Background
Arthroscopy is an important diagnostic and therapeutic technique for management of disorders of the joints. Ankle arthroscopy can be useful in treating a variety of intra-articular disorders, which may be caused by trauma or by degenerative, inflammatory, or neoplastic conditions. In some cases, the ankle-joint disorder may be related to extra-articular anomalies, which may be regional (eg, mechanical malalignment in the lower extremity) or systemic (eg, inflammatory arthritis).
As the indications for ankle arthroscopy have increased, so has its usage. The availability of modern arthroscopic instrumentation (eg, fiberoptics) and ankle distraction techniques has allowed orthopedic surgeons to manage a growing list of ankle disorders arthroscopically. Surgical procedures of the ankle performed arthroscopically are generally associated with lower morbidity, faster rehabilitation, and better cosmetic results as compared with conventional open surgical methods. [1, 2, 3, 4]
For example, management of osteochondral defects with autologous cartilage replacement has typically required an open procedure to suture a periosteal patch under which harvested and cultured cells are injected. With current techniques, however, the graft can be placed without the need for a periosteal flap and therefore can be implanted arthroscopically. [5]
It must be kept in mind that arthroscopy is not a panacea. For instance, whereas it can assist in reduction and internal fixation of ankle and pilon fractures, its role in the treatment of acute ankle fractures is still unclear. Ankle arthroscopy is also useful for treating syndesmosis disruptions, evaluating and treating posterior malleolar fractures of the tibial plafond, and facilitating removal of debris and reduction of talus fractures. Coincidental or concurrent osteochondral lesions can be managed with replacement of fragments or, if this is not feasible, microfracture surgery. Indications and applications for arthroscopy are still evolving and require further research.
Indications
Arthroscopy is indicated for definitive diagnosis of certain soft-tissue disorders when the exact etiology of ankle symptoms remains unclear, as well as for treatment of a variety of ankle disorders, usually after conservative measures have failed.
Indications for diagnostic ankle arthroscopy include the following:
-
Unexplained pain, swelling, stiffness, instability
-
Mechanical symptoms such as locking and popping
Indications for therapeutic ankle arthroscopy include the following:
-
Articular injury
-
Soft-tissue injury
-
Posttraumatic soft-tissue impingement
-
Bony impingement
-
Arthrofibrosis
-
Instability
-
Arthroscopic-assisted fracture fixation [6]
-
Synovitis
-
Loose bodies
-
Intra-articular bands
-
Tendinitis
-
Osteophytes
-
Osteochondral defects (see the image below)
-
Arthrodesis
-
Septic arthritis
Synovial inflammation and hypertrophy can result from various conditions, including inflammatory arthritis, infection, crystalline arthropathies, degenerative changes, trauma, and overuse. Pigmented villonodular synovitis (PVNS) is a benign synovial neoplasm that can be either generalized or local. Hemophiliacs often have synovial hypertrophy, and synovial impingement can lead to repeated ankle hemarthrosis.
Simple trauma, such as the common inversion injury of the ankle, after a single episode or multiple episodes, can lead to impingement of the superior portion of the anterior talofibular ligament.
Injury to the inferior tibiofibular syndesmosis can lead to tearing, scarring, and synovitis in the region of the anteroinferior tibiofibular ligament and impingement of this structure in the tibiofibular syndesmosis. Increased laxity resulting from torn ankle ligaments allows the talar dome to extrude anteriorly in dorsiflexion and cause soft-tissue impingement. [7]
Osteochondral lesions on the dome of the talus can result from acute trauma (eg, from an ankle sprain), degenerative changes, or repetitive trauma. About 10% of lesions are bilateral and are not associated with trauma. Traumatic lesions are mostly anterolateral in location, and degenerative lesions occur on the posteromedial aspect of the talus.
Loose bodies can be chondral or osteochondral in origin and usually result from trauma. They can also occur with synovial chondromatosis or synovial osteochondromatosis and can be free-floating or embedded in synovium or scar tissue.
Anterior osteophytes form over the anterior lip of the distal tibia and corresponding area of articulation on the dorsum of the neck of the talus. These osteophytes or spurs occur because of repetitive and forceful dorsiflexion. Football players and dancers have a high incidence of spurs.
