Overview
Low vision is a general term that refers to a permanent functional vision loss that cannot be corrected by medication, surgery, or glasses. Low vision patients may experience a wide array of diseases, field defects, and degrees of vision loss. However, in general, low vision can be defined as a bilateral decrement to visual acuity or visual field resulting from a disruption of the visual system. This decreased acuity or field results in an impaired ability to perform work, leisure, or daily living activities. It is already known that low vision in adults does impair quality of life, and one study demonstrates that children with visual impairment had significantly lower quality of life scores than an age-matched comparison group using the Low Vision Quality of Life Questionnaire. This research reinforces the need for low vision services for children. [1, 2, 3]
A low vision examination should detail the kinds and the quality of visual deficits afflicting patients and how they are adapting to their vision loss. This may include a chief complaint, as well as social, functional, and ocular health history. A low vision examination should detail the kinds and the quality of visual deficits afflicting patients and how they are adapting to their vision loss. This may include a chief complaint, as well as social, functional, and ocular health history. The low vision functional history includes details of a patient’s visual challenges and goals for work, leisure and activities of daily living (ADLs). The occupational needs assessment is detailed to discuss technology and mobility requirements of the job, as well as travel to and from work. The activities of daily living explore hobbies, and access to technology such as cell phone, tablet or computer. Other tasks such as meal preparation and self-care (grooming, taking medications) are discussed. The social history includes living situation challenges such as stairs, as well as assistance available and the patient’s household responsibilities. [4]
Low vision acuity and refraction often requires such nonstandard acuity measures as the Feinbloom low vision chart with numerals in the size range of Snellen 700 to 10. Distance acuity often is measured at varying distances (eg, 10 ft, 5 ft). Trial lens refraction is recommended to ensure accurate vertex distance to allow for eccentric eye or head position.
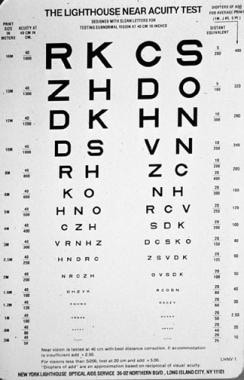
Near acuity is measured at 40 cm (ie, 0.40 m) with the patient's correction in place, with +2.50 D add if the patient is presbyopic. The add power needed to read average size print (ie, 1 M, 20/50 Snellen equivalent, Jaeger #5) is calculated by taking the reciprocal of the near acuity. For example, a patient reading 4 M print (20/200 Snellen equivalent) at 40 cm would require a +10 diopter (D) add to read 1 M print (1/0.40 m/4 M).
One option to speed up the add calculation is to use the Lighthouse Near Acuity Test chart (at 40 cm test distance), which includes precalculated adds for each acuity. To determine the necessary magnification, divide the best-corrected acuity by the desired acuity. For example, the best-corrected acuity is 20/200 and the desired level of acuity is 20/40, so the required magnification is 5 X (200/40).
Visual field
Goldmann visual field testing provides information regarding peripheral fields to 180 degrees. This test is needed when testing for driving. The Humphrey field analyzer can go to 60 degrees for details information about central fields. On the other hand, an Amsler grid is used to map out a central scotoma for patients with central vision loss from macular degeneration, macular edema, etc. Another test is now available for central fields called the California Central Visual Field test, which can more precisely map out scotomas. The results of the central vision tests help in rehabilitation using a peripheral retinal locus. In other words, the patient may use eccentric viewing to find the clearest image.
Contrast sensitivity
Contrast can be tested using the ETDRS low contrast acuity chart or the Pelli Robson contrast sensitivity chart. In low vision, the Pelli Robson chart is preferred because it separates contrast from acuity: all letters are the same size but in decreasing contrast order. The patient reads the chart and is scored by the last 2 of 3 correct in a given contrast level. The test may be performed monocularly to follow disease progression, or binocularly to predict functional vision deficits. Patients with poor contrast sensitivity have difficulty recognizing faces, seeing the edges of curbs and steps and seeing details with sub-optimal lighting conditions.
Task lighting
Lux IQ test allows patients to choose the brightness (Lux) and warmth of color (degrees Kelvin) for optimal task lighting. The subjective lighting levels may be entered in the Lightchooser website to give up to date suggestions of lamps and bulbs.
