Kelly JP, Feldman KW, Wright JN, Metz JB, Weiss A. Pediatric abusive head trauma: visual outcomes, evoked potentials, diffusion tensor imaging, and relationships to retinal hemorrhages. Doc Ophthalmol. 2023 Aug. 147 (1):1-14. [QxMD MEDLINE Link]. [Full Text].
Haas J. Ueber das Zusammenvorkommen von Veranderungen der Retina und Choroidea. Arch Augenheilkd. 1898. 37:343-48.
Pagenstecher HE. Ueber eine unter dem Bilde der Natzhauterblosung verlaufende, erbliche Erkrankung der Retina. Graefes Arch Ophthalmol. 1913. 86:457-6.
Anderson JR. nterior dialysis of the retina: disinsertion or avulsion at ora serrata. BrJ Ophthalmol. 1932. 16:641-70.
Thomson E. Memorandum regarding a family in which neuroretinal disease of an unusual kind occurred only in males. Br Ophthalmol. 1932. 16:681-86.
Magnus JA. Case of retinal detachment in a child (?cystic ?congenital). Trans Ophthalmol Soc UK. 1951. 71:728-30.
Mann I, Macrae A. Congenital vascular veils in the vitreous. BrJ Ophthalmol. 1938. 22:1-10.
Sauer CG, Gehrig A, Warneke-Wittstock R, et al. Positional cloning of the gene associated with X-linked juvenile retinoschisis. Nat Genet. 1997 Oct. 17(2):164-70. [QxMD MEDLINE Link].
Lee JJ, Kim JH, Kim SY, Park SS, Yu YS. Infantile vitreous hemorrhage as the initial presentation of X-linked juvenile retinoschisis. Korean J Ophthalmol. 2009 Jun. 23(2):118-20. [QxMD MEDLINE Link]. [Full Text].
Piquin G, Abdelmassih Y, Martin G, Edelson C, Metge F, Caputo G, et al. SYMPTOMATIC EARLY-ONSET X-LINKED RETINOSCHISIS: Clinical Presentation and Outcomes. Retina. 2023. 43:348-55. [QxMD MEDLINE Link].
Sikkink SK, Biswas S, Parry NR, Stanga PE, Trump D. X-linked retinoschisis: an update. J Med Genet. 2007 Apr. 44 (4):225-32. [QxMD MEDLINE Link].
George NDL, Yates JRW, Moore AT. Clinical Features in Affected Males With X-Linked Retinoschisis. Arch Ophthalmol. 1996. 14:274–80.
Regillo CD, Custis PH. Surgical management of retinoschisis. Curr Opin Ophthalmol. 1997 Jun. 8(3):80-6. [QxMD MEDLINE Link].
Hung JY, Hilton GF. Neovascular glaucoma in a patient with X-linked juvenile retinoschisis. Ann Ophthalmol. 1980. 12:1054-55.
Yan W, Wang Y, Ye Q, Chen X, Chen Y, Jiang C, et al. The electrophysiological features of X-linked juvenile retinoschisis in a young male: a case report. J Int Med Res. 2022. 50(1):[QxMD MEDLINE Link]. [Full Text].
Sieving PA, MacDonald IM, Hoang S; In: Adam MP, Mirzaa GM, Pagon RA, et al. X-Linked Congenital Retinoschisis. GeneReviews. Available at https://www.ncbi.nlm.nih.gov/books/NBK1222/. 1993-2003; Accessed: July 25, 2023.
Fenner Beau J., Russell Jonathan F., Drack Arlene V., Dumitrescu Alina V., Sohn Elliott H., Russell Stephen R., et al. Long-term functional and structural outcomes in X-linked retinoschisis: implications for clinical trials. Frontiers in Medicine. 2023. 10:[Full Text].
Huang WC, Liu PK, Wang NK. Electroretinogram (ERG) to Evaluate the Retina in Cases of Retinitis Pigmentosa (RP). Methods Mol Biol. 2023. 2560:111-22.
Jiang, X., Mahroo, O.A. Negative electroretinograms: genetic and acquired causes, diagnostic approaches and physiological insights. Eye. 2021. 35:2419-437. [Full Text].
Georgiou, M., Finocchio, L., Fujinami, K., et al. X-Linked Retinoschisis Deep Phenotyping and Genetic Characterization. Ophthalmology. 2022. 129:542-51. [Full Text].
