Practice Essentials
Ruptures of the quadriceps tendon are relatively infrequent and usually occur in patients older than 40 years. A strong association exists with numerous systemic diseases and prior degenerative changes in the knee extensor mechanism. Ruptures most often occur unilaterally. Bilateral ruptures are highly correlated with systemic disease but have been reported in healthy patients who do not have predisposing factors. [1, 2, 3, 4]
Patellar tendon ruptures are less common than quadriceps ruptures and tend to occur in patients younger than 40 years. In rare cases, partial ruptures of the quadriceps tendon are seen in young athletes with end-stage jumper's knee. [5, 6] Jumper's knee usually involves the patellar tendon, though in 25% of cases, the quadriceps is involved.
Complete quadriceps tendon rupture is a disabling injury, and operative repair is required. Lister, in 1878, was the first to report on surgical repair. In 1887, McBurney reported on the first surgical repair in the United States. The injury was a direct blow to the knee, and the tendon was repaired using catgut and silver wire. After several other reports on surgical repair of extensor mechanism injuries were published in the early 1900s, operative management became standard.
In 1949, Steiner and Palmer reported the first case of bilateral simultaneous ruptures of the quadriceps tendons. Since then, several large series of patients undergoing quadriceps tendon repair have been published. [7, 8, 9, 10, 11, 12] In the past few decades, many case reports of bilateral quadriceps ruptures have been published.
To obtain the best results, early diagnosis and treatment of quadriceps tendon ruptures are essential (see Presentation, Workup, and Treatment). [13] Particular care must be taken to educate all physicians on the importance of testing the integrity of the extensor mechanism in the injured knee; it is hoped that improved physician awareness will lead to fewer cases of misdiagnosis of extensor mechanism injuries. If intervention is delayed, repair is more difficult and results may be compromised.
Anatomy
The quadriceps muscle is composed of four muscle groups, as follows:
-
Vastus intermedius
-
Vastus medialis
-
Vastus lateralis
-
Rectus femoris
The quadriceps tendon is formed by the convergence of all four muscles just proximal to the superior patella. The tendon is multilayered. The rectus femoris becomes tendinous 3-5 cm proximal to the patella and is the most superficial layer inserting on to the patella. Some of its fibers continue over the anterior patellar surface and contribute distally to the patellar tendon. The middle layer is composed of the vastus lateralis and the vastus medialis.
The vastus medialis, which is composed of the vastus medialis obliquus and the vastus medialis longus, becomes tendinous only a few millimeters from its insertion into the patella. The vastus lateralis becomes tendinous about 3 cm proximal to its insertion into the patella. The deep layer is composed of the vastus intermedius. The tendon has an average thickness of 8 mm and an average width of 35 mm.
Peterson et al found that the blood supply to the quadriceps tendon arises from the descending branches of the lateral circumflex femoral artery, branches of the descending geniculate artery, and branches of the medial and lateral superior geniculate arteries. [14] The superficial layers are well vascularized. In the deep layer, however, there is an oval, avascular area that is 30 × 15 mm in size; this area probably plays a significant role in tendon degeneration.
Pathophysiology
Quadriceps tendon rupture usually occurs distally 0-2 cm from the superior pole of the patella, through pathologic tissue. Various systemic conditions may cause damage to the tendon vascular supply or may disrupt the tendon structure.
Diabetes can cause arteriosclerotic changes in tendon vessels. Fibrinoid necrosis of tendons is seen with chronic synovitis. Hyperparathyroidism causes dystrophic calcifications and subperiosteal bone resorption at the tendon insertion. Obesity causes fatty degenerative changes in tendons and increases the forces on the tendon. Fatty degeneration, fibrinoid degeneration, and decreased collagen are seen with normal aging.
Kannus and Jozsa examined histopathologic changes in 891 ruptured tendons; about 97% of the pathologic changes were degenerative. [15] The degenerative changes included hypoxic degenerative tendinopathy, mucoid degeneration, tendolipomatosis, and calcifying tendinopathy. In the 82 quadriceps tendons, tendolipomatosis was the most common type of degeneration, seen in almost half of the tendons (see the image below). No signs of inflammatory cells were noted in any of the specimens. In 62% of the ruptured tendons, pathologic changes of the tendon blood supply were seen, including vessel narrowing and thrombosis.
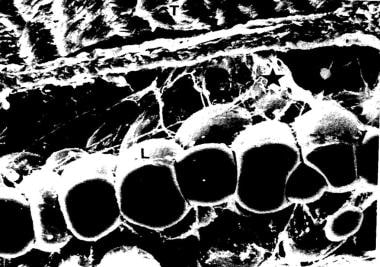 Tendolipomatosis. Reprinted with permission from Kannus P, Józsa L. Histopathological changes preceding spontaneous rupture of a tendon. A controlled study of 891 patients. J Bone Joint Surg Am. Dec 1991;73(10):1507-25.
Tendolipomatosis. Reprinted with permission from Kannus P, Józsa L. Histopathological changes preceding spontaneous rupture of a tendon. A controlled study of 891 patients. J Bone Joint Surg Am. Dec 1991;73(10):1507-25.
Trobisch et al retrospectively reviewed 45 quadriceps tendon ruptures in 42 patients and performed histologic analysis on a tissue sample from the rupture zone in 22 cases. [16] Only 14 (64%) of the 22 samples showed degenerative changes. The ratio of degenerative tendons to nondegenerative tendons rose with increasing patient age. These findings suggested that quadriceps tendon rupture can occur without pathologic tendon degeneration, especially in younger patients.
