Background
Many corneal refractive procedures, including automated lamellar keratoplasty, photorefractive keratectomy (PRK), laser in situ keratomileusis (LASIK), holmium:YAG (Ho:YAG) laser, and conductive keratoplasty, have been available to treat low-to-moderate hyperopia. The safety and the accuracy of PRK and LASIK for the treatment of hyperopia have improved over the years, but are still not as stellar as they are for the treatment of myopia. The quality of correction has advanced with the use of wavefront analysis and its seamless incorporation in refractive surgery.
Today, the quality of corneal refractive procedures is improving. Lens-related procedures are getting more popular. They include phakic intraocular lenses and a procedure like clear lens extraction with high-plus power lens implantation. Clear lens extraction causes a loss of accommodation but is preferred if the patient is older than 45 years or has any degree of cataract. However, presbyopia-correcting lenses, ie, multifocal (bifocal, trifocal, quadrifocal), accommodative, extended depth of focus, varifocal, and polyfocal intraocular lenses can overcome the problem of near vision.
Two types of intraocular lenses (IOLs) are mainly used in hyperopes: the precrystalline lens implant (implantable Collamer lens) and the iris-fixated lens (Artisan lens).
The Artisan lens is shown in the image below.
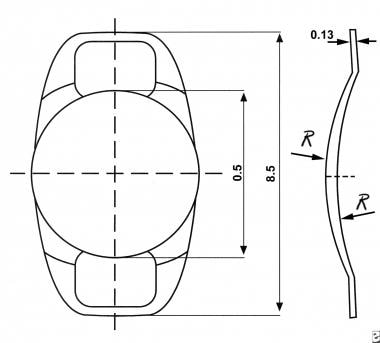 The dimensions of the Artisan phakic lens. The lens is 8.5 mm at the widest point, far away from the angle of the anterior chamber. The optic is vaulted suitably to stay clear of the iris cone.
The dimensions of the Artisan phakic lens. The lens is 8.5 mm at the widest point, far away from the angle of the anterior chamber. The optic is vaulted suitably to stay clear of the iris cone.
An angle-supported lens has been used very rarely in hyperopes and has fallen out of fashion owing to associated complications related to increased intraocular pressure and loss of endothelial cells.
Each lens has its advantages and disadvantages. The early problems are related to the design of the lens and the meticulous details of surgery. The late postoperative complications are related to the interaction of the IOL and the intimate ocular tissues during the lifetime of the patient. Lifelong, regular follow-up care is essential in all cases. Explantation of the phakic lens may ameliorate some of the complications.
Later in life, if the patient develops a cataract, performing an atraumatic explantation, followed by extracting the cataract and implanting another appropriate IOL, should be possible. A foldable Visian ICL hyperopia lens is easier to explant than a rigid Artisan hyperopia lens.
Refractive corneal surgery had the potential to rival the visual results of phakic lens implants, as it can correct both the spherical error and the cylindrical error. Wavefront analysis and its incorporation in the ablation process improve the image definition. The authors no longer advocate the use of laser refractive corneal surgery because of the possibility of regression in such a surgical (hyperopia) profile. Laser hyperopic corneal corrections results in loss of effect over time because of the natural or sometimes hyperplastic healing response of the cornea to fill in this ablated step between the treated and untreated zones.
History of the Procedure
In 1977, Worst designed and used a pure iris support lens. This iris claw lens was fixed to the anterior surface of the iris independent of the pupil. Over the next 9 years, it was well tolerated and used extensively in aphakes of Holland and India. An iris claw lens is shown in the image below.
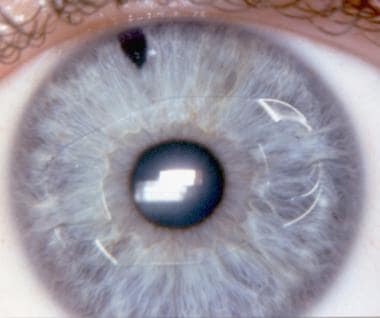 The iris claw lens for a phakic hyperopic eye, implanted in the eye of a blue-eyed patient. Minimal essential iris fold in the lens claw exists for the purpose of fixation. Jan Worst, the designer of the lens, considers the peripheral part of the iris as a silent area. It is least affected by the pupillary movements.
