Background
Phacoanaphylaxis/lens-induced uveitis occurs in the setting of a ruptured or degenerative lens capsule and is characterized by a granulomatous antigenic reaction to lens protein. [1, 2, 3, 4, 5, 6] Before the modern era of microsurgery, this disease was more common, and the diagnosis was often made histologically, as eyes with phacoanaphylaxis were often enucleated for intractable inflammation and secondary glaucoma. [7, 8, 9]
With improved microsurgical techniques, especially with the introduction of extracapsular cataract extraction and phacoemulsification, the incidence of phacoanaphylaxis has decreased dramatically and rarely occurs in its originally described form. However, chronic postoperative uveitis following phacoemulsification with retained lens material is still a well-known complication of cataract surgery and is the result of the same pathophysiology as the classically described entity of phacoanaphylaxis. [10, 11]
While lens fragments may be retained in the anterior or posterior chamber during seemingly uncomplicated cataract surgery, they also may be dislocated posteriorly into the vitreous cavity during phacoemulsification of the nucleus, usually after zonular dehiscence or posterior capsule rupture. Lens-induced uveitis may develop, and the degree of intraocular inflammation in these patients often is governed by the size of the retained lens fragment, the time since cataract surgery, the patient's individual inflammatory response, and the extent of other intraocular manipulations.
Pathophysiology
Lens proteins are most likely immunologically privileged, and they may initiate an immunologic sensitization only after entering the aqueous humor. This privilege is probably because of numerous factors, as follows: lens proteins are isolated from the fetal circulation early in embryonic life, the lens is devoid of innervation, and the adult lens is completely avascular. However, the immunopathogenesis of lens-induced uveitis is not precisely understood.
Antigenicity of lens proteins
The lens is an epithelial structure as it is derived from primitive ectoderm. By virtue of its capacity to synthesize alpha crystallins, the lens epithelium may become strongly antigenic. [12, 13, 14, 15, 16, 17, 18, 19] The protein concentration within the lens is higher than that of any other tissue in the body.
Early experiments inferred that lens antigens are shared among a number of animal species, and they can provoke the formation of homologous antibodies. [16, 20] Halbert et al found that lens proteins might be autoantigenic when they escape from their position of immunological isolation in the lens capsule. [21] Each of the crystallin protein groups of lens cortical fibers contains a number of subtypes with distinct antigenic characteristics. Autologous lens proteins are only weakly antigenic, but fractionated crystallins are much more effective in stimulating an antibody response. The conversion process from soluble crystallins to insoluble proteins during aging of the lens also may result in an increased antigenic effect of proteins from mature or hypermature cataracts.
Histopathology
The classic histologic picture is one of zonal granulomatous inflammation. [22, 12, 21, 23, 24] Polymorphonuclear leukocyte infiltration around degenerate lens remnants is surrounded by a palisade of macrophages, including epithelioid cells and multinucleated giant cells (see the images below).
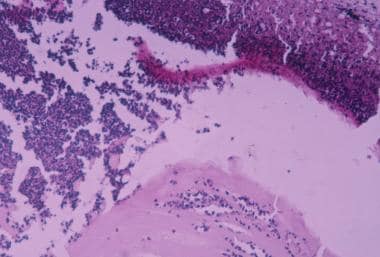 Gross photomicrograph for eye enucleated with penetrating injury. Note marked inflammatory reaction consisting of polymorphonuclear cells around lens capsule and lens fibers (hematoxylin and eosin X100).
Gross photomicrograph for eye enucleated with penetrating injury. Note marked inflammatory reaction consisting of polymorphonuclear cells around lens capsule and lens fibers (hematoxylin and eosin X100).
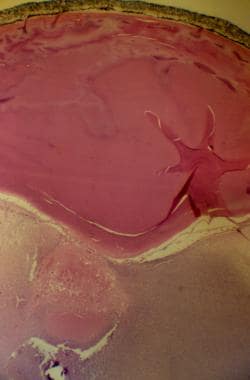 Low (X25) photomicrograph of phacoanaphylactic reaction to lens protein in eye enucleated with penetrating injury. Note polymorphonuclear leucocytes around lens protein (hematoxylin and eosin).
