Background
Typhoid fever, or enteric fever, is a potentially fatal multisystemic infection produced primarily by Salmonella enterica serotype typhi and to a lesser extent Salmonella enterica serotypes and paratyphi A, B, and C. Salmonella are motile enterobacteriaceae that can produce a variety of gastrointestinal infections. The most serious of these is typhoid that is primarily produced by Salmonella enterica serotype typhi and, to a lesser extent, S enterica serotypes paratyphi A, B, and C. It presents in a wide variety of ways ranging from an overwhelming septic illness to minor cases of diarrhea with low-grade fever. The classic presentation is one of fever, malaise, diffuse abdominal pain, and constipation. Untreated typhoid fever may progress to delirium, obtundation, intestinal hemorrhage, bowel perforation, and death within 1 month of onset. Survivors may be left with long-term or permanent neuropsychiatric complications. The term typhoid derived from the ancient Greek word for cloud, was chosen to emphasize the severity and long lasting neuropsychiatric effects among the untreated. Yearly, 21 million people acquire typhoid fever throughout the world. It is fatal in approximately 161,000. Over the years, it has developed increasing resistance to antibiotics. During 2016, extensively drug-resistant typhoid (XDR) were documented in Pakistan. Only three classes of antimicrobial agents, azithromycin, carbapenems, and tigecycline, remain affective among these strains. [1]
Typhoid thrives in conditions of poor sanitation, crowding, and social chaos. [1] Although antibiotics have markedly reduced the frequency of typhoid fever in the developed world, it remains endemic in developing countries. The incidence of infections with S paratyphi may be surpassing those due to S typhi. This may be due to the immunologic naïveté of a given population as well as the incomplete coverage provided by current Typhoid vaccines against these pathogens. Non -Typhoidal strains usually produce mild, self-limiting gastroenteritis. [2]
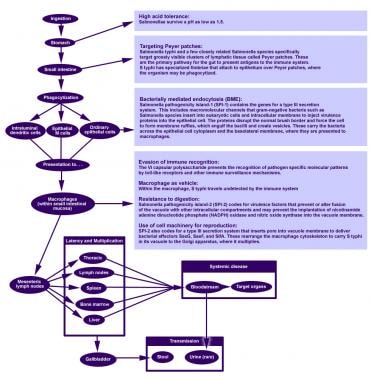
Pathophysiology
Pathogenic Salmonella species are engulfed by the phagocytic cells of the gut, which then present them to the macrophages of the lamina propria. By means of their toll-like receptor (TLR)–5 and TLR-4/MD2/CD-14 complexes, the macrophages recognize pathogen-associated molecular patterns (PAMPs) such as flagella and lipopolysaccharides. Macrophages and intestinal epithelial cells then mobilize T cells and neutrophils with interleukin 8 (IL-8). Hopefully, the resulting inflammation will be adequate to suppress the infection. [3, 4]
S typhi and paratyphi enter the host's system primarily through the distal ileum. They have specialized fimbriae that adhere to the epithelium over clusters of lymphoid tissue in the ileum (Peyer patches), the main relay point for macrophages traveling from the gut into the lymphatic system. The bacteria then induce their host macrophages to attract more macrophages. [3]
S typhi has a Vi capsular antigen that masks PAMPs, avoiding neutrophil-based inflammation, whereas the most common paratyphi serovar, paratyphi A, does not. This may explain the greater infectivity of Typhi as compared with paratyphi isolates. [5]
In addition,serotypes typhi and paratyphi are able to Quorum Sense. This is a type of intracellular communication by which the organisms coordinate swarming and biofilm production. [6]
Typhoidal salmonella co-opt the macrophages' cellular machinery for their own reproduction [7] as they are carried through the mesenteric lymph nodes to the thoracic duct and the lymphatics and then through to the reticuloendothelial tissues of the liver, spleen, bone marrow, and lymph nodes. Once there, they pause and continue to multiply. When a critical density is reached, the bacteria bring about macrophage apoptosis.This allows salmonella to enter the bloodstream [4]
The bacteria then infect the gallbladder via either bacteremia or direct extension of infected bile. The result is that the organism re-enters the gastrointestinal tract in the bile and reinfects Peyer patches. Bacteria that do not reinfect the host are shed in the stool and so become available to infect others. [2, 4]
Chronic carriers are responsible for much of the transmission of the organism. While asymptomatic, they may continue to shed bacteria in their stool for decades. The organisms sequester themselves either as a biofilm on gallstones or gallbladder epithelium or, perhaps, intracellularly, within the epithelium itself. [8] The bacteria excreted by a single carrier may have multiple genotypes, making it difficult to trace an outbreak to its origin. [9]
Risk factors
Typhoidal salmonella have no nonhuman vectors. An inoculum as small as 100,000 organisms of typhi causes infection in more than 50% of healthy volunteers. [10] Paratyphi requires a much higher inoculum to infect, and it is less endemic in rural areas. Hence, the patterns of transmission are slightly different.
