Background
A triple arthrodesis is a procedure consisting of the surgical fusion of the talocalcaneal (TC), talonavicular (TN), and calcaneocuboid (CC) joints in the foot. The primary goals of a triple arthrodesis are to relieve pain from arthritic, deformed, or unstable joints. Other important goals are the correction of deformity and the creation of a stable, balanced plantigrade foot for ambulation.
Edwin W Ryerson first described triple arthrodesis in 1923 as a fusion of the TC, TN, and CC joints. The aim was to create a well-aligned, plantigrade, and stable foot that would allow patients with paralytic or deforming conditions to function better. The most common indications were to correct lower-extremity deformities in children resulting from poliomyelitis, cerebral palsy, Charcot-Marie-Tooth disease, clubfoot, or tuberculosis.
The original procedures were performed by removing large blocks of subchondral bone and correcting the angular deformities by inserting or removing wedges. The corrections were maintained by casting that often required later manipulation for loss of position. Kirschner wires (K-wires), Steinmann pins, and staples were used over time to hold the corrections in place but are now not as common.
Internal fixation with various compression screws using the Arbeitsgemeinschaft für Osteosynthesefragen (AO) technique and specially designed plating systems has become the standard of care.
For patient education resources, see the Foot, Ankle, Knee, and Hip Center and Arthritis Center, as well as Rheumatoid Arthritis.
Indications
Triple arthrodesis should be considered a salvage procedure and should be employed only after other conservative treatment modalities have been exhausted. The primary goals are to abolish pain, correct underlying deformity, and restore a stable platform for ambulation. In conditions where a lesser fusion or soft-tissue procedure will suffice, triple arthrodesis should not be used, because of the potential long-term complications associated with it. The primary indications for the procedure are as follows [1] :
-
Valgus foot deformities that cannot be adequately braced
-
Collapsing pes planovalgus deformity
-
Advanced tibialis posterior tendon dysfunction
-
Rheumatoid arthritis (RA)
-
Degenerative arthritis (eg, degenerative joint disease [DJD])
-
Posttraumatic arthritis
-
Chronic pain
-
Varus foot deformities that cannot be adequately braced
-
Cavus and cavovarus [2]
-
Talipes equinovarus
-
Joint instability
-
Neuromuscular disease
The use of triple arthrodesis to treat Mueller-Weiss disease has also been described. [3, 4]
Contraindications
Contraindications for triple arthrodesis include conditions that can be adequately corrected and maintained via external bracing, soft-tissue procedures, tendon balancing, or lesser fusions (eg, double arthrodesis without CC joint fusion [5, 6] ). Chronic smoking is a relative contraindication because of the associated high incidence of nonunion. [7]
Technical Considerations
Anatomy
The bony anatomy consists of the talus, the calcaneus, the cuboid, and the navicular. The talus and the calcaneus make up the TC joint (also referred to as the subtalar joint). Its articular portion is composed of the more important posterior facets of the talus and calcaneus and the smaller anterior and middle facets. The anterior talofibular, posterior talofibular, calcaneofibular, deltoid, and interosseous TC ligaments stabilize it.
Subtalar motion is triplanar and is described appropriately as pronation (dorsiflexion, eversion, and external rotation) and supination (plantarflexion, inversion, and internal rotation). Clinically, however, most motion takes place in the frontal plane and is seen as heel eversion and inversion. Although normal range-of-motion (ROM) values are difficult to measure, a practical rule of thumb is 30° of total motion with approximately 10° of inversion and 20° of eversion.
The sinus tarsi is a tunnellike structure extending from distal lateral to posterior medial in the rearfoot. It is formed dorsally by the concavity in the neck of the talus and plantarly by the sulcus between the posterior facet and sustentaculum tali of the calcaneus. This structure is widest laterally and contains the bifurcate, cervical, and interosseous ligaments. It is filled by a fatty plug known as the Hoke tonsil and serves as the origin of the extensor digitorum brevis (EDB).
