Background
Because of the numerous refractive surgery terms that are used almost exclusively in the successful understanding of refractive disorders, first presenting a glossary of terms to assist the reader is essential.
Glossary of terms
Ablation - Removal. In excimer laser surgery, a frequency of energy causes corneal molecules to detach from one another from their points of attachment.
AK - Abbreviation for astigmatic keratotomy
ALK - Abbreviation for automated lamellar keratectomy
ArF - Abbreviation for argon fluoride
ASA – Abbreviation for advanced surface ablation. A collective term sometimes used to refer to the current techniques for surface treatments.
Astigmatic keratotomy - Surgical procedure in which microscopic incisions are positioned in the peripheral cornea to create a more spherical shape
Astigmatism - A refractive condition where the surface of the cornea is not spherical. A distorted image is formed because light images focus on 2 separate points in the eye.
Automated lamellar keratoplasty - An incisional refractive surgery method used in low-to-moderate myopia. An automated microkeratome placed on the eye removes, in an oscillating shaving motion, a thin layer of cornea that is microns thick. Subsequent removal of a thinner underlying corneal stroma is performed with stitchless replacement of the initial superficial cap.
Excimer - Abbreviation for excited dimer
LASEK - Abbreviation for laser epithelium keratomileusis
Laser - Abbreviation for light amplification by the stimulated emission of radiation
Laser in situ keratomileusis - A refractive laser procedure combining the use of ALK and photorefractive keratectomy in reshaping the central cornea to treat refractive errors. An automated microkeratome, similar to that used in ALK, is used to fashion a flap with a hinge. Subsequent ablation is performed on the corneal stromal bed with stitchless replacement of the corneal flap.
Laser epithelium keratomileusis - A modification of the epithelial debridement performed in photorefractive keratectomy. In this procedure, the epithelium is detached with the use of an alcohol solution (usually 20%) to lyse DNA bonds (cleave basement membrane) and to soften the epithelium to facilitate rolling over into a flap. Ablation is performed subsequently with replacement of the epithelial flap.
LASIK - Abbreviation for laser in situ keratomileusis
Light amplification by stimulated emission of radiation - Laser light is composed of one color (wavelength) traveling in one direction, and each light wave is traveling in step with the adjacent wave, making the laser light more powerful by a factor of millions.
Oblate - Shape of the cornea after conventional laser ablation profile where it is steeper in the periphery
PARK - Abbreviation for photoastigmatic refractive keratectomy
Pachymetry - Optical or ultrasonic procedure to measure the corneal thickness
Photoastigmatic refractive keratectomy - Although similar to photorefractive keratectomy, the ablation profile is specific for astigmatism.
Photorefractive keratectomy - Surgical procedure using an excimer laser to fashion the central cornea to treat refractive errors
Prolate - Normal corneal shape; steeper in the center
PRK - Abbreviation for photorefractive keratectomy
Topography - Used to measure the low or high areas of a plane
Wavefront - Describes the surface that connects all the points on a propagating light wave that are of equal phase
Wavelength - The distance between the top of one wave and the top of the next wave. In the case of an excimer laser, this is measured in nm (eg, argon fluoride has a wavelength of 193 nm).
Astigmatism and the advent of photoastigmatic refractive keratotomy
Astigmatism, a refractive condition in which the surface of the cornea is not spherical, can decrease visual acuity by forming a distorted image because light images focus on 2 separate points in the eye. Clinicians and surgeons have searched constantly for the most successful device or procedure to treat this refractive error. Nonsurgical devices include spectacles and contact lenses. To date, these devices are being improved continuously to address the complex problem of astigmatism. Initial surgical approaches include astigmatic keratotomy, compression sutures, and wedge resection. Recent surgical procedures involve the use of the excimer laser in PARK and LASIK with or without wavefront-guided technology. [1]
PRK is the application of ultraviolet high-energy photons (193-nm wavelength) of the ultraviolet range generated by an argon fluoride excimer laser to the anterior corneal stroma to change its curvature and, thus, to correct a refractive error. [2, 3] The physical process of remodeling by PRK is called photoablation. This surgical procedure reshapes the central cornea to a flatter shape for people who are nearsighted and a more curved surface for people who are farsighted. Several techniques are being used to correct for astigmatism.
Device description
Two different methods of energy delivery are available by the excimer laser device, a large circular beam and a scanning slit or spot.
