeks, followed by physical therapy and gradual return to normal activities.
Lateral ankle ligament sprains
It is generally accepted that for most patients, operative repair of third-degree anterior talofibular ligament (ATFL) tears and medial ankle ligament tears does not contribute to an improved outcome. [1]
In 100 patients with isolated lateral ligament sprains, Evans et al found no functional or symptomatic advantage 2 years after injury in patients who were treated surgically as compared with those who were treated with cast immobilization. [2] In fact, the nonsurgically treated group returned to work earlier and had less morbidity than the surgically treated patients. Patients in this study were divided into two groups, each with 30 individuals with anterior ligament sprains only and 20 individuals with anterior and middle ligament ruptures. One group of 50 patients was treated surgically, and the other group was treated with cast immobilization.
Double lateral ligament tears
Staples reported that young, active, athletic patients with tears of both the ATFL and the calcaneofibular ligament (CFL) are best treated surgically. His cohorts included a group of young athletic patients with only 58% satisfactory results after immobilization and a subsequent, similar group of patients who had 88.9% satisfactory results with surgical repair. In the group of patients who underwent surgery, the average hospital stay was 7.6 days, and six (22.2%) of 27 patients had complications. Marginal necrosis of the skin at the wound edge and hypesthesia of the fourth and fifth toes and adjacent forepart of the foot were the only reported complications. [3]
Entrapped deltoid ligament
An isolated complete medial ankle sprain with a palpable defect and demonstrable clinical instability is an indication for surgery, particularly if the deltoid ligament is caught in the medial ankle joint. Surgery allows removal of the ligament from the joint and repair of the ligament.
Go to Ankle Sprain for more complete information on this topic.
Surgery for Chronic Ankle Instability
Selection of operative approach
According to a review by Safran et al, more than 20 different delayed surgical procedures are available for chronic ankle instability and sprains. [4] These are classified as either anatomic or nonanatomic. Anatomic repairs use the native tissues, reinforce the existing ligaments, or both. Most of the nonanatomic repair procedures are reconstructive in nature and involve tenodesis between the lateral malleolus and calcaneus, talar head, or fifth metatarsal.
Some of these procedures use the peroneus brevis or longus as autograft and are routed through bone tunnels to provide lateral ankle stability. Use of the local tendons in a nonanatomic manner affects the normal biomechanics of the hindfoot in addition to donor tendon morbidity due to the loss of function from tendon that is sacrificed. If the tissues are of good quality, a direct repair of the ligaments can be performed; if the tissues are of poor quality, autograft or allograft tendons are used.
For syndesmotic sprains, surgical treatment depends on whether any arthritic change is present. If the articular surface is destroyed on both sides of the joint, tibiotalar arthrodesis or arthroplasty is necessary. In patients with diastasis without significant tibiotalar arthritis, late reduction of the syndesmosis and reconstruction of the ligaments are recommended. [5]
Broström procedure
Broström described a repair that reapproximates the ruptured ligaments and restores true normal anatomy of the ankle. Gould et al described a modified Broström procedure that allowed reinforcement of the repair and limited inversion (reducing the likelihood of injury) and that helped to correct the subtalar component to the instability. [6] This modified procedure permitted restoration of the normal anatomy and preserved normal ankle motion with less surgical exposure.
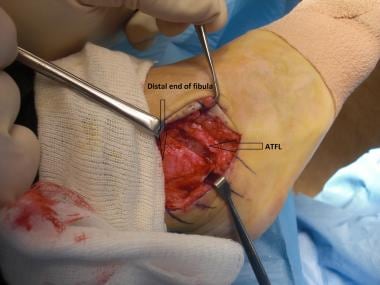
In Gould's modified procedure, the incision is performed from an anterolateral approach, paralleling the fibula border, and starting from the level of the plafond distally to the level of the peroneal tendons. Dissection is then carried down to the capsule. If no obvious ATFL rupture is present, the capsule and ligaments are divided for a few millimeters and then imbricated. [6, 7, 8] (See the images below.)