The iris claw lens for a phakic hyperopic eye, implanted in the eye of a blue-eyed patient. Minimal essential iris fold in the lens claw exists for the purpose of fixation. Jan Worst, the designer of the lens, considers the peripheral part of the iris as a silent area. It is least affected by the pupillary movements.
In 1986, Fechner used a negative-power iris claw lens for treating phakic myopes. Soon after, Singh used it in phakic hyperopes. In 1998, Fechner, Singh, and Wulff presented their 10-year experience with 69 cases. [1]
In 1996, Davidorf, Zaldivar, and Oscherow presented their results with the STAAR Collamer plate haptic posterior chamber phakic IOL in 24 phakic hyperopes. [2] In 1998, Rosen and Gore followed with 9 cases; in 1999, Pesando, Ghiringhello, and Tagliavacche followed with 15 eyes; and, in 1999, Sanders followed with 10 eyes. [3, 4]
Koivula and Zetterstrom evaluated the use of PRL phakic IOL for hyperopia and found that the main complication was early pupillary block. [5]
At present, there are many presentations of small series of cases with a short follow-up, with both iris claw lenses and posterior chamber refractive lenses.
Angle-supported lenses in phakic hyperopes have not made headway.
Problem
Hyperopia is a common refractive error that exists from a young age. A unilateral hyperopia, with or without amblyopia, might remain undiscovered for a long time. The treatment of unilateral hyperopia is not easy. The child is not impressed by the glass or the contact lens for the affected eye, since the other eye is so much better. Most parents give up all efforts out of sheer frustration, and the magnitude of wasted sight is immense.
Numerous innovative corneal procedures have been tried. All have been discontinued because of the difficult nature of these procedures, the serious flaws, and the complications.
Two promising modalities have appeared: the excimer laser for use as PRK or LASIK and the newly designed phakic IOLs. While experience with these modalities exists in adult patients, experience with them in young patients is also receiving increased attention. Phakic lenses are hazardous in pediatric patients with hyperopia.
The optic-mechanical solution to the problem of hyperopia is only one side of the story. The prevention and management of amblyopia are equally important, but efforts in these areas are lagging. When the latter are strongly addressed, hyperopia surgery will become a hot topic.
Epidemiology
Frequency
The incidence of +2 diopters (D) or higher hyperopia under cycloplegic refraction is as follows: 19% of patients aged 7-8 years, 3.6% of patients aged 14-15 years, and approximately 25% of adults have some degree of hyperopic refractive error.
Etiology
Much remains unknown about the developing eye, especially in relation to hyperopia. Hyperopia is known to result when the refracting optics of the eye can focus the parallel rays from infinity to a point behind the retina (relative to the length of the eyeball).
Newborns are moderately hyperopic, but they have a broad distribution of refractive errors. As the eye grows, a shift toward emmetropia occurs. Hyperopia perhaps represents a failure of the emmetropization process. Slow eyeball growth can be a cause of hyperopia and is the reason why hyperopia does not disappear with age.
Pathophysiology
The phakic posterior chamber lenses and the iris claw lenses contact different ocular tissues, so different mechanical and biological responses are elicited by each lens.
The precrystalline lens implant is made of soft lens material. It occupies a narrow space between the natural crystalline lens and the posterior surface of the iris. Despite its design to avoid touching the crystalline lens and the posterior surface of the iris, it is often difficult to achieve this situation. Touching or rubbing against the posterior pigment epithelium of the iris is inevitable. Similarly, touching the ciliary epithelium is unavoidable.
