Background
Laser-assisted subepithelial keratectomy (LASEK) is a laser surgical procedure for the correction of refractive error. LASEK is specifically used to correct astigmatism, hyperopia (farsightedness), and myopia (nearsightedness). It is a "hybrid" technique between laser assisted in situ keratomileusis (LASIK) and photorefractive keratectomy (PRK). The LASEK technique attempts to decrease the occurrence of flap-related complications associated with LASIK and, as in PRK, is specifically helpful in patients with corneas that are otherwise too thin for LASIK. By retaining a flap of corneal epithelium, LASEK may decrease the risk of infection and incidence of corneal haze, while reducing recovery time and postoperative discomfort when compared with PRK.
History of the Procedure
Concepts of corneal refractive surgery, such as keratectomy, keratotomy, and thermokeratoplasty, were first described in 1898 by Lans who published a set of experiments that focused on treating astigmatism in rabbits.
Refractive surgery, as it is known today, was not realized until 1966 when Pureskin first appreciated its potential with the demonstration that refractive changes could be made by removing central tissue underneath a corneal flap. Barraquer later showed that the corneal disc could be resected and frozen so that it could be reshaped using a cryolathe; however, his technique used complex equipment and had high intraoperative and postoperative complication rates, and the freezing resulted in damage to the disc itself.
In the late 1980s, Ruiz and Barraquer performed the first published keratomileusis in situ. They followed principles formulated by Krumeich using a microkeratome to remove a portion of the cornea followed by a second plano cut, the thickness and diameter of which established refractive change. The first disc was then repositioned and sutured back onto the cornea. These initial attempts were complex and unpredictable, often leading to keratoconus and other irregular astigmatisms.
Burratto and Pallikaris then combined the microkeratome technique with the use of the excimer laser to ablate tissue and to induce refractive change. Buratto performed excimer laser ablation on the posterior surface of the resected corneal disc before replacing and resuturing it back to its original position. Pallikaris then used the excimer laser ablation on the corneal stromal bed under a hinged flap in rabbit corneas. Pallikaris attempted this technique on blind human eyes in 1989 and on sighted human eyes in 1991, thereby creating a refractive surgical technique similar to the procedures currently in practice.
In 1993, Slade developed an automated microkeratome to refine the creation of the flap. Slade was one of the first surgeons to perform LASIK in the United States.
Since its introduction, LASIK has been associated with various complications, specifically when performed on eyes with decreased corneal thickness, irregular astigmatism, dryness, preexisting ocular surface disease, or glaucoma, to the point where several of these entities have become relative contraindications to performing LASIK. For these reasons, LASEK was developed to reduce the chance of complications that occur secondary to LASIK while inducing less discomfort than PRK.
Italian ophthalmologist Camellin is credited with developing the original LASEK procedure when he described the Camellin technique in ophthalmic literature in 1999. This technique involved the use of alcohol to separate the corneal epithelium from the stroma to create an epithelial sheet that could be repositioned over the ablated stroma. Since then, this method has evolved into multiple techniques, including Butterfly LASEK developed by Vinciguerra and Camesasca in 2002, cruciform LASEK described by Amolis in 2002, and gel-assisted LASEK created by McDonald in 2004. [1] Each of these techniques is described in Intraoperative details.
Problem
Ocular refraction is defined as the ability of the eye to bend light rays to focus them on the retina. The cornea, the lens, and the axial length of the eye are the main contributors to the eye's refraction capability. The total refractive power of an emmetropic (or normal length) eye is approximately 58 diopters (D), of which 43 D come from the cornea and the remaining 15 D from the lens, aqueous, and vitreous. Astigmatism, myopia (nearsightedness), and hyperopia (farsightedness) are common forms of refractive error that cause irregularities of the bending of light rays, thereby leading to blurred or distorted vision.
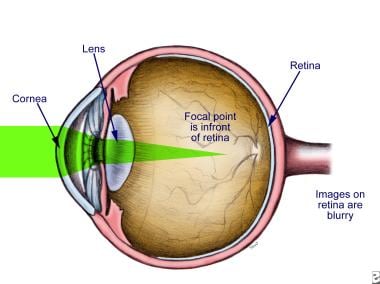
Myopia (nearsightedness) is a condition in which the eye is too long or the refractive power is too great, causing objects to focus at a point before the retina rather than upon the retina itself.