In summary, functional vision analysis for each patient includes visual acuity for distance and near, visual field, contrast sensitivity and perhaps color vision, and optimal task lighting preferences. Each patient is unique in functional vision loss. One patient may only have blurred vision while another has bothersome scotomas or faded vision (contrast sensitivity loss). Understanding how each patient sees enables us to provide tools to meet each patient’s goals.
Above photos show normal view, reduced visual field view, and blurred with reduced contrast view. Each patient may differ in their functional vision measures of acuity, visual field, or contrast sensitivity.
The goal of low vision rehabilitation services is to optimize the use of functional vision to the best of the patient’s ability. Success is when a patient can achieve his or her goals in accomplishing a task. The rehabilitation plan may include magnification, enhanced contrast, task lighting, colored filters, computer/cell phone adaptations and even text to speech options.
Low Vision therapy may include services from an optometrist providing optical and electronic devices, an occupational therapist providing adaptive equipment/techniques to promote success in activities of daily living, and an orientation and mobility instructor for navigating safely/white cane training. Some patients may also need referrals for psychological services when coping with vision loss is a struggle.
Indications
Various forms of low vision therapy can increase the patient's ability to perform work, leisure, or daily living activities.
Equipment
Equipment in low-vision therapy is as follows [5, 6, 7] :
-
Near aids - Readers, microscopes, handheld magnifiers, stand magnifiers
-
Closed-circuit televisions
-
Computer programs, tablets, or large monitors
-
Distance aids - Telescopes, sunglasses
-
Aids for daily living and eccentric viewing - Adaptive equipment, eccentric viewing training, contrast
-
Optical prosthetic device
Technique
Near optical aids
Readers
In patients with low-to-moderate vision loss, the near acuity often can be improved by increasing the bifocal add alone. However, bifocal powers greater than +5.00 D may impede mobility. Hence, separate glasses with a more moderate add may be necessary, in addition to the high-powered readers. Also, demonstrating the reduced focal distance (closer working distance) of high-add prescriptions helps to educate patients so that they know exactly at what distance the reading material should be held.
Excess convergence demanded by add powers greater than +4.00 D can be relieved by the use of a base-in prism, 2 more than the diopteric power of the add per eye. For example, +6.00 D glasses would have 8 prism diopters base-in for both eyes. Standard prism half glasses without astigmatism are available in +4, +5, +6, +8, +10, and +12 D powers.
Predicting reading Add
Magnification ratio = Present Acuity/Desired Acuity = letter size can read/letter size wants to read
Predicted Add= mag ratio x current reference add
Example: Patient’s acuity is OD 4M, OS 6M using her glasses with +3.00 add, goal is to read 1M size font
Using better eye at 4M and goal of 1M, Magnification needed equals ability/goal, 4/1 = 4x or 4 times as big
Predicted add= 4x3= +12 add
(This is usually done in M notation with 1M newspaper as a common goal. You can also use near Snellen denominator if you don’t have an M near card)
Optimal illumination with the light source directed at an angle of 45° to the page, and over the shoulder of the better eye, minimizes glare. The advantage of high-add readers is that they leave hands free and are familiar to patients. The primary disadvantage of these readers is the need to train patients to use a much closer reading distance.
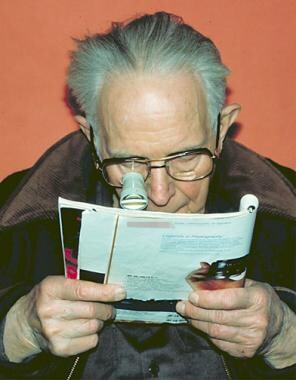
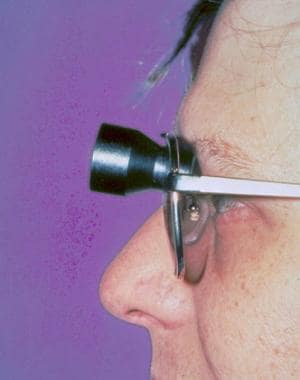
Microscopes and near telescopes
Microscopes typically are used when the needed add power is greater than 12 D. Because of the greatly reduced focal length, microscopes often are prescribed monocularly (see image below). [8]
In contrast, near telescopes allow the patient to read at a more natural working distance. Near telescopes, like surgical telescopes, have a narrow field of view, but they can be manufactured to focus at any working distance. However, good motor control is essential to maintain the reading material within the field of view. [8]
Handheld magnifiers
To achieve full magnification, handheld magnifiers should be demonstrated with the patient's distance correction in place. The demonstration should begin by placing the magnifier on the page and, then, slowly raising it until the image is at the maximum magnification.