During blinking, squeezing, and rubbing, the pressure and friction between the IOL and the surrounding tissues are inevitable. Even if the frictional force is very small, it is bound to continue for life. When shed from the iris and ciliary process, the pigment may lead to glaucoma. Developing diabetes also is a concern. The disease causes changes in the posterior pigment epithelium of the iris, possibly causing excessive shedding of pigment. An inflammatory process can bind the lens to the iris, the ciliary body, or even the crystalline lens. An intermittent or a continuous touch with the anterior lens capsule can produce lens opacification. Sometimes, the presence of the artificial lens in the posterior chamber can crowd the angle of the anterior chamber, leading to glaucoma.
The posterior chamber lens is sized empirically by subtracting 0.5 mm from the white-to-white corneal diameter. A short lens rubs against the anterior lens capsule, and a long lens impinges on the ciliary body and the posterior pigment epithelium of the iris.
An iris-fixated lens (iris claw lens) is fixed to the anterior surface of the iris via the in-built claws in the haptic of the lens. To achieve fixation, the claw holds a fold of the iris on either side of the pupil. The lens does not produce complications related to the angle of the anterior chamber, the crystalline lens, pigment epithelia of the iris, or the ciliary body. Consider the possibility that the iris tissue inside the claw will atrophy, leading to a late dislocation or possible breakdown of blood-aqueous barrier at the site of fixation. Blinking and squeezing do not produce friction between the iris and the IOL. Rubbing and pressing may produce an endothelial touch.
In both types of phakic IOLs, increased crystalline lens size with increasing age and cataract formation tends to increase the aforementioned risks. While the results of phakic IOLs are highly predictable, the long-term pathological changes and safety factors have been known only for about a dozen years.
Presentation
The eyeball may be placed normally, or it may be set deeply. The cornea may have a normal diameter, or some degree of microcornea may exist. The following may vary within the specified ranges:
-
Axial length - 15-23 mm
-
Keratometry reading - 38-50 D
-
Depth of the anterior chamber - 2.5-4 mm
-
Hyperopia - A low of +2 D or +3 D to as high as +18 D
The intraocular pressure (IOP) should be normal, and the patient should not be under treatment for any kind of glaucoma. In addition, unilateral moderate or severe hyperopia cases usually have amblyopia in the affected eye. The patient may have strabismus, nystagmus, or both.
Indications
Patients may experience unilateral or bilateral hyperopia. The corrected visual acuity may be normal in both eyes, normal in one eye with amblyopia in the other eye, or subnormal in both eyes. Strabismus or nystagmus may be present.
Patients may be dissatisfied and desire surgery because of thick glasses, cosmetic reasons, or poor visual acuity and peripheral vision. Two popularly misguided reasons why patients may desire surgery exist, frustration with (lack of) visual quality or the assumption that surgery will be as helpful for hyperopia as it is for myopia.
Refractive surgery by phakic IOLs among the hyperopes is not as popular as in myopes, simply because it has not been available as long. If the patient who is hyperopic agrees to refractive correction, especially if it is likely to help work-related tasks, then the search for the right modality of treatment begins. People do try to collect all information about the possibility of their getting benefited by a safe and proven technology through a trustworthy ophthalmologist. When patients are in the office, they do ask for clear-cut information on the various options and what option may suit them best. The ophthalmologist must consider personal experience and equipment. If resources are insufficient for a given case, the patient should be referred to a suitable institution.
The practical options for the cornea are PRK and LASIK; for intraocular implantation procedures, a posterior chamber lens and an iris claw lens. Both types of intraocular lenses are available worldwide.
When planning for an IOL implant in phakic hyperopes, consider the following:
-
What is the minimum age at which the lens is to be implanted?
-
What is the minimum or the maximum refractive error to be treated?
-
What should be the lowest limit for anterior chamber depth?
-
What is the lowest limit for the diameter of the cornea beyond which there will be a refusal to perform surgery?
-
How accurate is the white-to-white diameter on the basis of which the length of a length is to be derived?
-
What are the smallest available lenses of the 2 types (ie, posterior chamber lens, iris claw lens)?
-
How can the risk of complications be minimized? What will those complications be? What will be the chances of occurrence?