The earlier devices initially used large area ablation. To date, some manufacturers still use large area ablation in their modern devices. The circular laser beam passes through a diaphragm that slowly enlarges to deliver more cumulative energy in the center and less in the periphery. [4, 5] Some laser-induced irregularities (central islands) have been reported in these large area systems. This method results in a shorter operating time to deliver the necessary laser pulses versus a system that uses a scanning slit system. The following manufacturers use circular beam lasers: Schwind (Coherent Medical Inc, Palo Alto, CA), Summit (Waltham, MA), [6, 7, 8] and VISX (Santa Clara, CA).
The scanning slit or spot is an alternative method of energy delivery by the excimer laser. A smaller beam passes through a beam-shaping aperture, delivering a pattern of more pulses centrally than peripherally and resulting in greater corneal tissue ablation centrally. Less total energy is delivered at the corneal surface; therefore, a less powerful laser device may be used. In principle, this system is more effective in providing different ablation patterns in the treatment of astigmatism, irregular astigmatism, and hyperopia.
The use of scanning laser technology with its small moving beam has resulted in reduced thermal heating. This is visualized in a study that showed the different areas of plume production after each area of ablation following movement of the scanning beam. Central islands have not been reported in these systems. The smaller ablation size of the scanning laser consequently results in a longer operating time. Maintaining fixation has always been a problem for these scanning lasers, especially with the longer operating time, which results from more ablations by the smaller beams. Moreover, precise pulse-to-pulse registration of the scan is necessary to achieve a smooth and accurate final pattern. Automatic tracking devices are provided standard in these devices.
Manufacturers of scanning slit systems include the following: Autonomous (Orlando, FL), LaserSite (Orlando, FL), Meditec (Aesculap-Meditec, Heroldsberg, Germany) [9, 10] , Nidek (Fremont, CA) [11, 12, 13, 14, 15, 16] , Novatec (Carlsbad, CA), and Technolas (Chiron Vision Corp, Irvine, CA). Novatec's claim to fame is its use of solid-state laser crystals that obviates the need for argon fluoride gas to create its shorter ultraviolet beam. The Food and Drug Administration (FDA) has approved only the Summit and the VISX laser systems for commercial use within the United States. All the other systems are being used in other countries. [17]
PRK variations
The current techniques for surface treatments (eg, PRK, PARK, LASEK, epithelial scrubber assisted PRK, epi-LASIK) are sometimes collectively termed advanced surface ablation (ASA).
LASEK
Surface ablation resurgence was primarily assisted by the introduction of LASEK. The authors believe that LASEK is an improvement of the existing PARK technique. LASEK uses a sterile diluted alcohol solution to separate a viable sheet of corneal epithelium, fashioning a flap that can be rolled back after excimer laser ablation. Several advantages have been identified upon performing this procedure, as follows:
-
No blade technique for refractive surgery
-
Corneal tissue sparing
-
Less postoperative pain as compared to PARK
-
Less postoperative corneal haze as compared to PARK [18]
Epithelial scrubber assisted photorefractive keratotomy
The use of an Amoils epithelial scrubber allows fast and accurate epithelial removal, leaving a smoother anterior stromal surface. [19] The quick and efficient epithelial removal in less time decreases the potential for corneal dehydration to occur. It produces an easily seen bull’s eye that aids in centration of the laser application. Less epithelium is removed, resulting in faster healing time.
Epi-LASIK
The use of an epikeratome (plastic blade) mechanically sliding over the surface of the cornea, just underneath the epithelial layer of cells, while suction is applied, has resulted in another technique, which is basically automated LASEK without alcohol. [20, 21, 22]
History of the Procedure
The history of surgical treatment for astigmatism dates back to the late 1800s. Certain milestones in the development of this procedure can be attributed to several individuals, and a number of parallel procedures were in development at certain time periods.
In 1885, Schiotz performed limbal incision in the steep meridian to reduce iatrogenic astigmatism. Faber performed anterior transverse incisions to reduce idiopathic astigmatism. Lucciola also performed nonperforating corneal incisions to correct astigmatism. In 1894, Bates postulated that corneal incisions made at right angles to steeper meridians might correct astigmatism. Later, Lans showed that flattening in the meridian perpendicular to a transverse incision was associated with steepening in the orthogonal meridian and that a greater effect may be achieved with deeper and longer incisions.
In the 1940s, Sato began an extensive investigation of radial and astigmatic keratotomy. [23] Fyodorov is responsible for presenting several nonperforating anterior keratotomy patterns.