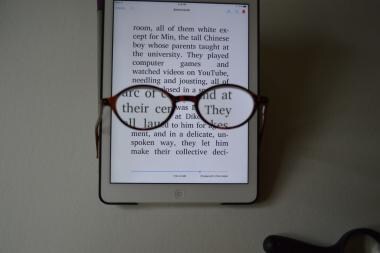
Although handheld magnifiers provide greater magnification than high-add readers and allow for a greater reading distance than microscopes, they require good motor control to be used effectively. Hence, handheld magnifiers often are suggested for short-term reading tasks, such as checking prices in a store or reading items on a menu. [8]
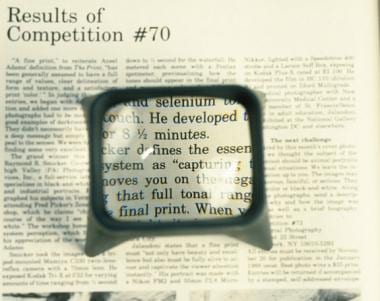
Stand magnifiers
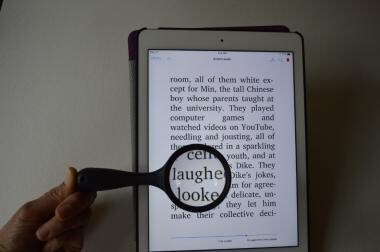
Stand magnifiers are similar to handheld magnifiers, but they have a base that is used to rest the magnifier on the reading page (see image below). Stand magnifiers require less motor control than handheld magnifiers and allow for a greater working distance than high-add reading glasses. Moreover, illuminated stand magnifiers can provide the patient with direct illumination of the reading material.
Fixed-focus stand magnifiers are designed to be viewed at a distance of 40 cm and require a reading add to bring the image into focus. Patients often may wish to use a greater add power than the standard +2.50 D to reduce the working distance and to gain a wider field of view. They provide the clearest image when the patient sights the object on axis. An off-axis view of the object through the magnifiers often produces a distorted image and results in reduced reading facility.
If the patient desires to write or sew under the magnifier and has only moderately impaired vision, then an illuminated stand magnifier mounted on a flexible arm can be used. One such device is the big eye magnifier with a +3.00 D or +6.00 D lens.
Stand magnifiers are especially useful for patients who have glaucoma or retinitis pigmentosa with restricted visual field. For such patients, the reduced field of view provided by the stand magnifier often results in better scanning skills while reading.
The 2 most common reasons for patients to reject these devices are postural fatigue from having to bend over the magnifier and difficulty with manual manipulation of the magnifier. Although practice makes the device more manageable and an adjustable light source with clipboard can improve the posture, patients may prefer the larger field of view provided by closed-circuit televisions (CCTVs) when reading for an extended period of time. [8]
Distance optical aids
Telescopes
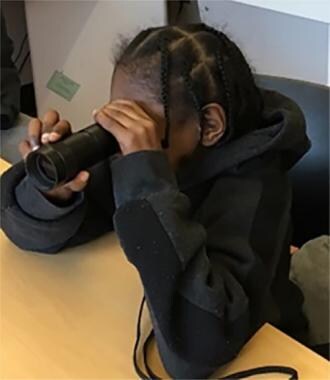
Telescopes are typically in clear focus for objects viewed from a distance of 20 feet or more. The doctor should prefocus the telescope on a distant object. The telescope should be aligned by focusing a penlight beam through the telescope onto the patient's pupil. The lowest possible magnification should be chosen to meet the patient's needs, thereby keeping the field of view at a maximum. The patient should wear the prescribed correction or have it placed within the lens of the telescope.
Improvements in telescopic systems include the ability to adjust for distance, intermediate, and near vision. Furthermore, increased fields of view and decreased weight allow patients to increase their reading duration and rate.
Hand-held telescopes are useful for short-term spotting tasks. They are small and inconspicuous and often are prescribed monocularly. [8]
Clip-on telescopes are usually monocular. They are useful when patients need their hands to be free. Patching the other eye is helpful when learning how to see with a clip-on telescope.