The final decision to do lens implantation comes after careful contemplation and detailed consultations and discussions with the patient or the parents.
Relevant Anatomy
The following anatomical features involved in phakic lens implantation are important:
-
The space availability for the implanted lens
-
The structures with which the lens will intimately contact
-
The effect of age on the dimensions of various involved structures and spaces
The pupillary margin normally rests on the crystalline lens. Maximum contact is in a mid-dilated condition. The posterior chamber, which has a volume of 65 µL, is a triangular space on section. The base is toward the periphery, and the apex is toward the pupillary margin (where the chamber depth is zero). In the case of a posterior chamber lens, the thickest part of the implant, the optic, occupies the shallowest or the zero space.
If a plate haptic lens has to stay clear of the crystalline lens, it should vault in the central area. This can happen only if the haptic rests strongly on the ciliary processes and bows forward. Staying clear of the crystalline lens can lead to rubbing against the posterior pigment. It also means impinging on the ciliary epithelium of the ciliary processes. If the ciliary epithelium sheds, then the implanted lens will further touch the ciliary vasculature. The ciliary capillary endothelium has fenestrations of 30-100 µm, which are permeable to plasma proteins and tracer elements. Lying between the crystalline lens and the iris, the phakic posterior chamber lens produces resistance to the flow of aqueous. The increasing volume of the crystalline lens with age encroaches on the posterior chamber volume. The crystalline lens volume increases by almost 50% from 150 µL to 240 µL in a matter of 60 years.
The average anterior chamber depth is 3.15 mm (2.6-4.4 mm). The volume of the anterior chamber is 250 µL, which decreases by 7.5% per decade.
The iris is 0.5 mm thick at the root and 0.6 mm at the collarette. An iris claw lens is attached to the peripheral anterior surface of the iris by pushing a fold of the iris into the 2 claws of the lens. Consider the following 3 points:
-
The space available around the lens and the distance from the corneal endothelium and the crystalline lens
-
The anatomy of the iris, especially the vasculature, as it is fixed in the claws of the lens
-
The pupil movements and the friction between the iris and the phakic iris claw lens
The posterior surface of the IOL is concave and cannot touch the crystalline lens. A respectable distance exists between the various parts of the lens and the corneal endothelium. The maximum height of the optic, which is in the center, is less than 1 mm. The haptic of the lens in the periphery is 0.18 mm. The growth of the crystalline lens with age tends to reduce the depth of the anterior chamber. The maximum width of the implant lens is 8.5 mm, which allows it to remain away from the structures of the angle of the anterior chamber.
The vasculature of the iris is peculiar. The vascular endothelium of the human iris is not fenestrated. The endothelial cells of the iris vessels are joined by 2 types of intercellular junctions, the zonular tight junctions and the gap junctions. The vessels are covered in layers in the following order:
-
Pericytes
-
0.5-3 µm wide basal lamina
-
7 µm zone of sparse, longitudinally directed collagen fibers
-
Granular ground substance
-
Another 10 µm wide connective tissue layer
Vessels that are located in the more cellular parts of the stroma (eg, anterior border layer) are invested in thicker and more cellular adventitia. These vascular peculiarities explain why the claw lens can grip the iris fold.
Friction between the iris claw lens and the anterior surface of the iris is possible at 2 points, in the immediate vicinity of the 2 claws. Nothing serious happens in aphakes, and it is unknown if, on a long-term basis, phakic eyes respond similarly.
Contraindications
These guidelines should prevent early or late postoperative problems, which permanently may threaten vision. Two basic factors are quintessential, as follows:
-
Patients should come for regular follow-up care throughout their lifetime. If a patient cannot comply, that patient is not a suitable candidate.
-
A fail-safe IOL design should be chosen. If the surgeon cannot confidently explant the lens after months and years without incurring any trauma to the eye, do not implant.
Eyes that already have vision-threatening problems (eg, uveitis, diabetic retinopathy glaucoma) are excluded to avoid precipitating more complications.