Genead MA, Fishman GA, Walia S. Efficacy of sustained topical dorzolamide therapy for cystic macular lesions in patients with x-linked retinoschisis. Arch Ophthalmol. 2010 Feb. 128(2):190-7. [QxMD MEDLINE Link].
Ambrosio L, Williams JS, Gutierrez A, Swanson EA, Munro RJ, Ferguson RD, et al. Carbonic anhydrase inhibition in X-linked retinoschisis: An eye on the photoreceptors. Exp Eye Res. 2021. [QxMD MEDLINE Link].
Cukras CA, Wiley HE, Jeffrey BG, Sen HN, Turriff A, Zeng Y, et al. Retinal AAV8-RS1 gene therapy for X-linked retinoschisis: initial findings from a Phase I/IIa trial by intravitreal delivery. Mol Ther. 2018. 26:2282-94. [QxMD MEDLINE Link].
Mishra A, Vijayasarathy C, Cukras CA, Wiley HE, Sen HN, Zeng Y, et al. Immune function in X-linked retinoschisis subjects in an AAV8-RS1 phase I/IIa gene therapy trial. Mol Ther. 2021. 29:2030-40. [QxMD MEDLINE Link].
Rishi E, Gopal L, Rishi P, Deshmukh H. Congenital x-linked retinoschisis: a novel approach for management of a large schitic cavity overhanging the macula. Retin Cases Brief Rep. 2009. 3:105-7. [QxMD MEDLINE Link].
Molday RS, Kellner U, Weber BH. X-linked juvenile retinoschisis: clinical diagnosis, genetic analysis, and molecular mechanisms. Prog Retin Eye Res. 2012 May. 31 (3):195-212. [QxMD MEDLINE Link].
Apushkin MA, Fishman GA. Use of dorzolamide for patients with X-linked retinoschisis. Retina. 2006 Sep. 26(7):741-5. [QxMD MEDLINE Link].
Apushkin MA, Fishman GA, Rajagopalan AS. Fundus findings and longitudinal study of visual acuity loss in patients with X-linked retinoschisis. Retina. 2005 Jul-Aug. 25(5):612-8. [QxMD MEDLINE Link].
Bergen AA, ten Brink JB, van Schooneveld MJ. Efficient DNA carrier detection in X linked juvenile retinoschisis. Br J Ophthalmol. 1995 Jul. 79(7):683-6. [QxMD MEDLINE Link].
Brucker AJ, Spaide RF, Gross N, Klancnik J, Noble K. Optical coherence tomography of X-linked retinoschisis. Retina. 2004 Feb. 24(1):151-2. [QxMD MEDLINE Link].
Dahl N, Pettersson U. Use of linked DNA probes for carrier detection and diagnosis of X-linked juvenile retinoschisis. Arch Ophthalmol. 1988 Oct. 106(10):1414-6. [QxMD MEDLINE Link].
Forsius HJ, Vainio-Mattila B, Erikson A. X-linked hereditary retinoschisis. Br J Ophthalmol. 1962. 46:678-681.
Gao H, Kusumi R, Yung CW. Optical coherence tomographic findings in X-linked juvenile retinoschisis. Arch Ophthalmol. 2005 Jul. 123(7):1006-8. [QxMD MEDLINE Link].
Gehrig AE, Warneke-Wittstock R, Sauer CG, Weber BH. Isolation and characterization of the murine X-linked juvenile retinoschisis (Rs1h) gene. Mamm Genome. 1999 Mar. 10(3):303-7. [QxMD MEDLINE Link].
Ghajarnia M, Gorin MB. Acetazolamide in the treatment of X-linked retinoschisis maculopathy. Arch Ophthalmol. 2007 Apr. 125(4):571-3. [QxMD MEDLINE Link].
Greene JM, Shakin EP. Optical coherence tomography findings in foveal schisis. Arch Ophthalmol. 2004 Jul. 122(7):1066-7. [QxMD MEDLINE Link].
Helve J. Colour vision in X-chromosomal juvenile retinoschisis. Mod Probl Ophthal. 1971. 11:122-129.
Ide CH, Wilson RJ. Juvenile retinoschisis. Br J Ophthalmol. 1973 Aug. 57(8):560-2. [QxMD MEDLINE Link].