Modern techniques for astigmatic keratotomy are attributed to the works of Nordan, Thornton, and Nichamin. Nordan advocated a simple method of straight transverse keratotomy, with a target correction of 1-4 diopters (D). Thornton proposed a technique that included up to 3 pairs of arcuate incisions in varying optical zone sizes and with consideration of age and timing after surgery, respectively. [24] Nichamin developed an extensive nomogram for astigmatic keratotomy at the time of cataract surgery, although this technique has been modified by the use of a limbal relaxing incision during cataract surgery. Consequently, Troutman, who fancied wedge resection for reduction of postcorneal transplant astigmatism, developed another technique of astigmatism reduction.
Increased interest in using lasers to ablate tissue occurred in the late 1980s. The excimer laser initially was developed to etch out inscriptions on microchips. The postulated application of controlled ablation on corneal tissue led to its use in refractive correction.
In the late 1990s, wavefront aberrometry promised both physicians and patients the potential to achieve the so-called supervision. Initially used by astronomers, this wavefront technology reduced unwanted wavefront distortions in the creation of land-based telescopes.
Problem
Refractive errors (ie, myopia, hyperopia, astigmatism) can decrease visual acuity. [25] Astigmatism is a more challenging entity because it is determined by regularity, amount, and orientation. It also is more difficult to treat than myopia or hyperopia.
The quest to treat astigmatism began with the use of nonsurgical devices, including spectacles and contact lenses. These nonsurgical devices were followed by surgical techniques involving astigmatic keratotomy, compression sutures, and wedge resection. Newer surgical procedures include the use of intracorneal ring segments, PARK, LASIK, and LASEK, with or without wavefront-guided technology.
Epidemiology
Frequency
The frequency of astigmatism has a wide range of values as presented in modern literature. Naturally occurring (idiopathic) astigmatism is common. Surgically induced (iatrogenic) astigmatism is less common yet more problematic. [26, 27]
Clinically detectable refractive astigmatism reportedly is present in as many as 9 out of 10 eyes. However, refractive astigmatism in most of these eyes would not be clinically significant. The incidence of clinically significant astigmatism has been reported to be 7.5-75%, a wide range that primarily depends on the specific study and an author's definitions. Studies have estimated that approximately 44% of the population has more than 0.50 D of astigmatism, 10% of the population has more than 1.00 D, and 8% of the population has 1.50 D or more.
Etiology
Aside from the previously mentioned idiopathic astigmatism that is present, iatrogenic astigmatism may result after surgery. Visually significant refractive astigmatism is fairly common after different kinds of ophthalmic surgery, including cataract extraction, lamellar or penetrating keratoplasty, other corneal and anterior segment surgeries, and trabeculectomy. [28, 29, 30, 31, 32, 33]
Reportedly, astigmatism of at least 1.00 D often results after extracapsular cataract extraction, and astigmatism of at least 3.00 D is present in as many as 20% of cases with 10-mm incisions. Even phacoemulsification procedures, using the clear cornea technique, reportedly cause postoperative astigmatism, thereby guiding the cataract surgeon as to the proper placement of the corneal approach. High astigmatism can occur after penetrating keratoplasty.
Pathophysiology
The means of ablation of the excimer laser seem to be photochemical in type. This removal of tissue is called photochemical ablation or ablative photodecomposition. Photochemical ablation is an extremely confined tissue interaction centered on the fact that every photon created by the ArF excimer laser has 6.4 eV of energy, which is sufficient to split covalent bonds.
The intramolecular bonds of uncovered organic macromolecules are split when a sufficient number of high-energy, 193-nm photons are absorbed in a brief period. The resulting fragments rapidly expand and are ejected from the exposed surface at supersonic velocities observed under high-resolution magnification as the plume effect. This is the reason why only the irradiated organic materials are affected and the adjacent areas are not affected.
Presentation
A patient with astigmatism may complain of shadowing, bending, loss of contrast, and distortion. Astigmatism is believed to be the most common cause of ametropia. In mild cases, it may cause blurring of vision and ghosting. In more advanced cases of untreated astigmatism, amblyopia may be noted. [34] Astigmatism may occur naturally (idiopathic) or secondary to surgical procedures (iatrogenic), such as cataract extraction and penetrating keratoplasty. Several clinical procedures may be performed to detect astigmatism. These procedures include automated and/or manifest refraction, keratometry, Placido ring reflections, corneal topography, and wavefront aberrometry.