The head of the talus and the navicular constitute the TN joint. This is a condylar joint. The head of the talus is convex, and the corresponding surface of the navicular is concave. This is an important spatial relation to understand because the navicular forms a lip around a portion of the talar head, making it difficult to access the joint fully and remove adequate amounts of cartilage.
Normally, during stance phase, the calcaneus everts, and the talus plantarflexes and internally rotates. This action produces a relative dorsiflexion, eversion, and abduction of the navicular, which subsequently translates that motion to the forefoot. In excessive or pathologic cases, this presents as medial arch collapse with forefoot abduction. The opposite takes place with weightbearing TC joint supination.
The anterior articular portion of the calcaneus and the cuboid make up the CC joint. This is often the first joint resected during a triple arthrodesis and is the most easily accessible of the three joints. Directly superior to the joint is the EDB muscle belly, and lateral to it are the peroneal tendons.
The sural nerve courses along the lateral side of the foot, and the superficial peroneal nerve takes a more dorsal lateral position. It should be noted that there is significant anatomic variation of the sural nerve, and care must be exercised in making the incision. The lateral incision is placed between these two nerves. The saphenous nerve and vein enter the foot on the dorsal medial aspect. A medial incision is also made and is usually located in line with and just plantar to these structures.
For more information about the relevant anatomy, see Foot Bone Anatomy and Ankle Joint Anatomy.
Procedural planning
Presentations in the clinic can vary, depending on the underlying pathology. A common feature of patients is the development of DJD. Conditions that produce an improperly functioning, unstable foot that leads to DJD are the main indications for surgical treatment.
TC joint arthritis usually manifests as pain located anterior to the distal tip of the fibula in the region of the sinus tarsi. The pain is exacerbated with forced inversion and eversion of the heel. In advanced cases, crepitation is noted with forced ROM. Similar findings can be seen in the CC and TN joints. Pain is usually elicited with periarticular palpation.
Depending on the underlying pathology, the patient may present with a varus or valgus deformity. Posttraumatic arthritis often presents with a rectus foot and complaints consistent with DJD of the TC joint. It commonly occurs after calcaneal fractures with posterior facet involvement.
Depending on the severity of the fracture, the heel can be shortened, can be widened, and can have an uneven lateral wall with bony prominences (see the images below). These findings are typically seen in lateral-wall blowout fractures that do not undergo open reduction with internal fixation (ORIF). Similar fractures with inadequate ORIF, or inadequate reduction, leaving a varus or valgus deformity, can also be seen in these cases.
 Lateral wall blowout fracture with comminution. Note shortening and widening of heel. If left untreated, heel would remain in varus with uneven lateral wall and bony prominence that could become irritated.
Lateral wall blowout fracture with comminution. Note shortening and widening of heel. If left untreated, heel would remain in varus with uneven lateral wall and bony prominence that could become irritated.
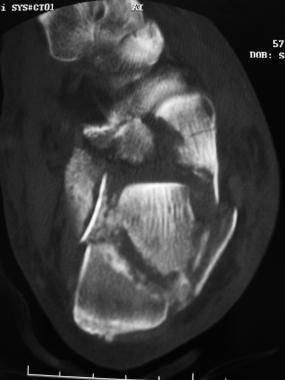 Lateral wall blowout fracture with comminution. Note shortening and widening of heel. If left untreated, heel would remain in varus with uneven lateral wall and bony prominence that could become irritated.
Lateral wall blowout fracture with comminution. Note shortening and widening of heel. If left untreated, heel would remain in varus with uneven lateral wall and bony prominence that could become irritated.
Valgus deformities are commonly seen in collapsing pes planovalgus, late-stage tibialis posterior tendon dysfunction, tarsal coalition, and some neuromuscular conditions. They are easy to identify, especially in the latter stages of the deformity, and present with a heel in valgus, an abducted forefoot, and a medial arch that is typically collapsed (see the images below).
 Valgus foot deformity with medial dislocation of talar head. Note abducted forefoot and head of talus rotated medially on navicular.
Valgus foot deformity with medial dislocation of talar head. Note abducted forefoot and head of talus rotated medially on navicular.