Joshi MM, Drenser K, Hartzer M, Dailey W, Capone A Jr, Trese MT. Intraschisis cavity fluid composition in congenital X-linked retinoschisis. Retina. 2006 Sep. 26(7 Suppl):S57-60. [QxMD MEDLINE Link].
Kjellstrom S, Bush RA, Zeng Y, Takada Y, Sieving PA. Retinoschisin gene therapy and natural history in the Rs1h-KO mouse: long-term rescue from retinal degeneration. Invest Ophthalmol Vis Sci. 2007 Aug. 48(8):3837-45. [QxMD MEDLINE Link].
Li X, Ma X, Tao Y. Clinical features of X linked juvenile retinoschisis in Chinese families associated with novel mutations in the RS1 gene. Mol Vis. 2007. 13:804-12. [QxMD MEDLINE Link].
Manschot WA. Pathology of hereditary juvenile retinoschisis. Arch Ophthalmol. 1972 Aug. 88(2):131-8. [QxMD MEDLINE Link].
McMahon TT, Rosenthal BP. X-linked juvenile retinoschisis. J Am Optom Assoc. 1983 Jan. 54(1):55-61. [QxMD MEDLINE Link].
Min SH, Molday LL, Seeliger MW, et al. Prolonged recovery of retinal structure/function after gene therapy in an Rs1h-deficient mouse model of x-linked juvenile retinoschisis. Mol Ther. 2005 Oct. 12(4):644-51. [QxMD MEDLINE Link].
Molday LL, Hicks D, Sauer CG, Weber BH, Molday RS. Expression of X-linked retinoschisis protein RS1 in photoreceptor and bipolar cells. Invest Ophthalmol Vis Sci. 2001 Mar. 42(3):816-25. [QxMD MEDLINE Link].
Pawar H, Bingham EL, Hiriyanna K, Segal M, Richards JE, Sieving PA. X-linked juvenile retinoschisis: localization between (DXS1195, DXS418) and AFM291wf5 on a single YAC. Hum Hered. 1996 Nov-Dec. 46(6):329-35. [QxMD MEDLINE Link].
Peachey NS, Fishman GA, Derlacki DJ, Brigell MG. Psychophysical and electroretinographic findings in X-linked juvenile retinoschisis. Arch Ophthalmol. 1987 Apr. 105(4):513-6. [QxMD MEDLINE Link].
Reid SN, Yamashita C, Farber DB. Retinoschisin, a photoreceptor-secreted protein, and its interaction with bipolar and muller cells. J Neurosci. 2003 Jul 9. 23(14):6030-40. [QxMD MEDLINE Link].
Sabates FN. Juvenile retinoschisis. Am J Ophthalmol. 1966 Oct. 62(4):683-8. [QxMD MEDLINE Link].
Shastry BS, Hejtmancik FJ, Margherio RT, Trese MT. Linkage mapping of new X-linked juvenile retinoschisis kindreds using microsatellite markers. Biochem Biophys Res Commun. 1996 Mar 27. 220(3):824-7. [QxMD MEDLINE Link].
Shimazaki J, Matsuhashi M. Familial retinoschisis in female patients. Doc Ophthalmol. 1987 Mar. 65(3):393-400. [QxMD MEDLINE Link].
Souied EH, Goritsa A, Querques G, Coscas G, Soubrane G. Indocyanine green angiography of juvenile X-linked retinoschisis. Am J Ophthalmol. 2005 Sep. 140(3):558-61. [QxMD MEDLINE Link].
Suganthalakshmi B, Shukla D, Rajendran A, Kim R, Nallathambi J, Sundaresan P. Genetic variations in the hotspot region of RS1 gene in Indian patients with juvenile X-linked retinoschisis. Mol Vis. 2007. 13:611-7. [QxMD MEDLINE Link].
Tantri A, Vrabec TR, Cu-Unjieng A, Frost A, Annesley WH Jr, Donoso LA. X-linked retinoschisis: a clinical and molecular genetic review. Surv Ophthalmol. 2004 Mar-Apr. 49(2):214-30. [QxMD MEDLINE Link].
Teixeira C, Rocha-Sousa A, Trump D, Brandao E, Falcao-Reis F. Identification of XLRS1 gene mutation (608C > T) in a Portuguese family with juvenile retinoschisis. Eur J Ophthalmol. 2005 Sep-Oct. 15(5):638-40. [QxMD MEDLINE Link].
