Practice Essentials
Cysts can occur in many shapes and forms around the knee, as shown in the images below. A cyst is defined as a closed cavity, or sac, that is lined with epithelium. It can contain liquid or semisolid material, can be normal or abnormal, and can occur in soft tissue or in bone. Benign or malignant masses must be distinguished from cystic lesions. This article discusses benign cysts that occur in the soft tissue around the knee or outside bone and that are filled with fluid or semisolid material. See the images below.
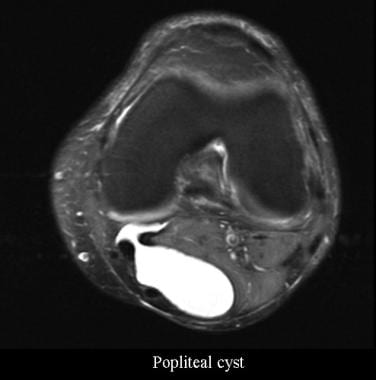 Popliteal cyst. Courtesy of James K. DeOrio, MD, Laura W. Bancroft, MD, and Jeffrey J. Peterson, MD.
Popliteal cyst. Courtesy of James K. DeOrio, MD, Laura W. Bancroft, MD, and Jeffrey J. Peterson, MD.
 Ganglion of the anterior cruciate ligament. Courtesy of James K. DeOrio, MD, Laura W. Bancroft, MD, and Jeffrey J. Peterson, MD.
Ganglion of the anterior cruciate ligament. Courtesy of James K. DeOrio, MD, Laura W. Bancroft, MD, and Jeffrey J. Peterson, MD.
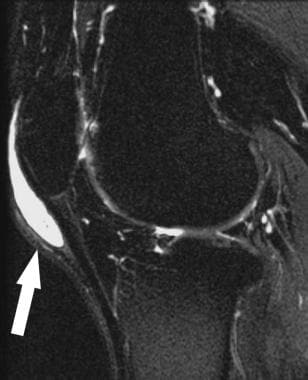
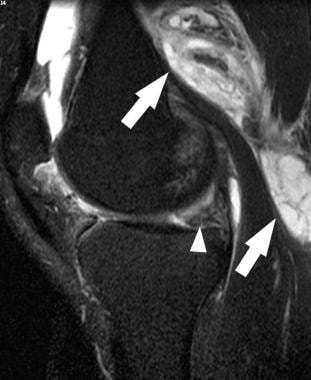 Baker cyst. Sagittal T2-weighted magnetic resonance image shows a large Baker cyst (arrow) posteromedial to the joint capsule and adjacent to the medial gastrocnemius muscle. Note the joint effusion and underlying complex tear of the medial meniscus (arrowhead). Courtesy of William B. Morrison, MD.
Baker cyst. Sagittal T2-weighted magnetic resonance image shows a large Baker cyst (arrow) posteromedial to the joint capsule and adjacent to the medial gastrocnemius muscle. Note the joint effusion and underlying complex tear of the medial meniscus (arrowhead). Courtesy of William B. Morrison, MD.
 Meniscal cyst. Coronal T2-weighted magnetic resonance image shows a cyst (arrow) adjacent to the lateral meniscus (arrowhead) and also demonstrates a tear communicating with the cyst. Courtesy of William B. Morrison, MD.
Meniscal cyst. Coronal T2-weighted magnetic resonance image shows a cyst (arrow) adjacent to the lateral meniscus (arrowhead) and also demonstrates a tear communicating with the cyst. Courtesy of William B. Morrison, MD.
 Tibial subchondral cyst. Courtesy of James K. DeOrio, MD, Laura W. Bancroft, MD, and Jeffrey J. Peterson, MD.
Tibial subchondral cyst. Courtesy of James K. DeOrio, MD, Laura W. Bancroft, MD, and Jeffrey J. Peterson, MD.
The understanding of various knee cysts is highly dependent on a thorough knowledge of the anatomy of the knee, which is a highly mobile structure. Bursae—sacs or saclike structures that are located at places where friction develops between the soft tissues and around the bony prominences—line many of the ligaments, tendons, and bony prominences around the knee. They can be lined with synovium and respond much the way synovium does to insults and pathologic conditions. Bursae can fill with fluid, and this accounts for the large majority of cysts seen around the knee.
