Background
The thumb plays an important role in hand function. Daily tasks involving pinch, grip, grasp, and precision handling are more easily accomplished with an opposable thumb. Traumatic loss, congenital absence, or hypoplasia diminishes or eliminates the thumb's prehensile abilities and may affect overall hand function.
Images relevant to thumb reconstruction are provided below:
Horta et al retrospectively reviewed 107 cases of thumb reconstruction in emergency situations using Moberg, radial innervated cross-finger, Venkataswami-Subramanian, Foucher, Tezcan, and Littler flaps. The Foucher flap was used the most often, in 56 cases, and the Tezcan flap proved to be a good alternative. [1]
According to Ray et al, when replantation of an avulsed/amputated thumb is not feasible, toe-to-hand transfer may be considered at initial presentation as an immediate one-stage transfer in appropriately chosen patients. In a retrospective study of 6 patients, great-toe transfer was safely and reliably performed and reduced hospitalization and operative and recovery time. In addition, according to the authors, it may speed up the return of function and return to work. [2]
History of the Procedure
Attempts to restore thumb function were recorded as early as 1874, when Huguier reported on the "phalangization" of the thumb metacarpal, which was carried out by deepening the first web space. [3] In 1900, Nicoladoni described a reconstruction procedure following traumatic amputation of the thumb in which a staged, pedicled transfer of the great toe was performed. [4] Development of microsurgical techniques allowed successful transfer of a toe to a thumb in monkeys in 1965 and in a human in 1966. [5, 6]
Reports of technical refinements in the toe-to-thumb transfer subsequently appeared in the literature. [7, 8] Congenital absence of the thumb from thalidomide exposure provided experience with index finger pollicization for thumb reconstruction. [9]
Problem
Congenital absence or traumatic injury to the thumb, resulting in a loss of its prehensile ability, significantly affects hand function.
Etiology
Traumatic loss, congenital absence, or hypoplasia of the thumb may result in a need for thumb replantation.
Indications
Restoration of the 5 components of thumb function described by Littler — stability, strength, mobility, sensibility, and posture — should serve as the basis for any reconstructive plan. [10] Consideration of these components and how they relate to each other allows a functional approach to the thumb deficit that guides the reconstructive hand surgeon. The goals of thumb reconstruction, as outlined by Heitmann and Levin, consist of the following [11] :
-
Sensate and nontender thumb tip
-
Stability at the interphalangeal (IP) and metacarpophalangeal (MCP) joints
-
Adequate strength to resist the forces of the fingers
-
Correct posture and positioning of the thumb with a wide webspace
-
Mobility of the carpometacarpal (CMC) joint with intrinsic muscles to aid prehension
Whether an indication for surgery is related to injury or congenital malformation of the thumb, the ultimate goal is optimal function of the hand. Pinch, fine manipulation, and power grip depend to some extent on stable, sensate skin in the pulp and a functional IP joint. The power grip is enhanced by the strength and mobility of the thumb, which in turn are largely defined by the integrity of the intrinsic and extrinsic musculature, as well as by the functionality of the CMC joint. [12, 13]
Selecting the most appropriate technique for thumb reconstruction depends on multiple factors, including the following:
-
Level of injury
-
Status of the remaining hand
-
Presence or absence of the thenar musculature
-
Age, occupation, overall health, and functional demands of the patient
In addition, the indication for surgery varies not only with the patient's needs and desires, but also with age, gender, and general health. The level of injury is among the most important factors to consider in deciding on the most appropriate reconstructive strategy. Kleinman and Strickland described a useful classification system, dividing the thumb into thirds: the distal phalanx, the proximal phalanx, and the metacarpal segment. [14]
The successful replantation of an amputated thumb restores the appearance of and some function to the injured hand. The procedure yields high satisfaction rates, whereas the functional outcome of other reconstructive methods tends to be less rewarding.
Relevant Anatomy
The thumb's arterial supply is provided mainly through the terminal branch of the radial artery, the princeps pollicis. This artery crosses the first intermetacarpal space to run on the volar aspect of the MCP joint, where it divides into the ulnar and radial collateral arteries. The ulnar collateral artery is usually larger than the radial collateral artery, and it is often easier to repair during replantation. The median nerve and the superficial radial nerve supply sensation to the palmar skin and to the dorsal side of the thumb, respectively.
The abductor pollicis longus, extensor pollicis brevis, and extensor pollicis longus extend the thumb. They insert at the base of the thumb metacarpal, proximal phalanx, and distal phalanx, respectively.
For more information about the relevant anatomy, see Hand Anatomy.
-
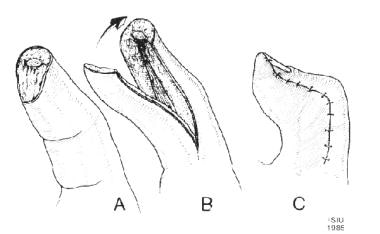
Diagram of a Moberg volar advancement flap being used for a thumb tip defect.
-
Marking for the radial incision of a Moberg flap.
-
Moberg flap raised just above the level of the flexor pollicis longus tendon sheath.
-
Markings for a volar advancement flap with modification of the incision at the base to allow closure in V-Y fashion after distal phalanx shortening.
-
Radial view of the markings for a volar advancement flap with modification of the incision at the base to allow closure in V-Y fashion after distal phalanx shortening.
-
Volar advancement flap with modification of the incision at the base to allow closure in V-Y fashion after distal phalanx shortening.
-
Thumb tip defect that is amenable to closure with a Moberg volar advancement flap.
-
Incision marking for a Moberg flap. The neurovascular bundle should be kept with the volar advancement flap.
-
Bridging vessel to the neurovascular bundle on a volar flap.
-
Flexion at the interphalangeal joint to allow closure.
-
Volar view of the closure of a thumb defect with a Moberg volar advancement flap.
-
Radial view of the closure of a thumb defect with a Moberg volar advancement flap.
-
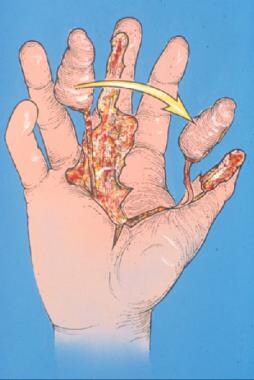
Diagram of a Littler neurovascular island flap for the coverage of a thumb tip defect.
-
Intraoperative view of a Littler neurovascular island flap.
-
Postoperative view of a Littler neurovascular island flap.
-
Second postoperative view of a Littler neurovascular island flap.
-
Markings for the pedicle of a first dorsal metacarpal artery flap.
-
Dissection for a first dorsal metacarpal artery flap.
-
Isolation of the pedicle for a first dorsal metacarpal artery flap.
-
Postoperative appearance of a thumb tip after coverage with a first dorsal metacarpal artery flap.
-
Second view of the postoperative appearance of a thumb after coverage with a first dorsal metacarpal artery flap.
-
Free tissue transfer of great toe pulp to restore a volar thumb defect.
-
Markings for a free tissue transfer of great toe pulp to restore a volar thumb defect.
-
Postoperative view after a free tissue transfer of great toe pulp to restore a volar defect.
-
Dorsal view of the clinical appearance of a Blauth type IV pouce flottant thumb.
-
Volar view of the clinical appearance of a Blauth type IV pouce flottant thumb.
-
Radiograph of a pouce flottant thumb
-
Pollicized index finger for thumb reconstruction at 2 weeks after surgery.
-
Functional use of a pollicized index finger at 8 weeks after surgery.