Practice Essentials
Giant papillary conjunctivitis (GPC), also called contact lens–induced papillary conjunctivitis (CLPC), is a common complication of contact lens wear. [1] First described by Spring, [2, 3, 4, 5] GPC is characterized by hypersensitivity-related inflammation of the ocular tarsal palpebral conjunctivae. [6] It is associated with the use of all types of contact lenses (eg, rigid, hydrogel, silicone hydrogel, piggyback, [7] scleral, prosthetic), [1] although similar reactions have been noted with ocular prostheses, extruding scleral buckles, exposed ocular sutures, and even elevated corneal scars.
GPC once was considered an allergic disease similar to other immunoglobulin E (IgE)–mediated ocular allergy such as allergic conjunctivitis and vernal keratoconjunctivitis because of the similar clinical symptoms seen in allergic diseases (eg, itchiness, tearing, mucous hyperproduction, increase in symptoms during allergy season). The mechanical irritation of contact lenses and sutures that causes GPC supports the classification of GPC into a group of nonallergic hypersensitivity disorders. [1, 8]
Background
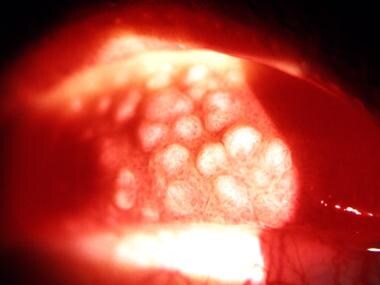
Initially, small papillae coalesce with expanding internal collections of inflammatory cells. When the lesions reach diameters of more than 0.3 mm, often approaching or exceeding 1 mm, the condition is referred to as GPC. Images of eyelid papillae appear below.
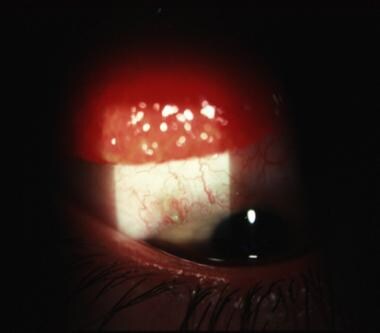 Giant papillary conjunctivitis (GPC) response (slightly out of focus) seen in the upper lid of a young patient recovering from cataract extraction with an exposed suture barb (in focus).
Giant papillary conjunctivitis (GPC) response (slightly out of focus) seen in the upper lid of a young patient recovering from cataract extraction with an exposed suture barb (in focus).
Because of the high prevalence of GPC among contact lens wearers, GPC should be considered in every patient with characteristic symptoms who wears contact lenses.
See the following for more information:
Etiology
The antigen(s) responsible for GPC have yet to be identified. From circumstantial evidence, the initiating event is believed to be mechanical irritation and/or antigenic stimulus of the tarsal conjunctiva of the upper lids by a contact lens surface or edge (rigid or flexible) or deposit. Histologic changes in the tissue occur with mast cell degranulation and a secondary inflammatory cascade. This leads to conjunctivitis and further tissue changes with increasing inflammatory markers in the tears.
GPC can be caused by all forms of ocular prostheses, including rigid and hydrogel (soft) contact lenses, prosthetic eyes, extruding scleral buckles, exposed portions of sutures, filters, knots, and even corneal scars. [9] Heat sterilization, poor cleaning, thick or rough contact lens edges, and extended wearing times also predispose to the development of GPC.
Lipid and protein deposits from the tears, as well as debris coating the surface of contact lenses, also may lead to a spiral of inflammation. This, in turn, causes even more lens deposits to form, leading to additional inflammation. [2, 3, 4] The level of coating on the lenses varies among individuals and the polymer of the contact lenses.
High-water hydrogel (HEMA) contact lenses tend to coat more than lower-water HEMA contact lenses. Silicone contact lenses tend to accumulate more lipid deposits than HEMA lenses. First-generation silicone hydrogel contact lenses may be more prone to GPC development, perhaps because of their mechanical stiffness or their higher propensity for lipid deposition. Silicone hydrogel lenses tend to induce more local GPC (similar to the changes seen with rigid lenses), whereas hydrogel lenses tend to induce more generalized GPC reactions in the palpebral conjunctiva. [10]
GPC may be more severe in patients with atopy. [4]
Epidemiology
The incidence rate varies ranging between 1.2% to 36% [11, 12, 13] as influenced by CL type, frequency of CL disposability, CL wear time, CL hygiene, and CL fit. The prevalence of GPC is highest among wearers of hydrogel contact lenses—approximately 27%, [12] whereas rigid gas-permeable contact lens wearers constitute approximately 10% of all cases. [12] With an increased frequency of contact lens replacement from more than 4 weeks to less than 4 weeks, the incidence of GPC has dropped from 36% to 4.5%. [14] The incidence of GPC in patients wearing one-day disposable contact lenses was significantly lower (7.4%) than those wearing monthly contact lenses (17.0%). [15] The international prevalence of GPC is similar to that in the United States.
Both sexes develop GPC.
GPC can be more aggressive in children who wear contact lenses.
Prognosis
The prognosis of GPC is good. Approximately 80% of patients can return to comfortable contact lens wear with appropriate treatment. [14]
GPC has been a common cause of temporary and permanent contact lens intolerance. It also can cause ptosis of the upper lids.
The lids of some patients return to normal appearance following the resolution of GPC, whereas other lids retain small, white, capped scars of the giant papillary lesions for long periods, sometimes indefinitely.
GPC is not associated with mortality.
Patient Education
Patients should be educated about appropriate contact lens cleaning and follow-up care. Regular professional evaluations (perhaps once or twice a year in the absence of other complications) and additional appointments are recommended if they experience any increasing ocular itching, mucous discharge, or dirty contact lenses.
Patients should be educated about the chronic nature of GPC and its symptoms (eg, ocular itch, mucous discharge, contact lens intolerance). Patients should be counseled to present within a week of any relapsing symptoms.
For patient education information, see the Eye and Vision Center, as well as Pinkeye and Contact Lenses.
-
Very large papillae in the everted upper lid of a patient who wears hydrogel (soft) contact lenses.
-
Giant papillary conjunctivitis (GPC) response (slightly out of focus) seen in the upper lid of a young patient recovering from cataract extraction with an exposed suture barb (in focus).