The patient and ocular parameters and the proposed lens design impose many restrictions. The patient should not rub the operated eye. Young children who cannot follow these instructions should not receive implanted phakic lenses. Hyperopic children older than 14 years have been more reliable and cooperative. Amblyopic patients deserve much-needed refractive crutches at an early age.
The smallest available posterior chamber phakic lens diameter is 11 mm. The length of the lens is calculated by subtracting 0.5 mm from the white-to-white limbal diameter. The minimum white-to-white diameter should be 11.5 mm. Any degree of microcornea from this size is a contraindication for posterior chamber lens implantation. In the case of an iris claw lens, customized, smaller lenses are possible. While the normal phakic lens is 8.5 mm wide, the iris claw lens may be made as small as 6 mm, thus greatly extending its application.
Anterior chamber depth is an important consideration for posterior chamber lenses and iris claw lenses. A depth of less than 2.75 mm is a contraindication. The posterior chamber lens may cause crowding of the angle, but the iris claw lens will encroach on the central depth of an already shallow anterior chamber.
The presence of amblyopia should not be a contraindication for the following purposes:
-
To reduce the power of the glasses and to improve the chances of spontaneous improvement of amblyopia
-
To provide a greater freedom of movement
-
Later, to attempt to improve the eyesight with pleoptic exercises
The lens, which is fixed to the anterior surface of the iris, can be examined from end-to-end under the slit lamp microscope throughout the patient's life. A posterior chamber lens cannot be examined in this manner. In the latter case, it can only be presumed that all is well at the haptic-ciliary junction or implant-iris touch areas. If inflammation develops and the pupil fails to dilate, only indirect inferences can be drawn. Therefore, the emphasis on contraindication can shift from patient to the implant and vice versa, depending upon the peculiarities of each patient.
-
A stereo pair demonstrates that the iris diaphragm is designed like a cone. The apex has been cut to make a pupil. An artificial lens behind the iris lifts this cone. An artificial lens to be kept in front of the iris has to be designed to stay clear of the cone. Otherwise, it impinges on the iris, the pupil, and the crystalline lens.
-
The dimensions of the Artisan phakic lens. The lens is 8.5 mm at the widest point, far away from the angle of the anterior chamber. The optic is vaulted suitably to stay clear of the iris cone.
-
The iris claw lens for a phakic hyperopic eye, implanted in the eye of a blue-eyed patient. Minimal essential iris fold in the lens claw exists for the purpose of fixation. Jan Worst, the designer of the lens, considers the peripheral part of the iris as a silent area. It is least affected by the pupillary movements.
-
An early version of the iris claw lens that was used to treat high hyperopia. The optic is 4.25 mm, and the overall length is much smaller. The optical section shows how far away the corneal endothelium is located. The lens is well tolerated, even by the pigmented iris.
-
An optical section, taken 7 years postoperatively, shows that this hyperopia lens is well tolerated by the eye. Iridectomy is an essential part of the procedure. The angle of the anterior chamber, the crystalline lens, and the corneal endothelium are not at risk because they are far away.
-
A phakic iris claw lens for hyperopia, fixed close to the collarette (an early version), the optic of which barely covers the pupil. It provides extreme safety, being wholly located in the deepest part of the anterior chamber. This lens size suffices for most people with black eyes, although some complain of glare from the edge of the optic. A small optic, small lens might be good in black eyes and in nonautomobile societies.
-
The phakic iris claw lens has no tendency to shift, either by itself or even by pupil dilatation with mydriatics. Because it does not touch the crystalline lens, there is no danger to its transparency. This red reflex picture after dilatation, taken 10 years postoperatively, shows that the lens is well tolerated.
-
This iris claw lens in an aphake shows how it is well tolerated by the iris. This 65-year-old patient had a primary implant 32 years ago. The claws are shifted upward (Singh variation of worst iris claw lens). No viscoelastic was available then. The endothelial cell count is 1980/sq mm. Best corrected vision is 6/6. The pictures are in 3D.