 Valgus foot deformity with medial dislocation of talar head. Note abducted forefoot and head of talus rotated medially on navicular.
Valgus foot deformity with medial dislocation of talar head. Note abducted forefoot and head of talus rotated medially on navicular.
 Valgus deformity with medial talar rotation that is so severe that patient bears weight on head of talus.
Valgus deformity with medial talar rotation that is so severe that patient bears weight on head of talus.
Varus foot deformities are seen in cavus foot types, cavovarus foot types, talipes equinovarus, and some neuromuscular conditions. The most common neuromuscular condition presenting with a varus deformity is Charcot-Marie-Tooth disease (see the images below). This deformity is also fairly easy to identify. The patient will have a heel that is in a varus position, an adducted forefoot, a higher-than-normal arch, and ankles that are storklike.
 Cavovarus deformity with high-arched foot. Note hammertoe deformity to all 5 digits common to this condition.
Cavovarus deformity with high-arched foot. Note hammertoe deformity to all 5 digits common to this condition.
 Triple arthrodesis. Cavovarus with high-arched foot, hammertoe deformity, adducted forefoot, and severely plantarflexed first metatarsal.
Triple arthrodesis. Cavovarus with high-arched foot, hammertoe deformity, adducted forefoot, and severely plantarflexed first metatarsal.
Outcomes
Outcomes are typically good, with high union rates of the TC and CC joints. The TN joint has the highest incidence of nonunion; however, the nonunion rate decreases with better understanding of the procedure and stable fixation. In a single-center retrospective study (N = 17; 18 feet; mean follow-up, 7.8 y) examining mid- to long-term results after triple arthrodesis, Maier et al cited a nonunion rate of approximately 11%. [8]
Degenerative changes at the unfused distal and proximal joints are still a long-term complication, but this is true with any fusion procedure. A study examining 400 triple arthrodesis procedures found less-than-perfect results in 24.5% of patients.
A period as long as 10 months is required for the patient to become pain-free. Return to high-impact activity is not a given. Lower-impact activities like walking, cycling, and swimming should be obtainable goals postoperatively.
-
CT scan of calcaneal fracture shows prominent lateral wall with heel rotated into varus.
-
Lateral wall blowout fracture with comminution. Note shortening and widening of heel. If left untreated, heel would remain in varus with uneven lateral wall and bony prominence that could become irritated.
-
Lateral wall blowout fracture with comminution. Note shortening and widening of heel. If left untreated, heel would remain in varus with uneven lateral wall and bony prominence that could become irritated.
-
Relatively mild calcaneal fracture still exhibiting shortening and widening.
-
Progression of talocalcaneal (subtalar) joint degenerative joint disease many years after calcaneal fracture with anatomic open reduction with internal fixation.
-
Medial arch collapse associated with valgus deformity.
-
Valgus foot deformity with medial dislocation of talar head. Note abducted forefoot and head of talus rotated medially on navicular.
-
Valgus foot deformity with medial dislocation of talar head. Note abducted forefoot and head of talus rotated medially on navicular.
-
Clinical view of valgus foot deformity with abducted forefoot and collapsed medial arch.
-
Valgus deformity with medial talar rotation that is so severe that patient bears weight on head of talus.
-
Varus foot deformity in patient with Charcot-Marie-Tooth disease.
-
Cavovarus deformity with high-arched foot. Note hammertoe deformity to all 5 digits common to this condition.
-
Triple arthrodesis. Cavovarus with high-arched foot, hammertoe deformity, adducted forefoot, and severely plantarflexed first metatarsal.
-
Cavovarus with high-arched foot, hammertoe deformity, adducted forefoot, and severely plantarflexed first metatarsal.
-
Osteophytes and degenerative joint disease easily seen at talonavicular, calcaneocuboid, and talocalcaneal (subtalar) joints.
-
Anteroposterior view depicting talonavicular and calcaneocuboid joints.
-
Articular surface on talar head rotated medially from concave articular surface of navicular. More than 7° of displacement is considered abnormal and is commonly found in valgus deformity with abduction of forefoot.