The following are modes of transmission of typhoidal salmonella:
-
Oral transmission via food or beverages handled by an often asymptomatic individual—a carrier—who chronically sheds the bacteria through stool or, less commonly, urine
-
Hand-to-mouth transmission after using a contaminated toilet and neglecting hand hygiene
Paratyphi is more commonly transmitted in food from street vendors. It is believed that some such foods provide a friendly environment for the microbe.
Paratyphi is more common among newcomers to urban areas, probably because they tend to be immunologically naïve to it. Also, travellers get little or no protection against paratyphi from the current typhoid vaccines, all of which target typhi. [14, 15]
Typhoidal salmonella are able to survive a stomach pH as low as 1.5. Antacids, histamine-2 receptor antagonists (H2 blockers), proton pump inhibitors, gastrectomy, and achlorhydria decrease stomach acidity and facilitate S typhi infection. [4]
HIV/AIDS is clearly associated with an increased risk of nontyphoidal Salmonella infection; however, the data and opinions in the literature as to whether this is true for S typhi or paratyphi infection are conflicting. If an association exists, it is probably minor. [16, 17, 18, 19]
Other risk factors for typhoid fever include various genetic polymorphisms. These risk factors often also predispose to other intracellular pathogens. For instance, PARK2 and PACGR code for a protein aggregate that is essential for breaking down the bacterial signaling molecules that dampen the macrophage response. Polymorphisms in their shared regulatory region are found disproportionately in persons infected with Mycobacterium leprae and S typhi. [12]
On the other hand, protective host mutations also exist. The fimbriae of S typhi bind in vitro to cystic fibrosis transmembrane conductance receptor (CFTR), which is expressed on the gut membrane. Two to 5% of white persons are heterozygous for the CFTR mutation F508del, which is associated with a decreased susceptibility to typhoid fever, as well as to cholera and tuberculosis. The homozygous F508del mutation in CFTR is associated with cystic fibrosis. Thus, typhoid fever may contribute to evolutionary pressure that maintains a steady occurrence of cystic fibrosis, just as malaria maintains sickle cell disease in Africa. [20, 21]
As the middle class in south Asia grows, some hospitals there are seeing a large number of typhoid fever cases among relatively well-off university students who live in group households with poor hygiene. [22] American clinicians should keep this in mind, as students from these areas often come to the United States for further education. [23]
Epidemiology
Frequency
United States
Since 1900, improved sanitation and successful antibiotic treatment have steadily decreased the incidence of typhoid fever in the United States. In 1920, 35,994 cases of typhoid fever were reported. In 2006, there were 314.
Between 1999 and 2006, 79% of typhoid fever cases occurred in patients who had been outside of the country within the preceding 30 days. Two thirds of these individuals had just journeyed from the Indian subcontinent. The 3 known outbreaks of typhoid fever within the United States were traced to imported food or to a food handler from an endemic region. Remarkably, only 17% of cases acquired domestically were traced to a carrier. [24]
International
Typhoid fever occurs worldwide, primarily in developing nations whose sanitary conditions are poor. Typhoid fever is endemic in Asia, Africa, Latin America, the Caribbean, and Oceania, but 80% of cases come from Bangladesh, China, India, Indonesia, Laos, Nepal, Pakistan, or Vietnam. [25] Within those countries, typhoid fever is most common in underdeveloped areas. Typhoid fever infects roughly 21.6 million people (incidence of 3.6 per 1,000 population) and kills an estimated 200,000 people every year. [26]
In the United States, most cases of typhoid fever arise in international travelers. The average yearly incidence of typhoid fever per million travelers from 1999-2006 by county or region of departure was as follows [24] :
-
Western Hemisphere outside Canada/United States - 1.3
-
Africa - 7.6
-
Asia - 10.5
-
India - 89 (122 in 2006)
-
Total (for all countries except Canada/United States) - 2.2
Mortality/Morbidity
With prompt and appropriate antibiotic therapy, typhoid fever is typically a short-term febrile illness requiring a median of 6 days of hospitalization. Treated, it has few long-term sequelae and a 0.2% risk of mortality. [24] Untreated typhoid fever is a life-threatening illness of several weeks' duration with long-term morbidity often involving the central nervous system. The case fatality rate in the United States in the pre-antibiotic era was 9%-13%. [27]
Race
Typhoid fever has no racial predilection.
Sex
Fifty-four percent of typhoid fever cases in the United States reported between 1999 and 2006 involved males. [24]
Age
Most documented typhoid fever cases involve school-aged children and young adults. However, the true incidence among very young children and infants is thought to be higher. The presentations in these age groups may be atypical, ranging from a mild febrile illness to severe convulsions, and the S typhi infection may go unrecognized. This may account for conflicting reports in the literature that this group has either a very high or a very low rate of morbidity and mortality. [22, 28]
-
Life cycle of Salmonella typhi.