Spectacle-mounted telescopes are made by cutting out a hole in the conventional lenses and inserting a telescope. The telescopes may be mounted in a central position or in a high position (bioptic position). They are best made with the patient's prescription in the telescope lens. Patients view through the conventional lens most of the time and tip their heads down to look through the telescope only when magnification is needed. In some states, they can be used to pass the acuity portion of the driver’s license test. They are useful for long-term distance tasks, such as watching sporting events or bird watching. [8]
Using a handheld monocular telescope
Sunglasses
Sunglasses are used to reduce the symptoms of glare and photosensitivity.
Corning SPF series are useful, especially for patients with macular degeneration, ocular albinism, and glaucoma. They are more costly than the other forms of sunlight protection.
Unlike conventional sunglasses, the top and sides of NOIR sunglasses shield the patient from excess light. NOIR sunglasses are available in many hues. Several companies suchs as Eschenbach and Chadwick offer custom tints in many colors and light blocking intensities.
Combining Optical Correction and Technology
Current technologic options are aimed at universal accessibility: reading or listening in variously sized fonts or volumes. This concept, in which a person with 20/20 vision may want to listen to a book in the car or use email while walking on a treadmill, has led to a surge in tablets, monitors, computer programs, and applications that assist all in accessing information and communication. While optical correction such as higher-power prism readers or handheld magnifiers are still used, lenses can now be combined with larger or contrast-enhanced font presentation.
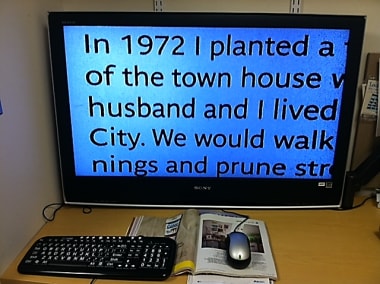
A computer may be plugged into a large monitor, such as in a 42-inch television. The text on the screen is 3 times larger even before adding computer program enhancement such as Zoomtext or other enlarging enhancing software options. Appropriate reading glasses may be added, with a net add of +2.00 D for 0.5-meter viewing distance or a net add of +1.50 D for 0.66-meter viewing distance.
 Large monitor. A computer may be plugged into a large monitor, such as in the 42-inch television pictured. The text on the screen is 3 times larger even before adding computer program enhancement such as Zoomtext or other enlarging enhancing software options.
Large monitor. A computer may be plugged into a large monitor, such as in the 42-inch television pictured. The text on the screen is 3 times larger even before adding computer program enhancement such as Zoomtext or other enlarging enhancing software options.
One of the most reasonably priced options for electronic magnification is the portable electronic reading aid by Mattingly. The pinhole style camera is plugged into the patient’s home television. Zoom magnification is available, along with enhanced contrast and reversed polarity, white letters on a black background. The handheld unit pictured below is currently in the $200 range.
 Portable electronic magnifier system. One of the most reasonably priced options for electronic magnification is the portable electronic reading aid by Mattingly. The pinhole style camera is plugged into the patient’s home television. Zoom magnification is available, along with enhanced contrast and reversed polarity, white letters on a black background. The handheld unit shown is currently in the $200 range.
Portable electronic magnifier system. One of the most reasonably priced options for electronic magnification is the portable electronic reading aid by Mattingly. The pinhole style camera is plugged into the patient’s home television. Zoom magnification is available, along with enhanced contrast and reversed polarity, white letters on a black background. The handheld unit shown is currently in the $200 range.
The complete CCTV system pictured below has the screen attached with excellent lighting conditions. The standard CCTV allows patients to write or do an activity requiring two hands under enhanced magnification. The costs for CCTVs currently range from $2000 to over $3000, depending on the monitor size and additional features such as a swivel camera that can be aimed at a distance as well as near. A new CCTV option includes text to speech, and the patient may read in a large font or scan and listen to the information.
 Complete closed-circuit television (CCTV) system. The complete CCTV system pictured has the screen attached with excellent lighting conditions. The standard CCTV allows patients to write or do an activity requiring two hands under enhanced magnification. The costs for CCTVs currently range from $2000 to over $3000, depending on the monitor size and additional features such as a swivel camera that can be aimed at a distance as well as near. A new CCTV option includes text to speech, and the patient may read in a large font or scan and listen to the information.
Complete closed-circuit television (CCTV) system. The complete CCTV system pictured has the screen attached with excellent lighting conditions. The standard CCTV allows patients to write or do an activity requiring two hands under enhanced magnification. The costs for CCTVs currently range from $2000 to over $3000, depending on the monitor size and additional features such as a swivel camera that can be aimed at a distance as well as near. A new CCTV option includes text to speech, and the patient may read in a large font or scan and listen to the information.