This inability to focus appropriately leads to an inability to see distant objects clearly. This problem tends to first appear in school-aged children and may progress through adolescence but usually stabilizes in early adulthood.
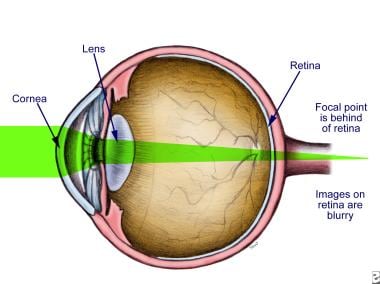
In hyperopia (farsightedness), the eye is too short or the cornea is too flat, so that parallel light rays come to focus behind the retina in the unaccommodated state.
This irregularity causes an inability of the eye to bring near objects into clear focus because light entering the eye focuses behind the retina rather than directly on it. Because younger individuals may accommodate (or adjust) to focus near objects, the blurred vision associated with hyperopia is often not appreciated until later years as the eye loses this ability to accommodate.
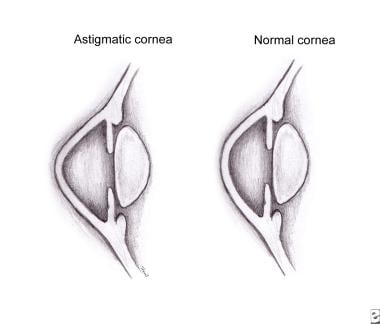
In astigmatism, the refractive power of the eye is not the same in all meridians.
For example, the eye may exhibit more myopia horizontally than vertically. In the diagram above, the astimatic corneal profile shows steeper curvature compared to the flatter curve in the perpendicular "normal" meridian. Most corneas have some degree of curvature asymmetry resulting in "regular" astigmatism.
Epidemiology
Frequency
Astigmatism, myopia, and hyperopia are relatively common in the general population. Myopia and hyperopia have an estimated prevalence of 33% and 25%, respectively. The prevalence of astigmatism varies with the definition used as clinically significant astigmatism. As many as 75% of the population has at least minor, clinically insignificant astigmatism present in either one eye or both eyes. Specifically, in the general population, 44% have greater than 0.50 D, 10% have greater than 1 D, and 8% have greater than 1.50 D.
A refractive surgery survey conducted in 2004 regarding 2003 practices identified LASIK as the most common refractive surgical procedure, with wavefront-guided ablation as an increasingly popular entity, increasing from 13% to 60% during 2002-2003 alone. Of the more than 1000 ophthalmologists who participated in this retrospective study, 71% were found to perform PRK, and 41% were found to perform LASEK. Of those ophthalmologists who performed LASEK, more than one half only performed this procedure when LASIK was not an option.
Another survey focused on the refractive surgery practices of the United States Army Warfighter Refractive Eye Surgery Program (WRESP) during 2000-2003. Of the more than 16,000 patients over these 4 years, nearly three quarters of cases involved surface ablative procedures, namely PRK or LASEK. PRK was performed on 64.7% of eyes, LASEK was performed on 8.7% of eyes, and LASIK procedures were performed on the remaining 26.6% of eyes.
Indications
The major indications for refractive surgery include astigmatism, myopia, and hyperopia, specifically in patients who are intolerant of or who desire to be free from glasses or contact lenses. Typically, up to 10 D of myopia and 4 D of hyperopia are the limits of corneal refractive surgery, but the US Food and Drug Administration (FDA) has approved treatment of as much as 14 D of myopia, 6 D of hyperopia, and 6 D of cylinder.