According to Gray's Anatomy of the Human Body, there are at least 13 bursae around the knee. [1] Four are present anteriorly; the largest is between the patella and skin. Four are present laterally and posterolaterally. Five are present medially and posteromedially. The bursa between the medial head of the gastrocnemius and the knee capsule, as well as the bursa between the lateral gastrocnemius head and the capsule, often communicate with the knee joint. Although normally quiescent, any of these bursae can become inflamed, fill with fluid, and present as a cystic mass.
Two types of bursae are described: those normally present and adventitious ones. The adventitious type occurs as a result of chronic irritation over abnormal bony prominences such as an osteochondroma or bunion. This type of bursa lacks an epithelial lining; however, it can become filled with blood from repetitive trauma and it can also become infected.
Other soft tissue cysts that occur around the knee are entities such as ganglion cysts; intraneural cysts; popliteal artery cysts and other vascular masses; and a wide assortment of secondary cysts, such as those caused by rheumatoid arthritis and osteoarthritis and those resulting from blood- or pus-filled bursae.
Crema et al, as part of the Multicenter Osteoarthritis Study (MOST), found that most subchondral cysts demonstrated full or partial contrast enhancement on MRI and were located adjacent or in the midst of enhancing bone marrow edema-like lesions. The authors noted that because pure cystic lesions are not expected to enhance on MRI, the term "subchondral cyst-like bone marrow lesion" may be appropriate to describe these lesions. [2]
Four hundred knees were included in the study. Subchondral cysts were detected in 260 of 5600 subregions (4.6%). After intravenous contrast administration, 245 cysts (94.2%) showed full enhancement; 12 (4.6%), partial enhancement; and three (1.2%), no enhancement. Enhancing bone marrow edema-like lesions (BMLs) were found in 237 (91.2%) subregions containing cysts, which were located adjacent to or in the middle of BMLs. In 121 subregions (46.5%) having cysts, no adjacent full-thickness cartilage loss was detected. [2]
Chatzopoulos et al found that Baker cysts were present in 72 of 195 (37%) patients with knee osteoarthritis. Abnormal and intense tracer accumulation in early-phase bone scintigraphy were significantly more frequent in osteoarthritic knees with Baker cysts than in those without. The authors noted that clinical and radiographic variables were not able to predict the presence of those cysts. [3]
For patient education information, see Knee Pain Health Center.
History of the Procedure
Determination of the treatment plan depends on the individual patient and the patient's diagnosis. Nonoperative treatment, including limitation of activity and aspiration of the cyst (with or without injection of corticosteroids), is usually the treatment of choice. Surgical treatment should not be the first option chosen and is not required in most instances. However, once nonoperative treatment is exhausted, the surgical treatment of choice for most cystic masses is excision.
Excision of the cyst requires a thorough knowledge of the relationships of the ligaments, tendons, and bone structures of the knee. Surgical excision of these cysts has probably been performed since anatomic dissections were first begun. The surgical approach to excision is based on the location and origin of the cyst. Adhering to the basic principles of skin incisions and proper dissection of the tissues can greatly aid in achieving a good result.
In the case of meniscal cysts, the treatment approach may differ. Nonoperative measures do not accomplish much more than the temporary relief of symptoms. Symptomatic meniscal cysts are usually treated by addressing the cause and performing an arthroscopic partial meniscectomy with cyst decompression. [4] Direct excision of a meniscal cyst is rarely required.
Problem
The problems related to cysts around the knee are largely proportional to the size and location of the cyst. [5] One of the most common knee cysts is the popliteal cyst, otherwise known as a Baker cyst; its symptoms can include pain. [6] This type of cyst most often develops in the bursa beneath the medial head of the gastrocnemius and from the semimembranosus bursa. Because the development of popliteal cysts correlates with intra-articular pathology, they usually point to a problem of one or both menisci, a complete or partial cruciate ligament tear, a chondral injury, or a combination of any of these.
Large popliteal cysts can rupture and become quite painful; it is important to rule out deep vein thrombosis in these instances. Meniscal cysts, as previously noted, are problematic because of the pain that is often associated with a palpable, firm mass.
Epidemiology
Frequency
Sansone et al reported a 4.7% prevalence rate of popliteal cysts in a series of 1001 adult patients. [7] Their most common associated lesions were meniscal lesions (83%), most frequently involving the posterior horn of the medial meniscus. The authors also found that 43% of the meniscal lesions were associated with articular cartilage damage and that 32% were associated with anterior cruciate ligament tears.
However, in children, popliteal cysts usually do not communicate with the knee joint; in rare cases, the cysts are associated with intra-articular pathology. In most cases, the cysts are self-limited; they rarely require surgical excision.