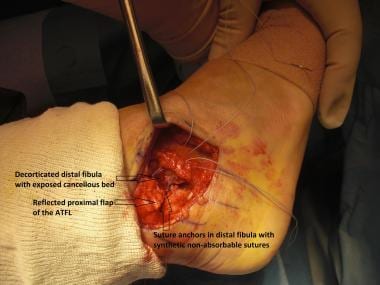 Brostrom-Gould repair. Reflected proximal flap of anterior talofibular ligament (ATFL), cancellous bed at distal end of fibula, and sutures coming out distal flap from embedded suture anchors to help advance distal flap of transected ATFL.
Brostrom-Gould repair. Reflected proximal flap of anterior talofibular ligament (ATFL), cancellous bed at distal end of fibula, and sutures coming out distal flap from embedded suture anchors to help advance distal flap of transected ATFL.
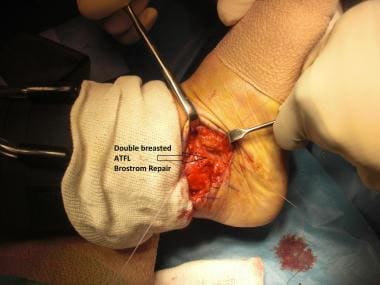 Brostrom-Gould repair. Double-breasted anterior talofibular ligament (ATFL) with proximal flap overlying distal flap.
Brostrom-Gould repair. Double-breasted anterior talofibular ligament (ATFL) with proximal flap overlying distal flap.
 Brostrom-Gould repair. Incorporation of extensor retinaculum in suture for advancement of retinaculum over repaired anterior talofibular ligament (ATFL).
Brostrom-Gould repair. Incorporation of extensor retinaculum in suture for advancement of retinaculum over repaired anterior talofibular ligament (ATFL).
The peroneal sheath is then opened to determine the quality of the CFL. If the CFL is stretched, it can be divided and imbricated. [6] If this ligament is ruptured, a distal avulsion from the calcaneus can be reattached with a suture anchor. A proximal avulsion can be reattached with sutures through drill holes in the fibula. [6]
Attenuation or failure of previously repaired ligaments in case of recurrent laxity necessitates augmentation with auto- or allograft, in that the local tissue is frequently of insufficient quality. Furthermore, failed surgical repair may be associated with previous surgical scars and compromised local skin and subcutaneous tissues.
Lateral ankle ligament repair is depicted in a video created by the author.
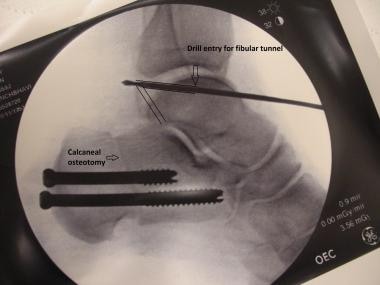
Minimally invasive reconstruction of lateral ankle ligaments is an attractive option that avoids long exposures and scars and minimizes the risks of wound or flap failure, especially in patients with previous scars or poor soft tissues. In 2011, the author published a minimally invasive technique in which allograft was used to reconstruct lateral ankle ligaments in the presence of scarring or revision surgery where the ligament tissue quality was poor. [9] (See the images below.)
 Minimally invasive allograft reconstruction of lateral ankle ligament. View post calcaneal osteotomy showing patient positioning and scar from previous failed lateral ankle ligament repair.
Minimally invasive allograft reconstruction of lateral ankle ligament. View post calcaneal osteotomy showing patient positioning and scar from previous failed lateral ankle ligament repair.
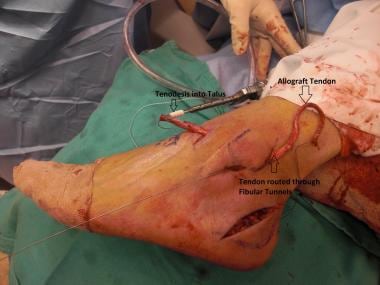 Minimally invasive allograft reconstruction of lateral ankle ligament. Percutaneous exposure for graft insertion using biotenodesis screw into talus and allograft routed distally.
Minimally invasive allograft reconstruction of lateral ankle ligament. Percutaneous exposure for graft insertion using biotenodesis screw into talus and allograft routed distally.
 Minimally invasive allograft reconstruction of lateral ankle ligament. Postoperative scars from percutaneous routing of allograft tendon.
