Practice Essentials
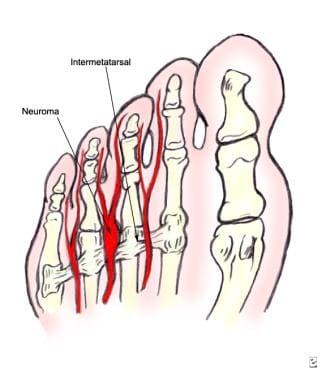
Morton neuroma, also referred to as interdigital neuroma or interdigital neuritis, is a common condition that involves enlargement of the interdigital nerve of the foot. [1] (See the image below.) It derives its common name from Thomas Morton, who, in 1876, first described interdigital nerve compression [2] and theorized that the nerve was being compressed between the metatarsal heads.
Interdigital neuritis is a mechanically induced nerve irritation due to intrinsic and extrinsic biomechanical factors that results in a combination of pain, paresthesia, and numbness in the forefoot. A greater understanding of forefoot anatomy and biomechanics has created an environment that facilitates further delineation of the pathophysiology of interdigital neuroma.
The biomechanical goals of nonsurgical management are to reduce forefoot compression and to eliminate the effect of intermetatarsal ligament tension. The indication for surgery is significant pain or dysfunction that is not tolerated by the patient and that fails to respond to conservative management. Once the diagnosis is made and conservative management has failed, few contraindications for surgical intervention exist. Local soft-tissue factors, such as infections or vascular insufficiency, are likely to be the only absolute contraindications.
Surgical procedures for treating Morton neuroma have historically been aimed either at directly dealing with the pathologic nerve or at altering the local biomechanical environment in which the nerve exists. The evolution of surgical care has resulted in some basic principles and goals, which are the foundation for the current surgical options. There is a growing body of literature that elaborates on many aspects of this seemingly simple problem.
This article outlines some current controversies regarding Morton neuroma; the fact that the eponym is likely a misnomer (see Pathophysiology) is a reflection of these controversies. The histology, use of adjunctive imaging modalities, and choice of surgical procedure all involve some variance of opinion. Current and future work will be addressing these issues.
Anatomy
The medial plantar nerve has four digital branches that begin at the medial aspect of the great toe and then form the common digital nerves of the first, second, and third web spaces. The lateral plantar nerve supplies the fourth web space and, in 27% of patients, contributes to the third web space. This increased thickness of the third digital nerve was hypothesized to predispose it to mechanical irritation; however, studies have shown no correlation between those patients with this anatomic variant and those with symptoms of Morton neuroma.
The common digital nerves lie plantar to the intermetatarsal ligament and give off small branches to the plantar skin approximately 1-2 cm proximal to the bifurcation of the nerve. These branches also must be resected at the time of surgery because they may prevent nerve stump retraction after neurectomy and lead to a recurrent neuroma. [2]
Pathophysiology
The term neuroma, as applied to this condition, may be a misnomer. Morton neuroma may be best described as a clinical syndrome stemming from a constellation of factors related to the local anatomy and the forces applied on the forefoot with ambulation and shoe wear. [3] Interestingly, it is not uncommon for the histopathology to be interpreted as relatively normal, even when classic preoperative findings are present and dramatic postoperative results are achieved. Clearly, the histopathology is not that of a typical neuroma. [4] Some or all of the following may be observed:
-
Sclerosis of the endoneurium
-
Hyalinization of the walls of endoneurial vessels
-
Thickened perineurium
-
Demyelination of nerve fibers
Etiology
Anatomic studies have revealed a wealth of information and helped to resolve some misconceptions regarding the etiology of this disease. The intermetatarsal space is narrower in the second and third interspaces than in the first and fourth interspaces, and this difference correlates with the clinical presentation pattern. [5] The composition of the tarsometatarsal (TMT) articulation allows relative hypermobility between the second and third metatarsals, which contributes to mechanical irritation of the nerve.
Narrow toe-box footwear can exacerbate the compression between the metatarsal heads, and hyperextension of the toes in high-heeled shoes tethers the nerve beneath the ligament and may expose it to more biomechanical stresses with gait. [4] Less commonly, metatarsophalangeal (MTP) joint pathology, inflamed bursa, or lipomas can create compression at the level of the common digital nerve.
Epidemiology
Morton neuromas are more common in women, with a female-to-male ratio of 4:1. They tend to occur in the fifth decade of life and frequently are exacerbated by constrictive footwear. [4] Symptoms are typically unilateral, with the third interspace most often involved, followed by the second and the fourth interspaces. [4] Simultaneous neuromas occurring in the same foot are uncommon. [6]
Prognosis
In general, review of the orthopedic literature from the past several decades supports an estimate of 75-95% satisfactory results after surgical intervention, regardless of technique or approach. Nonsurgical management probably results in a 20-30% success rate.