Meniscal cysts are less common. The prevalence rate is 1.5-4%. The literature has conflicting reports regarding the most common location of meniscal cysts. According to Campbell et al, in a series of 2572 knee magnetic resonance images (MRIs), meniscal cysts of the medial meniscus were noted to be nearly 2 times more common than cysts of the lateral meniscus. [8] However, in an earlier study by Ryu and Ting, medial and lateral meniscal cysts occurred with equal frequency in a small series of 18 patients. [9]
One of the most common bursa affected by chronic trauma is the prepatellar bursa. The resulting condition is also known as housemaid's knee or carpet layer's knee and occurs as a result of the repetitive trauma from kneeling. The prepatellar bursa can become filled with a hematoma and develop a thick capsule, thereby making it feel firm. [10] Other less common bursae that become inflamed are the medial collateral ligament bursa, lateral collateral ligament bursa, infrapatellar bursa, medial gastrocnemius bursa, and the semimembranosus bursa.
Multiple reports have described less common benign cysts about the knee. These include ganglion cysts, as shown in the images below, that occur in various areas (eg, cruciate ligaments) and synovium cyst enlargements at the proximal tibiofibular joint. [11] The latter cysts can potentially cause neurologic compromise of the peroneal nerve. Cystic adventitial disease of the popliteal artery has also been reported. Patients with these cysts present with intermittent claudication because the cysts compress the popliteal artery.
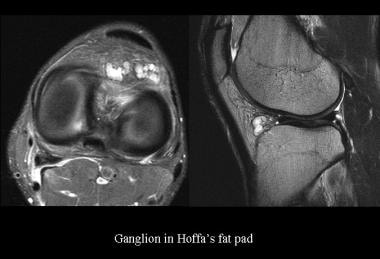 Ganglion in the Hoffa fat pad. Courtesy of James K. DeOrio, MD, Laura W. Bancroft, MD, and Jeffrey J. Peterson, MD.
Ganglion in the Hoffa fat pad. Courtesy of James K. DeOrio, MD, Laura W. Bancroft, MD, and Jeffrey J. Peterson, MD.
 Ganglion of the anterior cruciate ligament. Courtesy of James K. DeOrio, MD, Laura W. Bancroft, MD, and Jeffrey J. Peterson, MD.
Ganglion of the anterior cruciate ligament. Courtesy of James K. DeOrio, MD, Laura W. Bancroft, MD, and Jeffrey J. Peterson, MD.
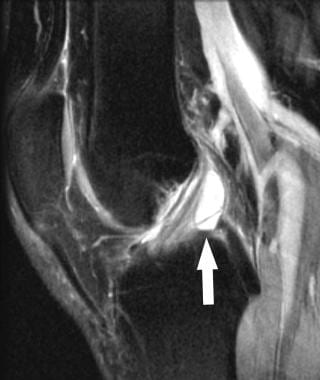 Cruciate ganglion. Sagittal T2-weighted magnetic resonance image shows a cyst (arrow) that slightly displaces the otherwise normal-appearing anterior cruciate ligament. Courtesy of William B. Morrison, MD.
Cruciate ganglion. Sagittal T2-weighted magnetic resonance image shows a cyst (arrow) that slightly displaces the otherwise normal-appearing anterior cruciate ligament. Courtesy of William B. Morrison, MD.
Reports also describe cases of myxoid intraneural cysts of the common peroneal nerve that are associated with pain around the knee and leg and that require surgical excision. [12] The importance of always considering the possibility that any cyst around the knee can become infected is demonstrated by a rare case report of a popliteal cyst infected with Neisseria gonorrhoeae. [13]
Etiology
Cysts about the knee have multiple etiologies, including irritated and inflamed bursae, meniscal cysts caused by intra-articular pathology, and special categories, such the following:
-
Baker cyst or popliteal cyst
-
Ganglia (both intra-articular and extra-articular)
-
Extraneural cysts
It is important to realize that other processes can mimic cysts on MRI. [14] Benign and malignant tumors must be ruled out during the workup of any cyst about the knee; other entities to consider are abscesses and vascular masses, such as popliteal vein varices and popliteal artery aneurysms.