Indications
According to a November 2000 press release, the FDA approved the VISX Star Excimer Laser System for photorefractive keratectomy (PRK) for reduction or elimination of the following:
-
Myopia between 0 and -12.0 D with up to -4.0 D of astigmatism
-
Hyperopia between +1.0 D and +6.0 D with no more than 1.0 D refractive astigmatism
-
Hyperopia between +0.5 and +5.0 D of sphere at the spectacle plane with refractive astigmatism from +0.5 to +4.0 D with a maximum manifest refraction spherical equivalent of +6.0 D
PRK is an elective procedure with alternatives, including eyeglasses, contact lenses, and other refractive surgeries. [35, 36, 37]
Despite the clear-cut indications released by the FDA, several authorities and high-volume surgeons in and out of the United States are continuing to challenge the guidelines. An increasing number of presentations are being made at conventions and in journals stating the success achieved in cases performed beyond that which is listed in the FDA guidelines.
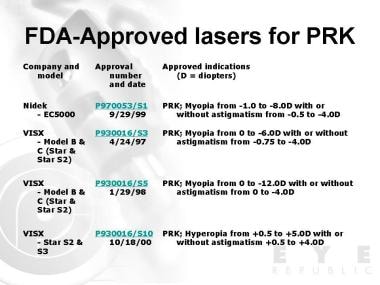
The images below illustrate current FDA-approved lasers for PRK and other refractive surgeries.
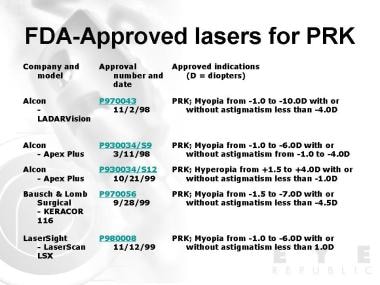 Food and Drug Administration (FDA)-approved lasers for photorefractive keratectomy (PRK). Adapted from US Food and Drug Administration - Center for Devices and Radiological Health - LASIK Eye Surgery.
Food and Drug Administration (FDA)-approved lasers for photorefractive keratectomy (PRK). Adapted from US Food and Drug Administration - Center for Devices and Radiological Health - LASIK Eye Surgery.
 Food and Drug Administration (FDA)-approved lasers for photorefractive keratectomy (PRK). Adapted from US Food and Drug Administration - Center for Devices and Radiological Health - LASIK Eye Surgery.
Food and Drug Administration (FDA)-approved lasers for photorefractive keratectomy (PRK). Adapted from US Food and Drug Administration - Center for Devices and Radiological Health - LASIK Eye Surgery.
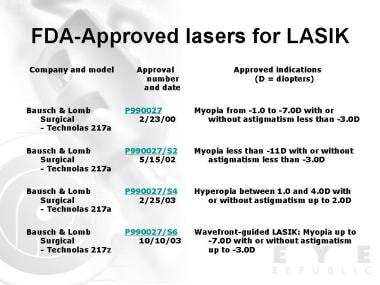
The images below outline current FDA-approved lasers for LASIK with or without astigmatism.
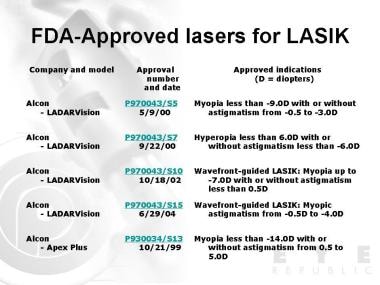 Food and Drug Administration (FDA)-approved lasers for laser in situ keratomileusis (LASIK) with or without astigmatism. Adapted from US Food and Drug Administration - Center for Devices and Radiological Health - LASIK Eye Surgery.
Food and Drug Administration (FDA)-approved lasers for laser in situ keratomileusis (LASIK) with or without astigmatism. Adapted from US Food and Drug Administration - Center for Devices and Radiological Health - LASIK Eye Surgery.
 Food and Drug Administration (FDA)-approved lasers for laser in situ keratomileusis (LASIK) with or without astigmatism. Adapted from US Food and Drug Administration - Center for Devices and Radiological Health - LASIK Eye Surgery.
Food and Drug Administration (FDA)-approved lasers for laser in situ keratomileusis (LASIK) with or without astigmatism. Adapted from US Food and Drug Administration - Center for Devices and Radiological Health - LASIK Eye Surgery.
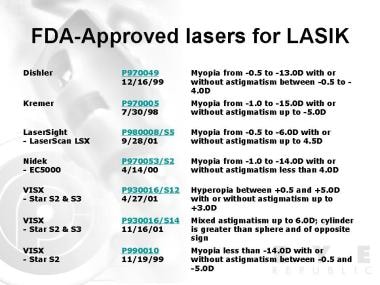 Food and Drug Administration (FDA)-approved lasers for laser in situ keratomileusis (LASIK) with or without astigmatism. Adapted from US Food and Drug Administration - Center for Devices and Radiological Health - LASIK Eye Surgery.