After trauma or degeneration, wear and tear of the cartilage can be responsible for intra-articular adhesions, loose bodies, and osteophytes. In the late stages, most of the cartilage is denuded, exposing the subchondral bone and cysts.
Intra-articular injury is increasingly being recognized as associated with ankle fractures, but the role of ankle arthroscopy in the evaluation, treatment, and prevention of long-term sequelae is unclear. [8]
All of these conditions can benefit from arthroscopic intervention.
Contraindications
Absolute contraindications for ankle arthroscopy include the following:
-
Active local soft-tissue infection
-
Severe degenerative joint disease
-
Poor vascularity in the leg
Relative contraindications for ankle arthroscopy include the following:
-
Moderate degenerative joint disease
-
Severe edema
Technical Considerations
Anatomy
The ankle joint is a hinged synovial joint with primarily up-and-down movement (plantarflexion and dorsiflexion). However, when the ranges of motion of the ankle and subtalar joints are taken together, the complex functions as a universal joint. A thorough knowledge of the anatomy of the ankle joint, especially the contours of the articular surfaces and the neurovascular and tendinous structures in the surrounding soft tissue, is vital for planning and performing arthroscopy in this joint. [9, 10, 11]
Articular surface contours
The distal tibia is concave in the sagittal plane and convex in the coronal plane. The anterior tibial rim is mildly convex anteriorly and has a notch medially, where it recedes proximally by about 4-5 mm at the junction of the medial malleolus (see the images below).
The posterior tibial margin extends further distally than the anterior tibial margin by about 5-6 mm. The lateral malleolus extends further distally and is situated more posteriorly than the medial malleolus. The talofibular articulation slopes medially distally on a coronal plane. The fibular articular surface, in addition, is convex.
Topographic anatomy
About 6.5 cm proximal to the tip of the fibula, the superficial peroneal nerve divides into the intermediate and medial dorsal cutaneous branches. [12] In some individuals, these branches, especially the intermediate branch, can be made prominent under the skin by plantarflexion and supination of the foot (see the image below).
The intermediate dorsal cutaneous nerve passes superficial to the inferior extensor retinaculum and crosses the ankle joint lateral to the peroneus tertius tendon. The medial dorsal cutaneous branch courses over the lateral part of the extensor digitorum longus (EDL) tendon. These structures are subject to displacement if the joint is distended with fluid.
The deep peroneal nerve and the dorsalis pedis lie centrally in front of the ankle joint between the tibialis anterior and extensor hallucis longus (EHL) tendons.
The great saphenous vein (GSV) and the saphenous nerve run along the anterior border of the medial malleolus. The sural nerve and the small saphenous vein (SSV) are located posterolaterally between the lateral border of the Achilles tendon and the peroneal tendon.
The soft spot between the posterior aspect of the medial malleolus and the anterior margin of the Achilles tendon hosts some important structures. Posteromedial to the ankle and between the posterior margin of the medial malleolus and the Achilles tendon, proceeding from superficial to deep, course the posterior tibial tendon, the flexor digitorum longus (FDL) tendon, the tibial nerve and posterior tibial vessels, and the flexor hallucis longus (FHL) tendon.
The superficial medial calcaneal nerve originates from the posterior tibial nerve 2-3 cm proximal to the tip of the medial malleolus. It runs anteroinferiorly for 2.0-2.5 cm, away from the Achilles tendon, curving posteriorly and medially, dividing in several cutaneous branches at the calcaneal tuberosity.
All these structures are at risk of lesions from surgical intervention at the subcutaneous layer.
Arthroscopic anatomy
The borders of the lateral gutter of the ankle include the talus medially, the fibula laterally, and the tibia superiorly, bordered by the anteroinferior and posteroinferior tibiofibular ligaments. The anteroinferior section of the lateral gutter is bordered by the anterior talofibular, calcaneofibular, and anterior talocalcaneal ligaments. The posteroinferior borders are composed of the posterior talofibular, calcaneofibular, and posterior talocalcaneal ligaments. [13]
The posterolateral gutter structures include the posterior talofibular ligament, the posteroinferior tibiofibular ligament, the transverse tibiofibular ligament, the tibial slip, the FHL tendon, and a synovial nodule in the tibiofibular recess. The structures of the posteromedial gutter of the ankle include the FHL tendon and the deep portion of the deltoid ligament.