Since the popularization of laser-assisted in situ keratomileusis (LASIK), surface ablative procedures, such as photorefractive keratectomy (PRK) and laser-assisted subepithelial keratectomy (LASEK), have usually been confined to individuals in whom LASIK is not recommended. However, due to the potential structural and other advantages of surface procedures, there are now many ophthalmologists who suggest surface procedures over LASIK, or who will endorse both equally. The characteristics that may prompt an ophthalmologist to recommend surface ablation over LASIK include the following:
-
Thin corneal pachymetry
-
Steep or flat corneas
-
Wide scotopic pupil (controversial) [2]
-
LASIK complications in fellow eye
-
Predisposition to trauma
-
Irregular astigmatism
-
Persistent epithelial infiltrates (typically related to soft contact lens wear or prior viral conjunctivitis)
-
Early Fuchs endothelial dystrophy, when there is good visual potential but flap adherence may be impaired due to stromal edema
Highly irregular astigmatism, specifically keratoconus, as well as severe dry eye syndrome can serve as contraindications to LASEK as well as to LASIK.
Relevant Anatomy
The cornea accounts for two thirds of the refractive power that acts to focus light rays on the back of the eye. Of this, approximately 80% of the refractive power is created by the air-tear interface. Average cornea diameter is approximately 11 mm vertically and 12 mm horizontally.
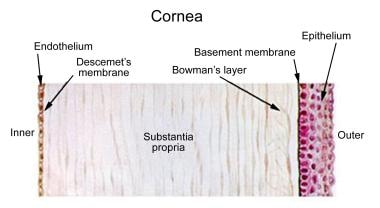
The cornea consists of 6 layers. From superficial to deep, these layers are the corneal epithelium, Bowman’s layer, the stroma, Dua's layer, Descemet's membrane, and the endothelium.
The corneal epithelium consists of 5-7 layers of stratified squamous epithelium. Defects in this layer may cause severe pain secondary to the rich sensory innervation. Fortunately, damage to the epithelium is quickly repaired in healthy eyes. The Bowman layer, on the other hand, is not replaced after injury, and this tough layer of collagen fibers may become opacified and replaced by scar tissue after trauma. The stroma makes up about 500 µm (90%) of the average 550-µm central corneal thickness. Its 200-250 lamellae (flattened bundles of collagen) give the cornea its clarity, strength, and shape. The lamellae are produced by scattered stromal fibroblasts or keratocytes. Keratocytes are also responsible for wound healing if the cornea becomes damaged. A newly discovered layer of the cornea, Dua's layer is found between the posterior stroma and Descemet'e layer [3] .
The Descemet membrane serves as the acellular basement membrane of the corneal endothelium. Like the Bowman layer, it is not replaced after injury and may result in scar formation. The deepest layer of the cornea is a monolayer of endothelial cells whose primary function is the maintenance of corneal fluid balance, thereby maintaining clarity across the cornea. Unlike the epithelium, these cells rarely undergo mitosis and instead decrease in number with age. See the images below for illustration of the layers of the cornea and corneal topography.
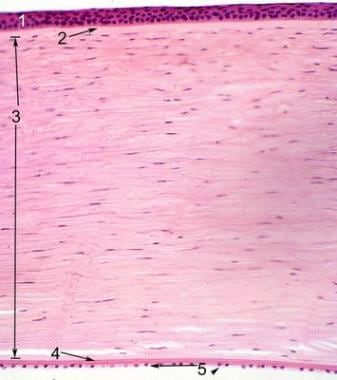 Histologic slide of the human cornea identifying its layers: (1) corneal stratified squamous epithelium with underlying Bowman layer, (2) stroma with keratocytes dispersed throughout, (3) Descemet membrane, and (4) single layer of endothelium. Image courtesy of Mission for Vision. Retrieved from http://www.missionforvisionusa.org/anatomy/2005/10/cornea.html.
Histologic slide of the human cornea identifying its layers: (1) corneal stratified squamous epithelium with underlying Bowman layer, (2) stroma with keratocytes dispersed throughout, (3) Descemet membrane, and (4) single layer of endothelium. Image courtesy of Mission for Vision. Retrieved from http://www.missionforvisionusa.org/anatomy/2005/10/cornea.html.