The Retinoschisis Consortium. Functional implications of the spectrum of mutations found in 234 cases with X-linked juvenile retinoschisis. Hum Mol Genet. 1998 Jul. 7(7):1185-92. [QxMD MEDLINE Link].
Trese MT, Ferrone PJ. The role of inner wall retinectomy in the management of juvenile retinoschisis. Graefes Arch Clin Exp Ophthalmol. 1995 Nov. 233(11):706-8. [QxMD MEDLINE Link].
Verdaguer J. Juvenile retinal detachment. Pan American Association of Ophthalmology and American Journal of Ophthalmology Lecture. Am J Ophthalmol. 1982 Feb. 93(2):145-56. [QxMD MEDLINE Link].
Wu G, Cotlier E, Brodie S. A carrier state of X-linked juvenile retinoschisis. Ophthalmic Paediatr Genet. 1985 Feb. 5(1-2):13-7. [QxMD MEDLINE Link].
Wu WW, Molday RS. Defective discoidin domain structure, subunit assembly, and endoplasmic reticulum processing of retinoschisin are primary mechanisms responsible for X-linked retinoschisis. J Biol Chem. 2003 Jul 25. 278(30):28139-46. [QxMD MEDLINE Link].
Yanoff M, Kertesz Rahn E, Zimmerman LE. Histopathology of juvenile retinoschisis. Arch Ophthalmol. 1968 Jan. 79(1):49-53. [QxMD MEDLINE Link].
Yassur Y, Nissenkorn I, Ben-Sira I, Kaffe S, Goodman RM. Autosomal dominant inheritance of retinoschisis. Am J Ophthalmol. 1982 Sep. 94(3):338-43. [QxMD MEDLINE Link].
Zeng Y, Takada Y, Kjellstrom S, et al. RS-1 Gene Delivery to an Adult Rs1h Knockout Mouse Model Restores ERG b-Wave with Reversal of the Electronegative Waveform of X-Linked Retinoschisis. Invest Ophthalmol Vis Sci. 2004 Sep. 45(9):3279-85. [QxMD MEDLINE Link].
Alitalo T, Kruse TA, de la Chapelle A. Refined localization of the gene causing X-linked juvenile retinoschisis. Genomics. 1991 Mar. 9(3):505-10. [QxMD MEDLINE Link].
Molday RS, Kellner U, Weber BH. X-linked juvenile retinoschisis: clinical diagnosis, genetic analysis, and molecular mechanisms. Prog Retin Eye Res. 2012 May. 31(3):195-212. [QxMD MEDLINE Link].
Delgado D, del Pozo-Rodriguez A, Solinis MA, et al. Dextran and protamine-based solid lipid nanoparticles as potential vectors for the treatment of X-linked juvenile retinoschisis. Hum Gene Ther. 2012 Apr. 23(4):345-55. [QxMD MEDLINE Link].
Byrne LC, Oztürk BE, Lee T, Fortuny C, Visel M, Dalkara D, et al. Retinoschisin gene therapy in photoreceptors, Müller glia or all retinal cells in the Rs1h-/- mouse. Gene Ther. 2014 Jun. 21(6):585-92. [QxMD MEDLINE Link]. [Full Text].
Retinopathy of Prematurity. Children's Eye Site- University of Iowa Hospital and Stead Family Children's Hospital. Available at https://childrenseye.org/home/images/. 2023; Accessed: September 20, 2023.
Fenner BJ, Russell JF, Drack AV, Dumitrescu AV, Sohn EH, Russell SR, et al. Long-term functional and structural outcomes in X-linked retinoschisis: implications for clinical trials. Front Med (Lausanne). 2023. 10:1204095. [QxMD MEDLINE Link]. [Full Text].
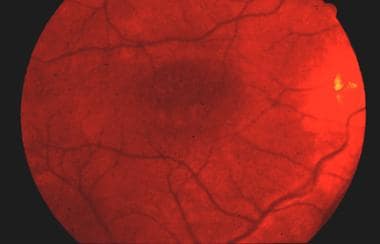 Fundus photograph of juvenile retinoschisis demonstrating stellate spokelike appearance with microcysts.
Fundus photograph of juvenile retinoschisis demonstrating stellate spokelike appearance with microcysts.