-
Harris-Beath projection allowing visualization of posterior facet of talocalcaneal (subtalar) joint and varus/valgus rotation.
-
Lateral view demonstrating talocalcaneal angle (yellow angle marker), talus first metatarsal angle (black angle marker), and calcaneal inclination angle (red angle marker).
-
Anteroposterior view demonstrating talocalcaneal angle (black angle marker), talus first metatarsal angle (red angle marker), and degree of talar head rotation from navicular (yellow marker).
-
Talocalcaneal (subtalar) joint injection via sinus tarsi.
-
Talocalcaneal (subtalar) joint injection via sinus tarsi.
-
Triple arthrodesis. Lateral incision is made from just inferior to distal tip of lateral malleolus to base of fourth metatarsal. This allows exposure to talocalcaneal (subtalar) joint, calcaneocuboid joint, and lateral portion of talonavicular joint. Care is taken to avoid branches of sural and superficial peroneal nerves running just inferior and superior to incision. This approach follows plane between nerves, but small branches may enter area and should be avoided if possible.
-
Triple arthrodesis. Anatomy of lateral incision: (A) lateral incision, (B) lateral malleolus, (C) base of fourth metatarsal, (D) base of fifth metatarsal, (E) peroneal tendons, (F) sural nerve, (G) intermediate dorsal cutaneous nerve.
-
Triple arthrodesis. Deep structures encountered through lateral incision: (A) Hoke tonsil before removal, (B) L-incision along insertion of extensor digitorum brevis (EDB) and across calcaneocuboid joint, (C) deep fascia over EDB.
-
Triple arthrodesis. (A) Extensor digitorum brevis elevated to expose (B) calcaneocuboid joint. (C) Hoke tonsil.
-
Triple arthrodesis. Exposure of (A) calcaneocuboid joint, (B) talocalcaneal (subtalar) joint, and lateral side of (C) talonavicular joint.
-
Triple arthrodesis. Medial incision is made beginning just anterior to distal tip of medial malleolus extending dorsomedially to naviculocuneiform joint. It lies between anterior and posterior tibial tendons. Saphenous vein and nerve are typically located slightly dorsal to incision and should be carefully retracted away during dissection.
-
Triple arthrodesis. Anatomy of medial incision: (A) medial incision, (B) medial malleolus, (C) posterior tibial tendon, (D) tibialis anterior tendon, (E) saphenous vein.
-
Triple arthrodesis. Dorsal exposure of talonavicular joint. (A) Talus. (B) Navicular.
-
Triple arthrodesis. Lateral view showing talocalcaneal (subtalar) joint arthrodesis with 7.3 cannulated screw going from talus to calcaneus.
-
Triple arthrodesis. Lateral view showing talocalcaneal (subtalar) joint arthrodesis using a 7.0 cannulated screw from calcaneus into talus.
-
Triple arthrodesis. Subchondral bone in joint with degenerative joint disease can be very sclerotic and hard. It may be wise to extend guide hole from near cortex in navicular all the way through talonavicular joint and into talus, even when using cannulated screws that are self-drilling and self-tapping. Corkscrew-appearing hardware represents threads from cannulated screw that delaminated off implant during attempt to cut through subchondral bone in talar head.
-
Triple arthrodesis. Talocalcaneal (subtalar) joint arthrodesis using 2 screws for fixation. This technique has increased in popularity owing to its added strength and rotational stability. Headless screws offer potential for less irritation.
-
Triple arthrodesis. Locking-compression plates have also gained in popularity, owing to their ease of placement, excellent strength, and impressive compressive force. Primary author has taken to using these almost exclusively for calcaneocuboid and talonavicular fixation and attributes them to early bone union and weightbearing.
-
Triple arthrodesis. Locking-compression plates.
-
Double arthrodesis of talonavicular and talocalcaneal (subtalar) joints. This procedure can be done entirely through medial incision and should be considered in severe valgus deformity where lateral skin breakdown is concern.