Adaptive equipment for daily living
Nonoptical aids can enhance greatly the patient's abilities to cope with reduced vision in daily life. Adaptive equipment is offered by a wide variety of distributors, including the following:
-
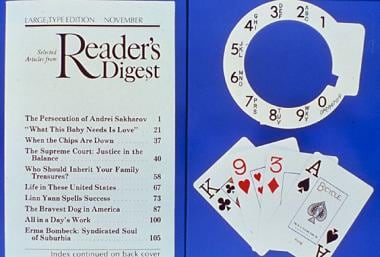
Large print material, such as the New York Times, and the Reader's Digest (see image below), allow patients with low-to-moderate vision loss to read with greater facility. Tablets and computers also provide access to larger font sizes.
-
Dial markers offer tactile cues for patients to set gauges on ovens, washers, dryers, and thermostats.
-
Self-threading needles allow patients to thread a needle without seeing the needle eye.
-
Books on tape (talking books) allow patients to keep current on a plethora of topics and to compensate for the lost pleasure of reading.
-
Talking clocks and watches help patients to keep time verbally.
-
Check signing and writing guides are stencils with openings cut out to allow the patient to write the date, amount, or signature without writing above or below the line.
-
Free telephone information calls are provided by most telephone services to patients who send in certification of visual impairment.
-
Descriptive video service provides narrated descriptions of visual elements (eg, actions, costumes, gestures, scene changes) in program.
-
Financial benefits: Patients who are certified as legally blind may be entitled to an extra exemption on their state income tax form and/or a higher standard deduction on their federal income tax form and may qualify for social security disability insurance or supplemental security income benefits.
-
In some states, handicapped parking permits are provided to visually impaired people with certification of visual impairment from an eye care practitioner.
-
Count-a-dose devices assist patients in obtaining the correct number of medications.
Eccentric viewing training
Patients with macular disease may benefit from learning to view objects with their peripheral vision. Instructions for eccentric viewing training are as follows:
-
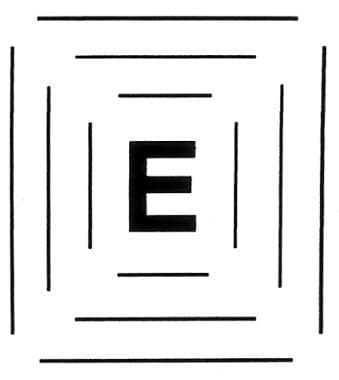
The boxed "E" (see image below) is used to determine where the patient needs to look to see the E most clearly. That area is marked on the box with an X. This is the eccentric viewing position.
-
Next, the patient is instructed to practice looking away and, then, back to the X.
-
The patient should move the E left and right, while maintaining fixation on the X. If the E becomes blurred or out of focus, then the patient is instructed to place the E centrally and refixate on the X. The exercise is repeated, while moving the E up and down.
-
Next, the patient has to repeat the exercise with an E that does not have an X or lines to guide the patient to the eccentric viewing position.
Contrast enhancement
Improving the contrast between images results in better visual recognition. Pouring milk into a white cup against a white tablecloth is one example of poor contrast. Using a different color tablecloth and/or cup can improve the contrast.
Optical prosthetic device
The Implantable Miniature Telescope (IMT), an optical prosthetic device, provides an innovative method of improving visual acuity in patients with moderate or severe ARMD. See image below.
The device is a fixed focus telescope (2.2X or 3.0X) mounted in a carrier with 2 rigid haptics. It consists of a glass cylinder 4.4 mm in length and 3.6 mm in diameter with a polymethylmethacrylate carrier. This visual prosthetic device enlarges retinal images in the central visual field, enabling patients to improve distance and near visual acuity. However, this also causes a severe reduction in the visual field. The fellow eye is needed to provide peripheral vision. In other words, one eye sees the magnified telescopic view, while the other eye maintains the full field of vision. Each eye is used monocularly, as it is impossible to fuse the two images.
Patient selection
Patient selection is critical to a successful surgical outcome because of the complexity of the surgery and the postoperative rehabilitation required in adapting to the device.
The IMT is appropriate for a small subset of patients. Selected patients have untreatable macular disease, have a fellow eye capable of mobility, and have a cataract or intraocular lens implant.