Outcomes
Outcome and prognosis vary, depending on the condition being managed. Good-to-excellent results have been reported at 2-year follow-up in as many as 84% of patients after arthroscopic management of anterolateral impingement. [14]
Persistent pain after an ankle sprain is often caused by the development of intra-articular fibrous scars or even tibiotalar spurs as a consequence of repetitive trauma. This may result in a posttraumatic impingement syndrome of the ankle. Pain is typically provoked by dorsiflexion of the ankle and palpation of the tibiotalar anterior joint space.
In a retrospective study evaluating 32 patients who underwent arthroscopy because of a grade I-III impingement syndrome of the ankle due to trauma without therapeutic response to conservative therapy over 3 months, ankle arthroscopy with resection of hypertrophic synovium and fibrous bands (type I) or tibial spurs (type II and III injuries) after an ankle sprain proved to be a reliable therapy for a posttraumatic impingement syndrome of the ankle that had not responded to conservative treatment. [15]
This approach was characterized by low morbidity and good-to-excellent results in most cases. [15] The outcome of arthroscopic treatment was related to the extent of chondral lesions. Diagnostic criteria included anterior ankle joint pain on palpation and pain provoked by dorsiflexion, in cases of grades II and III lesion spurs on the radiograph as well. The mean follow-up time was 49 months.
On the West Point Ankle Score, 26 patients had more than 80 points, corresponding to a good or excellent result (mean, 86 points; range, 80-98); their preoperative mean score was 64 (range, 57-70). [15] Of the remaining six, five had a fair postoperative result and one had a bad result (mean, 73 points; range, 62-78); their preoperative mean score was 56 point (range, 48-62). The fair and poor results were associated with severe ankle sprain leading to ligament ruptures or fractures where severe chondral lesions were to be found with arthroscopy.
In another study, arthroscopic resection of a torn portion of the interosseous ligament causing syndesmotic impingement successfully relieved symptoms in all 19 patients. [16]
In other studies, arthroscopic drilling of osteochondral defects in the talus yielded good-to-excellent results in 28-93% of patients. [17, 18, 19, 20]
A study that correlated the size of the lesion with results after arthroscopic microfracture treatment for osteochondral lesions of the ankle in 105 consecutive patients achieved excellent results for lesions smaller than 15 mm, regardless of location, at a mean follow-up of 31.6 ± 12.1 months. [21] Increased age, a higher body mass index (BMI), a history of trauma, and the presence of osteophytes negatively affected outcome. The presence of instability and anterolateral soft tissue scars was correlated with a successful outcome.
A prospective cohort study designed to evaluate whether residual degenerative cartilage at the lesions may obstruct the healing of the articular cartilage showed that in the treatment of osteochondral lesions of the talar dome, removal of the remaining degenerative cartilage may be of some therapeutic benefit. [22] A total of 39 patients underwent arthroscopic drilling that kept the remaining cartilage at the lesion, and 30 underwent arthroscopic drilling that removed the remaining cartilage at the lesion.
In a prospective, controlled trial, patients with symptomatic, recalcitrant Ferkel class 2b, 3, and 4 osteochondral lesions of the talus were randomly assigned to chondroplasty, microfracture, or osteochondral autologous transplantation (OAT) treatment groups; no differences were found between chondroplasty, microfracture, and OAT. [23] In all, 11 patients underwent chondroplasty, nine patients (10 ankles) underwent microfracture surgery, and 12 underwent OAT. Mean time to follow-up was 53 months (range, 24-119 months).
Arthroscopic ankle arthrodesis has shown good-to-excellent results in approximately 85-97% of patients, with a rapid fusion time, a low rate of nonunion, and few complications. [24, 25]
Leontaritis et al studied 84 ankle fractures (categorized according to the Lauge-Hansen criteria) that were treated with open reduction and internal fixation (ORIF) and for which ankle arthroscopy had been routinely performed in order to determine whether the severity of an acute ankle fracture was correlated with the number of arthroscopically detected intra-articular chondral lesions. [26] Chondral lesions were found in 61 patients (73%). The lesions were associated with individual fracture types as follows:
-
Fractures graded as pronation-external rotation or supination-external rotation type I (n = 17) - Fifteen were associated with one or no chondral lesion; two were associated with two or more chondral lesions
-
Fractures graded as pronation-external rotation or supination-external rotation type II (n = 10) - Nine were associated with one or no chondral lesion; one was associated with two or more chondral lesions
-
Fractures graded as pronation-external rotation or supination-external rotation type IV (n = 56) - Twenty-seven were associated with one or no chondral lesion; 29 were associated with two or more chondral lesions
The more severe ankle fracture patterns were found to be significantly more likely to be associated with two or more chondral lesions. [26]
Kunzler et al reported a case of synovial chondromatosis in a 54-year-old man leading to pain and limited range of motion in the ankle. [27] This unique case of extensive nodule formation was treated via a three-port arthroscopic approach. Removal of loose bodies and synovectomy were successfully performed arthroscopically. A total of 76 loose bodies were removed, and synovectomy was performed with a 3.5-mm diameter full-radius shaver. This case demonstrated that a three-port arthroscopic approach could provide adequate treatment while maintaining the superior risk profile inherent to arthroscopic intervention.