Minimally invasive allograft reconstruction of lateral ankle ligament. Postoperative scars from percutaneous routing of allograft tendon.
An arthroscopic variant of the Broström procedure has been described. [10]
Suture tape augmentation and or augmentation with graft can be undertaken if the tissue at the time of repair is felt to be of insufficient quality.
After lateral ankle ligament repair, the need for immobilization to protect the surgical repair site must be balanced against the need for ankle joint mobilization to restore optimal postoperative ankle range of motion (ROM). The period of immobilization in a short leg cast or a boot ranges from 3 to 6 weeks.
A systematic review by Vopat et al compared early and delayed mobilization (EM, ≤ 3 wk post surgery; DM, > 3 wk) postoperative protocols in patients undergoing primary lateral ankle ligament repair. [11] A total of 28 studies met the criteria for the final analysis (N = 1457). The study followed PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) guidelines, and a meta-analysis using the PubMed/Ovid MEDLINE database was performed. Return to sport (RTS), outcome scores (American Orthopaedic Foot and Ankle Society [AOFAS] ankle-hindfoot scale and Karlsson score), radiographic outcomes (talar tilt and anterior drawer), and complications were recorded and statistically analyzed.
The postoperative AOFAS score was significantly greater in the EM group (98.8 vs 91.9), as was the postoperative Karlsson score (92.2 vs 90.0). [11] However, the EM group had significantly greater postoperative laxity on both the anterior drawer test (6.3 vs 3.9 mm) and the talar tilt test (5.1º vs 4.5º). Also, the DM group had significantly lower rates of overall complications (3.1% vs 11.4%) and skin wound complications (1.3% vs 3.8%). RTS was not significantly different between the two groups. Additional randomized studies are needed for definitive evaluation of early versus delayed rehabilitation protocol timetables to optimize functional outcomes without compromising long-term stability.
Tenodesis procedures
Other surgical options, as mentioned above, are mainly tenodesis procedures, of which the following four have been extensively used and described in the literature:
-
Evans procedure
-
Watson-Jones procedure
-
Larsen procedure
-
Chrisman-Snook procedure
These procedures focus on harvesting all or part of the peroneus brevis and then rerouting the tendon through various bone tunnels, thereby creating a tenodesis of the ankle or reconstructing the ATFL or the CFL. Indications for these augmented types of reconstruction are as follows:
-
The ATFL and CFL are so disrupted and frayed that they cannot be repaired primarily
-
Hypermobility of the subtalar joint is present
-
The patient has had previously unsuccessful reconstruction of the ankle
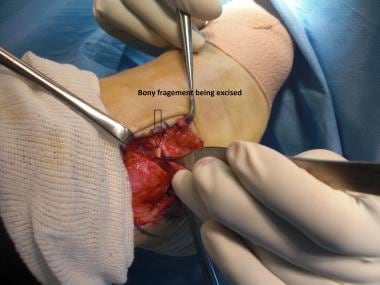
For each of these procedures, the overall technical approach is essentially the same. A longitudinal incision is made running just posterior to the prominence of the lateral malleolus. The incision is then extended to allow harvesting of the peroneus brevis tendon. Before harvesting the tendon, the joint is inspected and debrided if necessary. Occasionally, the ATFL, the CFL, or both are avulsed from the fibula with a piece of bone. This so-called os subfibulare should be excised.
The integrity of the superior peroneal retinaculum should be maintained during exposure of the peroneus brevis tendon. The anterior one third of the tendon is isolated distally and split from the distal position to the musculoskeletal junction. This tendon portion is transected at its proximal aspect. A drill hole is made through the distal fibula, and the split portion of the peroneus brevis is passed through this hole. The tendon is tensioned with the foot in mild plantarflexion and eversion.
Because the peroneus brevis tendon is anchored to the fibula, the Evans reconstruction indirectly limits inversion of the ankle and anterior talar translation while also limiting motion of the subtalar joint. This procedure provides stability in a location that lies between the ATFL and CFL; therefore, it does not restore the anatomy or biomechanics of the hindfoot.
The Watson-Jones procedure reconstructs the ATFL but not the CFL. This technique makes use of the Evans tenodesis. One important addition, however, is that the peroneus brevis graft is routed anteriorly through the talar neck to reconstruct the ATFL.