Patients must understand the procedure and the expected outcome. To demonstrate the concept of magnified central vision with peripheral vision loss, patients must try on a central telescope mounted in a pair of glasses. Patients need to understand that the 2 eyes will not work together, thereby creating a unique monovision concept. This idea is especially challenging to demonstrate in these patients because of the cataract in the eye that will be implanted.
In addition, patients must also understand the pros and cons of this device; they may gain better visual acuity but lose peripheral vision and binocularity.
Surgical procedure
The implantation for the telescope prosthesis is a complex procedure beyond typical cataract surgery.
The telescope has larger dimensions than an IOL, and the incision needs to be around 12 mm. A large capsulorrhexis of 7 mm with an intact capsular bag is needed for telescope implantation. First, the cortical lens material is completely removed to prevent residual cortex from being trapped between the telescope and the posterior capsule. A viscoelastic product, such as Healon, is used in the anterior chamber to prevent damage to the endothelium. Both haptics are placed in the capsule, and the IMT is then rotated to stabilize the device, with the haptics at the 6-o’clock position and the 12 o’clock position. This requires considerable surgical skill because of the size and the stiffness of the IMT.
Following surgery, patients require a longer course of anti-inflammatory medications as well as postoperative education/rehabilitation.
Postoperative refractive errors are corrected by spectacles. Because of the central position of the telescope, a separate pair of distance and reading glasses or a high-mounted bifocal may be used.
Outcomes
A 2-year multicenter clinical trial of the IMT has been completed, including follow-up on 206 patients (mean age, 76 y) who were operated on by 32 different surgeons. [9, 10] All patients had moderate to profound bilateral central vision loss resulting from bilateral, untreatable macular degeneration. The acuity and the visual field in their fellow eye were adequate enough for mobility, since the operated eye was to maintain only central vision. Patients also had significant cataracts in the eye to be implanted.
After 1 year, 67% of eyes with the implant achieved a 3-line or greater improvement in best-corrected distance visual acuity, and 53% of eyes achieved a 3-line improvement in distance and near visual acuity (10% for fellow eye controls). [9, 10] Overall, 90% of patients with the device implanted had a 2-line improvement in distance vision after the Phase I trial. [9, 10]
The National Eye Institute 25-item Visual Function Questionnaire (NEI VFQ-25) was used to evaluate changes in perceived visual function in daily living activities. [9, 10] The mean NEI VFQ-25 scores improved 7 points from baseline (p< 0.01), indicating an improvement in vision-related quality of life.
The endothelial count is critical, as the IMT protrudes through the pupillary plane by up to 0.5 mm, and telescope implantation is associated with endothelial cell loss. Trial results showed that the endothelial cell count was decreased an average of 25%, mostly occurring in the initial 3 months postoperatively and correlating with postsurgical corneal edema. [9, 10] There was no evidence of further endothelial trauma in the later postoperative period.
Rehabilitation concerns
A careful refraction is critical after implanting the telescope. Autorefractors and retinoscopy are not possible with the IMT. Because patients have a central vision of about 50 degrees, they may not adapt to a bifocal; therefore, a separate pair of distance and reading glasses may be used successfully. Another possibility is a very high bifocal for only the IMT eye so that patients may adjust the position only slightly to view through the bifocal prescription. Other low vision devices, such as magnifiers and high-power reading glasses, may be used in conjunction with the IMT.
Coordinating the monovision aspect (ie, one eye for peripheral vision and the other eye for detailed vision) is also challenging. Patients may seem to understand this concept prior to surgery, but they may later comment that they cannot get their 2 eyes to work together.
Coordination of care is critical so that patients have the appropriate glasses and other magnification tools to ensure a successful outcome. This multidisciplinary approach includes rehabilitation efforts both before and after surgery.
Occupational Therapy and Low Vision Rehabilitation
Occupational therapy practitioners working with persons with vision loss focus on increasing the person's level of independence with activities of daily living that have been compromised by visual impairment. The services can be provided in a clinic setting or in the person's home or work environment. Occupational therapists work with persons with age-related macular degeneration, diabetic retinopathy, glaucoma, retinitis pigmentosa, cataracts, visual field deficits from CVA, and traumatic brain injuries.