Bojanic et al reported on 17 patients who underwent combined posterior and anterior ankle arthroscopy within the same operative session and had histologically confirmed primary synovial chondromatosis (PSC) of the ankle. [28] In 14 patients, loose bodies were found in both compartments of the ankle; in two, only in the anterior compartment; and in one, only in the posterior compartment. In all 17, signs of synovial inflammation were evident in both compartments.
At final follow-up, [28] the median American Orthopaedic Foot and Ankle Society (AOFAS) Ankle-Hindfoot score had increased from 65 (range, 29-90) preoperatively to 95 (range, 65-100). Fourteen patients were extremely satisfied with the outcome, one was moderately satisfied, and two were dissatisfied. No recurrences of synovitis, loose-body formation, or signs of malignant transformation were noted. These findings led the authors to believe that ankle PSC should be regarded as a whole-joint disorder and felt that a combined posterior-anterior arthroscopic procedure within the same operative session should always be considered in patients with ankle PSC.
A retrospective study (N = 31; 18 male, 13 female; mean age 41.7 y; range 17-69 y) by Colasanti et al evaluated the clinical outcomes of in-office needle arthroscopy (IONA) for the treatment of anterior ankle impingement in the office setting and also assessed patient experience of IONA. [29] Patients were followed for a minimum of 12 months (mean, 15.5 mo). For outcome assessment, Foot and Ankle Outcome Scores (FAOS) and Patient-Reported Outcomes Measurement Information System (PROMIS) pain interference and pain intensity domains were obtained preoperatively and at final follow-up.
At final follow-up, the mean postoperative FAOS values were 79.4 for symptoms, 82.9 for pain, 83.5 for daily activities, 71.9 for sports activities, and 64.3 for quality of life. [29] Minimal clinically important differences were achieved for FAOS pain by 84% of patients, for FAOS symptoms by 77%, for FAOS quality of life by 75%, for FAOS sports by 74%, for PROMIS pain interference by 65%, for FAOS activities of daily living by 61%, and for PROMIS pain intensity by 42%. Of the 31 patients, 29 (94%) stated that they would be willing to undergo the same procedure again.
-
Intraoperative photo showing establishment of an anterolateral portal. The arthroscope is inserted into the anteromedial portal.
-
Cadaver dissection demonstrating the convex anterior aspect of distal tibial lip.
-
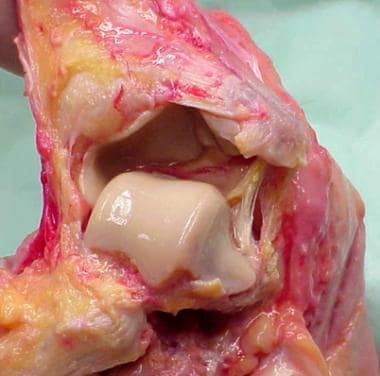
Cadaver specimen with dislocation of the ankle joint showing the contours of the talar dome.
-
Demonstration of branches of the superficial peroneal nerve.
-
Ankle stirrup attached to a distraction device fixed to the operating table.
-
Ankle distraction stirrup attached to a belt worn by the surgeon.
-
Joint distention before establishment of the anteromedial portal.
-
Arthroscopic view of a loose body.
-
Arthroscopic view of an osteochondral defect being punctured by an awl.
-
Arthroscopic view of an intra-articular band.
-
Arthroscopic view following debridement with an arthroscopic shaver of the intra-articular band seen in the figure above.