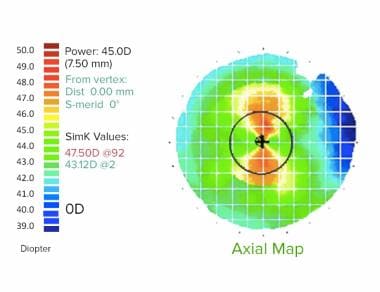 Example of placido based corneal topography. This image depicts a large quantity of “with-the-rule” corneal astigmatism. The warmer colors represent steeper areas and the cooler colors represent flatter areas of the cornea. This illustration demonstrates symmetric steepness along the vertical meridian and relative flattening along the horizontal meridian.
Example of placido based corneal topography. This image depicts a large quantity of “with-the-rule” corneal astigmatism. The warmer colors represent steeper areas and the cooler colors represent flatter areas of the cornea. This illustration demonstrates symmetric steepness along the vertical meridian and relative flattening along the horizontal meridian.
Contraindications
Contraindications common to laser assisted in situ keratomileusis (LASIK), laser assisted subepithelial keratectomy (LASEK), and photorefractive keratectomy (PRK) include the following:
-
Unstable refractive error
-
Refractive error outside the range of correction (The range varies according to the surgeon's experience, the laser used, and the laser strategy; however, it is typically approximately 9-14 D of myopia, 4-6 D of hyperopia, and 2-6 D of astigmatism.)
-
Keratoconus or forme fruste keratoconus
-
Significant dry eye syndrome
-
Active inflammation of external eye
-
Autoimmune disease
-
History of or active herpes simplex keratitis, because of the concern of eliciting reactivation of the virus
-
Active collagen vascular disease
-
Uncontrolled diabetes
-
Uncontrolled glaucoma
-
Pregnancy or breastfeeding
-
Use of medications that may adversely affect corneal wound healing, such as Accutane (isotretinoin), Cordarone (amiodarone hydrochloride), and Imitrex (sumatriptan)
-
Presence of a pacemaker
Contraindications unique to LASEK and PRK include the following:
-
Concern regarding postoperative pain
-
Requirement of rapid visual recovery
Patients with thin, flat, or steep corneas may be better candidates for LASEK and PRK than for LASIK
-
Illustration of myopia.
-
Illustration of hyperopia.
-
Illustration of an astigmatic cornea.
-
Illustration depicting the layers of the human cornea.
-
Histologic slide of the human cornea identifying its layers: (1) corneal stratified squamous epithelium with underlying Bowman layer, (2) stroma with keratocytes dispersed throughout, (3) Descemet membrane, and (4) single layer of endothelium. Image courtesy of Mission for Vision. Retrieved from http://www.missionforvisionusa.org/anatomy/2005/10/cornea.html.
-
Example of placido based corneal topography. This image depicts a large quantity of “with-the-rule” corneal astigmatism. The warmer colors represent steeper areas and the cooler colors represent flatter areas of the cornea. This illustration demonstrates symmetric steepness along the vertical meridian and relative flattening along the horizontal meridian.
-
This image depicts the epithelial flap of a porcine eye as it is folded along its hinge to reveal the surface for laser ablation. Image courtesy of Ronald R. Krueger, MD, Cole Eye Institute, The Cleveland Clinic Foundation.
-
This image, taken intraoperatively on a rabbit eye, depicts the creation of the epithelial flap using the microkeratome. Image courtesy of Ronald R. Krueger, MD, Cole Eye Institute, The Cleveland Clinic Foundation.
-
This image depicts the epithelial flap created in laser assisted subepithelial keratectomy (LASEK) surgery on a rabbit eye. Image courtesy of Ronald R. Krueger, MD, Cole Eye Institute, The Cleveland Clinic Foundation.
-
Image of corneal haze following refractive surgery, as viewed through a slit lamp. Image courtesy of Ronald R. Krueger, MD, Cole Eye Institute, The Cleveland Clinic Foundation.
-
Relative differences of laser assisted in situ keratomileusis (LASIK), laser assisted subepithelial keratectomy (LASEK), and photorefractive keratectomy (PRK). Adapted from Taneri S, et al: Evolution, techniques, clinical outcomes, and pathophysiology of LASEK: review of the literature. Surv Ophthalmol 2004 Nov-Dec; 49(6): 576-602.