Pathophysiology
The pathophysiology of benign knee cysts depends on the specific etiology. Although at times controversial, the underlying causes of most cysts are similar; a benign cyst results whenever a saclike structure is formed secondary to a mechanical or biochemical irritant. A sac that already is present, such as an epithelial-lined bursa, is subject to the same irritants. These potential spaces then become filled with a fluid or with degenerative myxoid products. Over time, the cyst becomes mucoid and semisolid if resorption of the fluid is slow and if the fluid has a high protein content.
Presentation
History
The workup of all cysts about the knee should start with a thorough history and physical examination. The history should include the following:
-
The patient's age and sex
-
The exact location of the cyst around the knee and the length of time it has been present
-
If pain is present, all of its characteristics
-
The activity level of the patient and any recent change in activity level
-
Any recent trauma to the knee
-
Any associated medical conditions, such as rheumatoid arthritis, osteoarthritis, gout, tuberculosis, sexually transmitted diseases, infection, and neoplastic disease
-
Any prior surgery of the knee
-
Type of treatment undertaken to date
Physical
Physical examination should include the following:
-
Careful assessment for ligament or meniscal injury
-
Comparison between the appearance of the affected knee and that of the unaffected side, as well as range of motion
-
Direct palpation of the cyst to determine its relation to anatomic landmarks, its size, and its consistency
-
Results of stability testing of all ligaments and meniscus-specific signs
Presentation
The clinical presentation of the more common cysts about the knee is that of a nonpainful or minimally painful soft mass. The location depends on which extra-articular structure is involved. Popliteal cysts, as shown in the image below, usually present as a nonpainful posterior popliteal mass. Patients may also have intra-articular knee symptoms, as well. When pain is present, it is most often due to the intra-articular process that is responsible for the popliteal cyst. Children usually present with a nonpainful mass that is noticed by an adult.
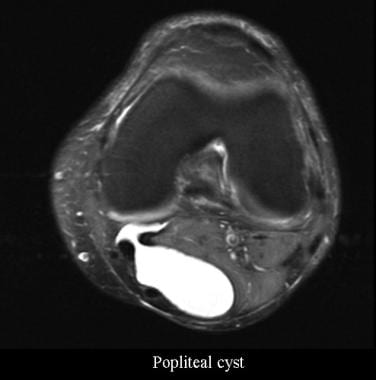 Popliteal cyst. Courtesy of James K. DeOrio, MD, Laura W. Bancroft, MD, and Jeffrey J. Peterson, MD.
Popliteal cyst. Courtesy of James K. DeOrio, MD, Laura W. Bancroft, MD, and Jeffrey J. Peterson, MD.
Swollen and inflamed bursae can be painful. Prepatellar bursitis, as shown in the image below, can occur following repetitive trauma of recurrent kneeling, is often occupation-related, and can degenerate and become infected in the acute setting. A pes anserinus bursa, an infrapatellar bursa, and a collateral ligament bursa can also appear as painful, swollen masses in their respective areas.
 Prepatellar bursitis. Sagittal T2-weighted magnetic resonance image shows a fluid collection (arrow) anterior to the patella. Courtesy of William B. Morrison, MD.
Prepatellar bursitis. Sagittal T2-weighted magnetic resonance image shows a fluid collection (arrow) anterior to the patella. Courtesy of William B. Morrison, MD.
Meniscal cysts, as shown in the images below, most often manifest as pain that is aggravated by activity. These are sometimes palpable, most often on the lateral side, along the anterolateral aspect of the knee joint. Meniscal cysts are more difficult to palpate on the medial side of the knee because they tend to dissect in the tissue planes.
 Meniscal cyst. Coronal T2-weighted magnetic resonance image shows a cyst (arrow) adjacent to the lateral meniscus (arrowhead) and also demonstrates a tear communicating with the cyst. Courtesy of William B. Morrison, MD.
Meniscal cyst. Coronal T2-weighted magnetic resonance image shows a cyst (arrow) adjacent to the lateral meniscus (arrowhead) and also demonstrates a tear communicating with the cyst. Courtesy of William B. Morrison, MD.
Other less common benign cysts about the knee, such as intraneural cysts of the common peroneal nerve, present with pain and sensory changes in the anterior tibial nerve along the anterior aspect of the leg and dorsum of the foot. The muscles of the anterior compartment of the leg can also be involved, manifesting clinically as a footdrop. Patients with cystic adventitial disease of the popliteal artery have been reported to present with intermittent claudication. [15]
Indications
Surgical indications for the excision of cysts about the knee depend on the origin and cause of the cyst. Treatment of bursal cysts is nonoperative and aimed at the etiology, whether it is mechanical, biochemical, or immunologic. An adventitial bursa can occur over any prominence (eg, osteochondroma, large osteophyte, surgically placed hardware). Removing the prominence treats the bursitis. Bursal cysts that become inflamed because of a systemic reason are treated by addressing the systemic cause for the swelling and inflammation. Local measures to control swelling also can be used, such as rest, heat, compression, elevation, and immobilization.
