Background
Granular corneal dystrophy (GCD), an IC3D category 1 dystrophy, is an autosomal-dominant, bilateral, noninflammatory condition that results in deposition of discrete, irregularly shaped opacities in the cornea by adulthood. It specifically affects the middle portion of the cornea (stroma) and eventually can cause decreased vision and eye discomfort.
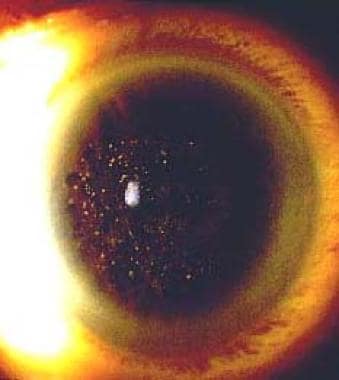
There are 2 clinically separate types: granular corneal dystrophy type 1 (classic type) and granular corneal dystrophy type 2 (Avellino corneal dystrophy), which tends to have fewer corneal deposits, potentially resembling a combination of lattice corneal dystrophy and granular corneal dystrophy. Severe cases of granular dystrophy can be treated with either excimer laser ablation or by replacing cornea (corneal transplant). An example is shown in the image below.
Pathophysiology
The cornea is the clear outer coat of the front of the eye. A dystrophy of the cornea is defined as a bilateral noninflammatory clouding of the cornea. Corneal dystrophies can be divided into 3 categories based on their location within the cornea, as follows: (1) anterior corneal dystrophies affect the corneal epithelium and may involve the Bowman layer, (2) stromal corneal dystrophies affect the central layer of cornea (the stroma), and (3) posterior corneal dystrophies involve the Descemet membrane and the endothelium. Granular corneal dystrophy is a stromal dystrophy, but the epithelium and Bowman layer may be affected in late disease.
The age of onset for most corneal dystrophies is before 20 years (exceptions include map-dot-fingerprint dystrophy and Fuchs corneal dystrophy). Most corneal dystrophies are inherited in a dominant pattern. Exceptions include macular corneal dystrophy, type-3 lattice dystrophy, and the autosomal-recessive form of congenital hereditary endothelial dystrophy.
Granular corneal dystrophy types I and II result from mutations in the TGFBI (BIGH3) gene. [1, 2] Depending on the specific mutation in the TGFBI gene, phenotypes of corneal dystrophy may differ. [3, 4] R124H and R555W are mutation hotspots of the TGFBI gene. [5, 6] The R124H mutation of TGFBI is highly correlated with granular corneal dystrophy type 2 (GCD2).
In a 2017 Chinese cohort study of 24 patients with clinically apparent granular corneal dystrophy, the R124H mutation was identified in 37.5% of cases; R555Q, 16.7%; R124L, 25%; R555W, 20.8%, and R124C, 0%. In 13 subjects with a positive family history of granular corneal dystrophy but no clinical signs of the disease, the mutation rate was 69.2%. [6]
Two 2017 studies demonstrated that granular corneal dystrophy type 22 corneal fibroblasts were more susceptible to oxidative stress–induced cell death than were wild-type cells, suggesting that oxidative stress is involved in the corneal pathogenesis of granular corneal dystrophy type 2. [7] Melatonin might have potential as a therapeutic agent by reducing endoplasmic reticulum (ER) stress. [8, 9]
Extinguishing or shortening of the meibomian glands was observed in patients with granular corneal dystrophy type 2. [10]
Epidemiology
Frequency
United States
Although granular corneal dystrophy type 2 is more common than granular corneal dystrophy type 1 in the United States, both are rare.
International
Granular corneal dystrophy is uncommon worldwide. Granular corneal dystrophy type 1 is more common in Europe, whereas granular corneal dystrophy type 2 is more prevalent in Japan, Korea, and the United States. [11]
Mortality/Morbidity
Corneal changes generally first become visible during the second decade of life, but vision may not be affected until the fourth to fifth decade of life. Eye pain from recurrent corneal erosions also can occur.
Sex
No sexual predilection has been reported.
Age
In granular corneal dystrophy type 1, corneal changes appear within the first decade of life but may not be visible until the second decade of life. [11] Visual acuity usually remains good until the fourth or fifth decade of life, once the opacities become confluent. Granular corneal dystrophy type 2 is usually diagnosed during early adulthood. [2]
Prognosis
The prognosis of granular corneal dystrophy is good, with symptomatic patients being eligible for either laser phototherapeutic keratectomy (PTK) or corneal transplant.
For granular corneal dystrophy type 1, recurrence occurred most rapidly after PTK (median, 2.7 years), deep anterior lamellar keratoplasty (DALK; median, 3.2 years), and anterior lamellar keratoplasty (ALK; median, 3.7 years). Recurrence was most delayed after penetrating keratoplasty (median, 13.7 years). All groups in this study achieved a similar median best corrected visual acuity (BCVA); 20/25-20/30). [12]
-
Granular dystrophy. Image courtesy of James J Reidy, MD, FACS, Associate Professor of Ophthalmology, State University of New York, School of Medicine & Biomedical Sciences, Buffalo, New York.
-
The slit lamp parallelipid demonstrates the deposition of opacities throughout the central stroma.