Long-term postoperative outcomes have been quantified. [7, 8, 9, 10, 11]
Coughlin et al monitored 66 patients (71 feet, 74 neuromas) over an average of 5.8 years. [7] A dorsal approach was used, and a neurectomy was performed 3 cm proximal to the intermetatarsal ligament. The results were as follows:
-
Histology was available on 72 of the 74 specimens, and all were neuromas
-
Rates were excellent in 61% (no problems, no or only mild pain), good in 24% (few problems, mild pain at most, willingness to have surgery again), fair in 8% (moderate pain, some difficulty walking, reservations about surgery outcome), and poor in 8% (continued pain and difficulty walking, regrets about having surgery)
-
Thirty percent had no shoe-wear restrictions, 53% had mild restrictions, and 17% had major restrictions
-
Sixty-five percent of the feet were pain-free, and 4% were severely painful
-
Complications included one deep infection requiring incision and drainage; six superficial infections resolved with antibiotics; intractable plantar keratosis in lesser metatarsal heads in 15% of the feet, one of which had MTP joint instability; and continued major shoe-wear restriction believed to be related to neuroma surgery in 8%
A study by Nery et al retrospectively followed 168 consecutive patients in whom nonoperative management had failed (median follow-up, 7.1 y). [8] All patients underwent magnetic resonance imaging (MRI) to rule out other pathology and, after neurectomy, had a pathology-proven neuroma. In contrast to the approach followed by Coughlin et al, the surgical procedure involved a transverse plantar approach and preservation of the deep transverse incision. The results were as follows:
-
A good result (no pain or paresthesia) occurred in 89%, a fair result (mild pain or paresthesia without recurrence) in 7%, and a poor result (complications or persistent symptoms) in 4%
-
In all patients with a poor result, a recurrent neuroma was found on a second surgery and resected; all were subsequently asymptomatic
The study authors concluded that the transverse plantar incision approach for Morton neuroma resection is comparable in outcomes to other approaches. They also stated that MRI is not needed for diagnosis but was required in these cases by insurance providers.
Akermark et al followed 55 patients with a longitudinal plantar incision for at least 2 years and found an 86% rate of overall satisfaction. [10] The complication rate in this study was low (5%) and may have been related to the meticulous care taken to keep scar formation between the metatarsal heads.
Colgrove et al compared transposition with resection in a randomized trial. [9] At the 36- to 48-month follow-up, they found the resection group to have 86% excellent results and 14% fair results; meanwhile, the transposition group had 96% excellent results and 4% good results. The authors concluded that resection is unnecessary for symptom relief. To date, however, no repeat study has been conducted to confirm their results.
Kasparek et al reported good-to-excellent results in 75 (77%) feet at a mean of 15.3 years after surgery in their retrospective series. [11]
Reichert et al assessed the long-term results of dorsal neurectomy in 41 patients treated for Morton neuroma (average follow-up, 7.4 y; range, 5-12). [12] Mean American Orthopedic Foot and Ankle Society (AOFAS) score rose from 39.4 ± 7.84 preoperatively to 83.4 ± 12.1 postoperatively; mean visual analogue scale (VAS) score fell from 7.04 ± 1.4 preoperatively to 1.4 ± 0.8 postoperatively. Results were reported as very good in 31 patients, good in six, satisfactory in one, and poor in three. Single neuromas that were larger than 3 mm and were resected within 12 months of symptom onset were associated with the best results.
Kundert et al prospectively studied clinical outcomes and complications in 44 patients (51 feet, 56 neuromas) who underwent excision of Morton neuroma via a plantar longitudinal approach. [13] Mean VAS score fell from 8 preoperatively to 0.4 at final follow-up (mean, 54 mo; range, 12-99). The overall complication rate was 7.1%, and the incidence of scar problems (eg, delayed wound healing, hypertrophic scar formation, and inclusion cyst) was 5.2%.
Bucknall et al performed a prospective study aimed at determining pre- and postoperative outcomes and satisfaction scores in 99 consecutive patients (78 women, 21 men; 111 feet) who underwent excision of Morton neuroma. [14] They documented statistically significant differences between mean pre- and postoperative scores on the Manchester-Oxford Foot Questionnaire (MOXFQ) and the physical component of the Short Form (SF)-12.
In this study, 10 patients were dissatisfied, describing results as poor or very poor; however, most were satisfied, describing results as good or excellent. [14] At follow-up, 63 of the 99 patients were pain-free; eight had worse scores than they had before the procedure. No statistically significant difference in outcome was found between single-site surgery and multiple-site surgery. Revision surgery was associated with significantly worse MOXFQ scores.
-
Plantar view showing relationships between metatarsal heads, intermetatarsal ligament, and neuroma.
-
Image demonstrates key provocative physical examination maneuver: simultaneous forefoot compression coupled with intermetatarsal space compression.
-
Histopathology reveals nerve fibers and pacinian corpuscles entrapped within fibromyxoid connective tissue.
-
Surgery for Morton neuroma. Dorsal incision.
-
Surgery for Morton neuroma. Superficial exposure.
-
Surgery for Morton neuroma. Deeper dissection.
-
Surgery for Morton neuroma. Neuroma and adherent fibrofatty tissue.
-
Surgery for Morton neuroma. Distal plantar transverse incision.
-
Surgery for Morton neuroma. Plantar longitudinal incision.