Larsen rerouted the peroneus brevis tendon from the fifth metatarsal base into the fibula and then back down into the calcaneus. The proximal part of the tendon is sutured to the peroneus longus. [12]
The Chrisman-Snook procedure, most commonly used for subtalar instability, involves using half of the longitudinally divided peroneus brevis tendon to substitute for or reconstruct the CFL. In this procedure, the peroneus brevis graft is brought through the fibula from anterior to posterior to reconstruct the ATFL. It is then brought posteriorly and inferiorly to the calcaneus in a weave pattern to reconstruct the CFL. This procedure, though technically demanding, has been repeatedly demonstrated to produce satisfactory stability in patients with talotibial and combined talotibial and talocalcaneal instability.
Outcomes of Operative Repair
Most of the nonanatomic procedures are now considered to be of historical interest only, having been superseded by anatomic repairs that use either native ligaments or allograft tendons.
In the literature, the Watson-Jones procedure was associated with subjective instability 20-90% of the time; the Evans procedure, 20-33%. In addition, with the Evans procedure, a persistent anterior drawer sign was found in 45-60% of patients. In the Chrisman-Snook procedure, 13-30% of patients had subjective persistent instability. Decreased inversion is common with all these procedures. In each procedure, a specific weave pattern (referring to the manner in which the peroneus brevis tendon is routed through the drill holes) is used.
In a study by Kim et al, chronic syndesmotic instability and chronic medial ankle instability were found to be significantly associated with unsatisfactory outcomes in patients with chronic ankle instability who had undergone treatment with a modified Broström procedure. [13]
Park et al, in a study of the use of the anterior half of the peroneus longus tendon (AHPLT) as an autograft for lateral ankle ligament reconstruction in 31 cases, reported good clinical and radiographic results at a minimum 1-year follow-up, without a significant decrease in peroneus longus strength. [14]
Matheny et al compared outcomes and revision rates after Broström-Gould lateral ankle ligament repair with those after anatomic allograft reconstruction in 86 patients with lateral ankle instability. [15] At an average follow-up of 3.0 years, no patient in either cohort underwent revision lateral ligament surgery. The authors concluded that anatomic allograft reconstruction, as compared with lateral ankle repair, produced similarly favorable outcomes, including high patient satisfaction, high function and activity levels, and no need for surgical revision.
Lee et al studied the effect of smoking on the outcomes of lateral ankle ligament reconstruction in 70 patients (23 smokers, 47 nonsmokers) with chronic ankle instability who were treated with anatomic reconstruction of the ATFL and the CFL using semitendinosus tendon allografts and biotenodesis screws. [16] Visual analog scale (VAS) pain scores, American Orthopedic Foot and Ankle Society (AOFAS) ankle-hindfoot scores, Karlsson scores, and complications were routinely determined at each follow-up visit. Anterior translation and the talar tilt angle on radiographic stress views were also assessed. The mean follow-up period was 21.8 months (range, 12-68).
No significant differences were observed between the two groups in this study with respect to age, gender, body mass index (BMI), or duration of preoperative symptoms. [16] Mean preoperative pain VAS scores were 5.8 in nonsmokers and 5.3 in smokers. Postoperatively, mean VAS scores improved to 1.4 in both groups. Although clinical and radiographic measures did not change significantly in the presence of smoking after surgery, two wound complications (one delayed healing and one superficial necrosis) occurred in nonsmokers, whereas five (two delayed healing, two superficial infections, and one superficial necrosis) occurred in smokers.
Araoye et al retrospectively reviewed 382 cases of lateral ankle ligament repair or reconstruction, assessing the prevalence of associated copathologies in chronic lateral ankle instability in an effort to determine whether the presence of these could predict outcome. [17] In the 99 cases selected for inclusion, copathologies included peroneal pathology (75/99 [75.8%]), ankle impingement (40/99 [40.4%]), and osteochondral lesion of the talus (17/99 [17.2%]); 36.4% (36/99) had a low-lying muscle belly of peroneus brevis.