Indications for surgical treatment of a meniscal cyst are pain that interferes with activity and a palpable mass along the lateral or medial joint line. The diagnosis can be confirmed with an MRI, although an MRI is not necessary with the presence of every knee cyst.
Popliteal cysts are usually not surgically excised. Surgical treatment is aimed at the inciting cause of the cyst and typically involves knee arthroscopy to look for an intra-articular process. MRI can be helpful in guiding and developing a treatment plan. Smith et al reported safe and effective treatment of symptomati popliteal cysts with ultrasound-guided aspiration of fluid through a spinal needle, fenestration of the cyst walls and septations, and injection of 1 mL triamcinolone and 2 mL 0.5% bupivacaine into the decompressed remnant. [16]
Surgical treatment is usually indicated for more rare types of cysts, such as the following:
-
Intraneural cysts
-
Popliteal artery cystic adventitial disease
-
Arterial aneurysms
-
Symptomatic ganglia
Relevant Anatomy
Knowledge of the bursae, tendon sheaths, fascial planes, tendons, ligaments, muscle, articular capsules, major nerves, arteries, veins, and the bony prominences around the knee is critical to the proper surgical and nonsurgical treatment of knee cysts. The most relevant of these structures is the location of the various bursae and tendon sheaths. [17]
Considering that the knee is a very mobile structure, it makes sense that there are numerous bursae to allow for the smooth gliding of tendons, muscles, bone, and skin over each other. The most significant bursa are as follows:
-
Anterior knee: Prepatellar, suprapatellar, and deep infrapatellar bursae
-
Medial and posteromedial knee: Pes anserine, medial gastrocnemius, semimembranosus, and medial collateral ligament bursae
-
Lateral and posterolateral knee: Inferior bursa of the biceps femoris, as well as the bursae of the lateral gastrocnemius, the iliotibial tract, the lateral collateral ligament, and the popliteal tendon
Contraindications
There are no contraindications to the excision of knee cysts; however, a complete diagnostic workup must be performed prior to excision. Thorough knowledge of the behavior and etiology of the cyst should be understood. For example, popliteal cysts in the adult usually resolve after addressing their cause, such as meniscal pathology (eg, arthroscopic resection of a meniscal tear). Surgical excision of a popliteal cyst is rarely performed.
-
Popliteal cyst. Courtesy of James K. DeOrio, MD, Laura W. Bancroft, MD, and Jeffrey J. Peterson, MD.
-
Ganglion in the Hoffa fat pad. Courtesy of James K. DeOrio, MD, Laura W. Bancroft, MD, and Jeffrey J. Peterson, MD.
-
Ganglion of the anterior cruciate ligament. Courtesy of James K. DeOrio, MD, Laura W. Bancroft, MD, and Jeffrey J. Peterson, MD.
-
Meniscal cyst. Courtesy of James K. DeOrio, MD, Laura W. Bancroft, MD, and Jeffrey J. Peterson, MD.
-
Tibial subchondral cyst. Courtesy of James K. DeOrio, MD, Laura W. Bancroft, MD, and Jeffrey J. Peterson, MD.
-
Baker cyst. Sagittal T2-weighted magnetic resonance image shows a large Baker cyst (arrow) posteromedial to the joint capsule and adjacent to the medial gastrocnemius muscle. Note the joint effusion and underlying complex tear of the medial meniscus (arrowhead). Courtesy of William B. Morrison, MD.
-
Meniscal cyst. Coronal T2-weighted magnetic resonance image shows a cyst (arrow) adjacent to the lateral meniscus (arrowhead) and also demonstrates a tear communicating with the cyst. Courtesy of William B. Morrison, MD.
-
Prepatellar bursitis. Sagittal T2-weighted magnetic resonance image shows a fluid collection (arrow) anterior to the patella. Courtesy of William B. Morrison, MD.
-
Cruciate ganglion. Sagittal T2-weighted magnetic resonance image shows a cyst (arrow) that slightly displaces the otherwise normal-appearing anterior cruciate ligament. Courtesy of William B. Morrison, MD.