Food and Drug Administration (FDA)-approved lasers for laser in situ keratomileusis (LASIK) with or without astigmatism. Adapted from US Food and Drug Administration - Center for Devices and Radiological Health - LASIK Eye Surgery.
Relevant Anatomy
The cornea is a transparent, avascular tissue that is continuous with the opaque sclera and semitransparent conjunctiva. It is covered by tear film on its anterior surface and bathed by aqueous humor on its posterior surface. In adults, the cornea measures 11-12 mm horizontally and 9-11 mm vertically. The average corneal thickness is 0.5 mm (500 µm) centrally and 0.7 mm (700 µm) peripherally.
Contraindications
Contraindications to PRK are similar to those of LASIK and other refractive surgery procedures. PRK is contraindicated in patients with collagen, vascular, autoimmune, or immunodeficiency diseases; those with signs of keratoconus; patients taking isotretinoin or amiodarone hydrochloride; or those who are pregnant or breastfeeding.
PRK is not recommended in patients with a history of ophthalmic herpes simplex or herpes zoster.
Caution should be undertaken in deciding to perform PRK or other refractive surgery procedures on patients with systemic diseases (eg, connective tissue disease, diabetes, severe atopic disease, immunocompromised status) that are likely to affect wound healing. Safety and efficacy have not been established for these patient populations.
Despite these contraindications, non-recommendations, and cautions, several high-volume surgeons continue to "push the envelope" and perform these procedures beyond the FDA guidelines. Several reports exist of procedures performed on patients with forme fruste keratoconus and amiodarone toxicity.
Prognosis
Around 90% of people who undergo PRK, with or without astigmatism correction, achieve at least 20/40 vision without spectacle correction or contact lenses.
Patient Education
All patients considering PRK laser vision correction are shown animation videos on PRK before their suitability screening and counseling visits.
-
Food and Drug Administration (FDA)-approved lasers for photorefractive keratectomy (PRK). Adapted from US Food and Drug Administration - Center for Devices and Radiological Health - LASIK Eye Surgery.
-
Food and Drug Administration (FDA)-approved lasers for photorefractive keratectomy (PRK). Adapted from US Food and Drug Administration - Center for Devices and Radiological Health - LASIK Eye Surgery.
-
Food and Drug Administration (FDA)-approved lasers for laser in situ keratomileusis (LASIK) with or without astigmatism. Adapted from US Food and Drug Administration - Center for Devices and Radiological Health - LASIK Eye Surgery.
-
Food and Drug Administration (FDA)-approved lasers for laser in situ keratomileusis (LASIK) with or without astigmatism. Adapted from US Food and Drug Administration - Center for Devices and Radiological Health - LASIK Eye Surgery.
-
Food and Drug Administration (FDA)-approved lasers for laser in situ keratomileusis (LASIK) with or without astigmatism. Adapted from US Food and Drug Administration - Center for Devices and Radiological Health - LASIK Eye Surgery.
-
Food and Drug Administration (FDA)-approved lasers for laser in situ keratomileusis (LASIK) with or without astigmatism. Adapted from US Food and Drug Administration - Center for Devices and Radiological Health - LASIK Eye Surgery.
-
Astigmatic ablation profile. Image courtesy of Manolette Roque, MD, Ophthalmic Consultants Philippines Co, EYE REPUBLIC Ophthalmology Clinic.
-
Myopic ablation profile. Image courtesy of Manolette Roque, MD, Ophthalmic Consultants Philippines Co, EYE REPUBLIC Ophthalmology Clinic.
-
Hyperopic ablation profile. Image courtesy of Manolette Roque, MD, Ophthalmic Consultants Philippines Co, EYE REPUBLIC Ophthalmology Clinic.
-
Technolas 217z excimer laser. Digital photo published with permission from Bausch & Lomb Surgical Philippines.
-
Orbscan IIz. Digital photo published with permission from Bausch & Lomb Surgical Philippines.
-
ZyWave wavefront aberrometer. Digital photo published with permission from Bausch & Lomb Surgical Philippines.
-
ZyWave wavefront aberrometer user interface. Digital photo published with permission from Bausch & Lomb Surgical Philippines.
-
Fixation with ZyWave wavefront aberrometer. Digital photo published with permission from Bausch & Lomb Surgical Philippines.