The total reoperation rate in this study was 13.1%; it was lower in cases with peroneal pathology (8.7% vs 27.5%). [17] Peroneal pathology, ankle impingement, and osteochondral lesions were the most common associated copathologies in surgical patients with chronic lateral ankle ligament instability. The presence of peroneal pathology may lead to fewer reoperations, possibly as a result of a more comprehensive first-time surgical approach.
A systematic review and meta-analysis (N = 1920) by Vopat et al compared outcomes after primary repair (PR; n = 1486), graft reconstruction (GR; n = 350), and suture tape augmentation (STA; n = 84) in patients who underwent surgical intervention for chronic lateral instability with at least a 1-year follow-up. [18] The GR group appeared to have the lowest rate of complications, at 3.1%, compared with 4.2% for the PR group and 10.7% for the STA group.
Outcomes were excellent across all groups. [18] Postoperative AOFAS scores ranged from 89.0 to 95.1 for GR and from 90.0 to 98.8 for PR. Postoperative Karlsson scores were 80.9-94.4 for GR and 89.2-94.1 for PR. Anterior-drawer postoperative scores were 1.4-30.3 mm for GR, 2.7-8.6 mm for PR, and 4.1-4.2 mm for STA. Postoperative talar tilt was 2.4-7.3º for GR, 1.9-6.0º for PR, and 3.6-4.5º for STA. RTS was 9.5-20.4 weeks for PR; one study reported an RTS of 10.6 weeks for STA. Analysis suggested that there may be no difference in functional outcomes between PR and GR but that there may be a potential improvement with PR versus STA.
May et al conducted an analysis of return to play after a modified Broström lateral ankle ligament reconstruction procedure (MBP). [19] Patients who had undergone a primary MBP by a single surgeon over a 6-year period and had a minimum follow-up of 24 months of follow-up were contacted by telephone and asked about their ability to return to sport or work activity at final follow-up. Of the 59 patients who met the inclusion criteria, 41 (69%; 20 men, 21 women) participated in the telephone interview.
Of the 41 participants, 22 (54%) returned to their prior level of activity (returners). Mean age was 27.2 years for returners and 27.1 years for nonreturners. [19] Most patients (36/41; 88%) were satisfied with surgery and the overall outcome. Of the 19 nonreturners, 7 (37%) noted ankle-related reasons for not returning (pain, 57%; residual instability, 29%; decreased ROM, 14%), and 12 (63%) cited non-ankle-related reasons.
-
Brostrom-Gould repair. Instrument under anterior talofibular ligament (ATFL).
-
Brostrom-Gould repair. Transected anterior talofibular ligament (ATFL).
-
Brostrom-Gould repair. Avulsed fibular bony fragment.
-
Brostrom-Gould repair. Excision of avulsed fibular bony fragment.
-
Brostrom-Gould repair. Reflected proximal flap of anterior talofibular ligament (ATFL), cancellous bed at distal end of fibula, and sutures coming out distal flap from embedded suture anchors to help advance distal flap of transected ATFL.
-
Brostrom-Gould repair. Double-breasted anterior talofibular ligament (ATFL) with proximal flap overlying distal flap.
-
Brostrom-Gould repair. Incorporation of extensor retinaculum in suture for advancement of retinaculum over repaired anterior talofibular ligament (ATFL).
-
Minimally invasive allograft reconstruction of lateral ankle ligament. View post calcaneal osteotomy showing patient positioning and scar from previous failed lateral ankle ligament repair.
-
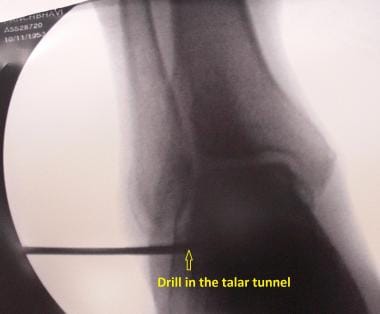
Minimally invasive allograft reconstruction of lateral ankle ligament. Percutaneous exposure for graft insertion using biotenodesis screw into talus and allograft routed distally.
-
Minimally invasive allograft reconstruction of lateral ankle ligament. Talar tunnel.
-
Minimally invasive allograft reconstruction of lateral ankle ligament. Fibular tunnel.
-
Minimally invasive allograft reconstruction of lateral ankle ligament. Postoperative scars from percutaneous routing of allograft tendon.