Occupational therapists train people in the use of the prescribed optical devices (eg, high power readers, magnifiers, telescopes, microscopes, video magnifiers) to successfully integrate the devices into daily livings tasks and activities. Difficulty with reading is the most noticeable result of vision loss. Tasks that present the greatest challenge are those that have low contrast features or small print. [11]
Occupational therapists may assist with the following self-care (grooming, dressing, bathing, eating) tasks:
-
Locating items needed for self-care
-
Safely entering and exiting the shower or tub
-
Correctly identifying medication
-
Properly administering medication, monitoring blood glucose levels
-
Tracking or logging medication routine
-
Selecting clothing by color
-
Locating and identifying food on a plate
Occupational therapists may assist with the following meal preparation tasks:
-
Accurately setting dials on ovens, burners, microwaves, toaster ovens
-
Reading directions on food packages and recipes
-
Reading nutritional labels
-
Correctly identifying measurements on cups and spoons
-
Safely cutting, slicing, chopping foods
-
Measuring items
Occupational therapists may assist with the following writing tasks:
-
Completing checks and financial records
-
Signing documents
-
Addressing envelopes
-
Writing personal notes, shopping lists
-
Filling out applications
Occupational therapists may assist with the following functional mobility tasks:
-
Safely walking through familiar and unfamiliar environments
-
Identifying visual detail, surface changes
Occupational therapists also train people in nonoptical options, such as the use of contrast and illumination, to increase visibility. In a clinic setting or during a Functional Home Living Assessment or Workplace Assessment, the occupational therapist can assist a person with the following:
-
Ensure lighting is optimal for task performance by evaluating overhead, ambient, and task lighting
-
Use contrast to increase visibility of key objects and landmarks
-
Use various materials to mark features of objects to increase their visibility or allow another sensory system to identify them (eg, colored plastic tape, tactile adhesive dots, Hi marks-tactual marking substance) or supplement visibility with auditory or tactile cues
-
Ensure even illumination and determine maximum lumens, minimum glare, flexible placement of lighting
-
Determine the type of lighting that works best (eg, incandescent, fluorescent, halogen, full spectrum)
-
Ergonomic completion of tasks to alleviate muscle strain and fatigue
For persons who have a central scotoma or blind spot, an occupational therapist assesses the awareness and ability to use the preferred retinal locus (PRL) in direct eye movement. This ability is highly correlated to the ability to read. Visual training skills can be implemented with pre-reading and writing exercises designed to improve accuracy and efficiency of reading and then graded to include continuous text. Areas assessed include the following:
-
Ability to locate and fixate on a target
-
Ability to perform saccades between a target
-
Ability to perform smooth pursuits or tracking
-
Ability to view target at distance and near
-
Reading performance to determine critical print size, maximum reading speed, reading comprehension, and reading endurance
Occupational therapists also work with people to increase awareness and participation in community resources, including the following:
-
Transportation services
-
Meals on wheels
-
Voice activated dialing
-
Large print and descriptive video services
-
Local support groups [11]
-
Sample examination form.
-
Lighthouse near acuity chart.
-
Microscope aid used monocularly at close working distance.
-
Stand magnifier useful for patients with poor dexterity.
-
Bioptic telescope allowed for driving in some states.
-
Large print material used for patients with low-to-moderate reading impairment.
-
Eccentric "E" used to retrain fixation away from a central scotoma.
-
Increased contrast helps patients maximize visual recognition.
-
Undilated view of Implantable Miniature Telescope.
-
Higher-power prism readers.
-
Higher-power prism readers.
-
Handheld magnifier.
-
Handheld magnifier.
-
Large monitor. A computer may be plugged into a large monitor, such as in the 42-inch television pictured. The text on the screen is 3 times larger even before adding computer program enhancement such as Zoomtext or other enlarging enhancing software options.
-
Portable electronic magnifier system. One of the most reasonably priced options for electronic magnification is the portable electronic reading aid by Mattingly. The pinhole style camera is plugged into the patient’s home television. Zoom magnification is available, along with enhanced contrast and reversed polarity, white letters on a black background. The handheld unit shown is currently in the $200 range.
-
Complete closed-circuit television (CCTV) system. The complete CCTV system pictured has the screen attached with excellent lighting conditions. The standard CCTV allows patients to write or do an activity requiring two hands under enhanced magnification. The costs for CCTVs currently range from $2000 to over $3000, depending on the monitor size and additional features such as a swivel camera that can be aimed at a distance as well as near. A new CCTV option includes text to speech, and the patient may read in a large font or scan and listen to the information.
-
Photos show normal view and views with reduced field and reduced contrast with blur.
-
Using prism half-eye reading glasses.
-
Using a handheld telescope.