Background
Lower eyelid aging results in prominent adipose tissue, skin redundancy, increased rhytids, and laxity.
The traditional technique includes a subciliary incision with removal of fat, skin, and hypertrophied orbicularis muscle and canthal tightening. This approach can result in ectropion, retraction, and canthal angle blunting in 5-20% of patients. [1, 2]
The transconjunctival approach allows for fat rearrangement, debulking, and arcus marginalis release, leading to improved eyelid contour. This approach does not address dermatochalasis, rhytids, or skin texture. The use of the carbon dioxide laser for resurfacing has been used successfully to reduce these findings. [1, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13]
The images below depict a patient who underwent combined upper and lower laser blepharoplasty, perioral and periorbital carbon dioxide laser resurfacing, SMAS facelift, and full-face blue peel.
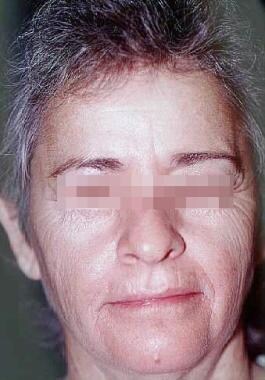 Laser tissue resurfacing. Female patient with skin and muscle laxity, photoaging, and dermatochalasis.
Laser tissue resurfacing. Female patient with skin and muscle laxity, photoaging, and dermatochalasis.
Pathophysiology
Lasers target water-containing tissue. Treatment with lasers results in tissue vaporization. [14, 15]
Indications
Indications for carbon dioxide laser skin resurfacing include the following:
-
Verruca vulgaris/plana
-
Junctional and compound nevi
-
Lentigo simplex
-
Small syringomas
-
Epidermal melasma
-
Scars [17]
-
Dermatoheliosis
Relevant Anatomy
Extensive knowledge of skin microanatomy, histology, and physiology is essential before proceeding with resurfacing procedures. Familiarity with relative facial skin thickness (ie, thin, medium, thick) is necessary to limit overtreatment and potential complications.
Contraindications
Absolute contraindications to carbon dioxide laser skin resurfacing are as follows:
-
Active bacterial, viral, or fungal infections
-
Oral isotretinoin use within the previous 6 months
-
Tendency for keloid or hypertrophic scar formation
-
Ectropion
-
Unrealistic expectations
-
Uncooperative patient
Relative contraindications to carbon dioxide laser skin resurfacing are as follows:
-
Poor general health
-
Continued ultraviolet exposure
-
Prior radiation to area of proposed treatment
-
Fitzpatrick skin phototypes V-VI
-
Reticular dermis-level resurfacing procedure within the preceding 2-3 months
-
Unwillingness to accept the possibility of postoperative erythema or hypopigmentation
-
Significant eyelid laxity
-
Excessively thin or thick skin
-
Collagen vascular disease, HIV, or hepatitis C infection
-
Depigmentation seen periorbitally, periorally, and on the forehead following carbon dioxide laser resurfacing.
-
Laser tissue resurfacing. Female patient with skin and muscle laxity, photoaging, and dermatochalasis.
-
Same patient as in image above underwent combined upper and lower laser blepharoplasty, perioral and periorbital carbon dioxide laser resurfacing, SMAS facelift, and full-face blue peel. This photograph was taken 6 months after the procedure.