Etiology
Quadriceps tendon rupture usually occurs during a rapid, eccentric contraction of the quadriceps muscle, with the foot planted and the knee partially flexed. This injury commonly occurs during falls. Other mechanisms of injury include direct blows, lacerations, and iatrogenic causes. [17, 18, 19, 20, 21, 22, 23, 24, 25]
McMaster showed that normal tendons in rabbits do not rupture under stress. Instead, linear stress causes disruption at the musculotendinous junction, the muscle belly, or the tendinous insertion into bone. Harkness demonstrated that approximately 30 kg/mm2 of longitudinal stress may be applied to normal quadriceps tendons before they fail. Additionally, many ruptures occur after relatively trivial trauma. Therefore, tendon rupture usually occurs through a pathologic area of the tendon.
Many conditions have been reported to contribute to degeneration of the quadriceps tendon, including the following:
-
Infection
-
Metabolic disease
-
Steroid abuse [28]
-
Tumors
-
Immobilization
Repetitive motion has been implicated as the cause of jumper's knee. [29, 30]
Rare iatrogenic cases have been reported. Examples include rupture after total knee arthroplasty (TKA), lateral retinacular release, meniscectomy, and anterior cruciate ligament (ACL) reconstruction with central-third patellar tendon graft. In addition, steroid injections are believed to weaken tendons. Quadriceps tendon ruptures have also reportedly occurred with knee and patellar dislocations.
Epidemiology
When all types of knee injuries are considered, unilateral quadriceps tendon ruptures are relatively rare; bilateral ruptures are even less common. However, quadriceps tendon ruptures are more common than patellar tendon ruptures are, though they are also more likely to be misdiagnosed. [31]
As mentioned previously, quadriceps tendon rupture usually occurs in patients with predisposing factors who are older than 40 years, but these ruptures may be seen in nearly any age group. Siwek and Rao reviewed 69 cases reported in the literature from 1880 to 1978 and found that 88% of the ruptures were in patients aged 40 years or older. [8] To the authors' knowledge, the youngest patient was a 13-year-old who had been immobilized in a long leg cast before sustaining the injury.
In contrast, partial ruptures occur in young athletes. [5, 6] Raatikainen et al reported an average age of 28 years in a series of patients with partial tears. [32] Partial and complete tears occur predominantly in males.
Prognosis
Studies generally have reported good results after early repair of complete unilateral and bilateral quadriceps tendon ruptures. [33] The type of repair, the location of the tear, the patient's age and sex, and the mechanism of injury do not appear to affect the results. Good range of motion (ROM) usually can be regained, but some persistent quadriceps weakness is fairly common. Most patients can return to their previous occupation, but many cannot return to their preinjury activity level.
In a large study, Konrath et al found that 83% of patients returned to their previous occupations, 51% were unable to return to their preinjury activity levels, and 53% had persistent quadriceps strength deficits (>20% in comparison with the uninjured leg). [12] The injured leg had a mean thigh atrophy of 1.5 cm as compared with the uninjured leg.
Several studies have shown markedly worse results with delayed repairs. Rougraff et al reported significantly poorer functional results, lower satisfaction scores, and lower isokinetic data in patients with delayed repair. [11] Raatikainen et al reported good results from simple debridement and repair of partial quadriceps tendon ruptures. [32]
Because quadriceps tendon ruptures are most frequent between the ages of 50 and 60 years, the outcomes of timely surgical repair in older patients have received comparatively little study. Ellanti et al retrospectively reviewed all such ruptures occurring between 2009 and 2014 at their institution in patients older than 80 years (with penetrating trauma and partial ruptures excluded) [34] ; six of the 32 patients (mean age, 81.38 y) were eligible for study inclusion. At last follow-up (mean, 54 mo), the mean Lysholm score was 84.8/100 (good outcome), the mean Rougraff score was 21.3/25 (excellent outcome), and all patients considered themselves close to their premorbid mobility level.
In a retrospective continuous study that included 25 knees with acute quadriceps tendon rupture (22 patients; 17 males, 5 females; mean age, 64 y; age range, 52-87 y), Brossard compared the outcomes of suture-anchor fixation and the gold standard technique (ie, transosseous patellar suture). [35] Variables studied included active ROM, muscle strength, patient satisfaction, Lysholm score, return to work, and radiologic behavior of the anchors. At a mean follow-up of 7 years (range, 3-9 y), the outcomes with anchors were comparable to those with the gold standard technique.
-
Tendolipomatosis. Reprinted with permission from Kannus P, Józsa L. Histopathological changes preceding spontaneous rupture of a tendon. A controlled study of 891 patients. J Bone Joint Surg Am. Dec 1991;73(10):1507-25.
-
Toothlike ridging of the anterosuperior patella. Reproduced with permission from Greenspan A, Norman A, Tchang FK. "Tooth" sign in patellar degenerative disease. J Bone Joint Surg Am. Jun 1977;59(4):483-5.
-
Magnetic resonance imaging (MRI) scans of complete and incomplete quadriceps tendon ruptures. Reproduced with permission from Zeiss J, Saddemi SR, Ebraheim NA. MR imaging of the quadriceps tendon: normal layered configuration and its importance in cases of tendon rupture. AJR Am J Roentgenol. Nov 1992;159(5):1031-4.
-
Exposure of a tendon rupture.
-
Drill holes through the patella.
-
Passing suture through patellar drill holes.
-
Tendon pulled down into the patellar bony trough with sutures.
-
Finished repair.