Low (X25) photomicrograph of phacoanaphylactic reaction to lens protein in eye enucleated with penetrating injury. Note polymorphonuclear leucocytes around lens protein (hematoxylin and eosin).
Eosinophils may be prominent, and, eventually, fibroblastic granulation tissue develops together with prominent lymphocyte and plasma cell infiltration. The uveitis principally affects the iris, with the choroid being only secondarily involved. Retinal perivasculitis and papillitis may develop because of the presence of cross-reacting antigens in these tissues. Although a zonal granulomatous inflammation is the classic histopathologic description, a nongranulomatous uveitis also has been observed (see the image below).
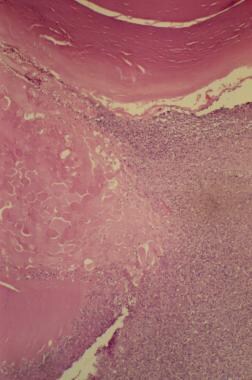 High (X50) photomicrograph of phacoanaphylactic reaction to lens protein in eye enucleated with penetrating injury. Note polymorphonuclear leucocytes around lens protein (hematoxylin and eosin).
High (X50) photomicrograph of phacoanaphylactic reaction to lens protein in eye enucleated with penetrating injury. Note polymorphonuclear leucocytes around lens protein (hematoxylin and eosin).
Pathogenesis
The term phacoanaphylaxis is probably inappropriate because no evidence exists of a classic type I immunoglobulin E (IgE) mediated anaphylactic reaction. The immunopathogenesis of lens-induced uveitis is believed to be the result of autosensitization to lens proteins. After a break in the lens capsule and sensitization to lens proteins, an immune complex–mediated phenomenon develops, which can be transferred by hyperimmune serum. Type II, III, and IV hypersensitivity reactions may be involved in the pathogenesis.
The disease most likely is induced by altered tolerance to lens protein and not as a result of a rejection phenomenon of sequestered foreign materials. The specific type of immunological reaction in lens-induced uveitis may vary from patient to patient, and it may depend on the type of surgery or injury, the amount of retained lens in the vitreous cavity, and the previous immunological status of both the patient and the eye.
Epidemiology
Frequency
International
The incidence of both phacoanaphylaxis and lens-induced uveitis is unknown. The best estimate of the incidence of posteriorly displaced lens fragments during phacoemulsification is 0.3-18% (the latter figure reported by a surgeon learning to use phacoemulsification). The incidence of retained lens fragments has increased as phacoemulsification has become more popular for cataract surgery. Although data are lacking, the authors' clinical impression is that about 50% of patients with retained lens material after cataract surgery have lens-induced uveitis. The incidence of lens-induced uveitis following penetrating injury is unknown.
Mortality/Morbidity
Lens-induced uveitis may cause or may be associated with cystoid macular edema, hypotony, phthisis, and secondary glaucoma. [25, 26, 27, 28] Complications also may be the result of medical or surgical treatment of lens-induced uveitis.
Race
No racial predilection exists.
Sex
No sexual predilection exists.
Age
Phacoanaphylactic endophthalmitis and lens-induced uveitis are more common in the elderly population, with a peak incidence in the sixth to seventh decades. The main exception is traumatic cataract and related complications, which are more common in younger age groups.
-
Gross photomicrograph for eye enucleated with penetrating injury.
-
Gross photomicrograph for eye enucleated with penetrating injury. Note marked inflammatory reaction consisting of polymorphonuclear cells around lens capsule and lens fibers (hematoxylin and eosin X100).
-
Low (X25) photomicrograph of phacoanaphylactic reaction to lens protein in eye enucleated with penetrating injury. Note polymorphonuclear leucocytes around lens protein (hematoxylin and eosin).
-
High (X50) photomicrograph of phacoanaphylactic reaction to lens protein in eye enucleated with penetrating injury. Note polymorphonuclear leucocytes around lens protein (hematoxylin and eosin).
-
Phacoanaphylactic reaction to penetrating injury of lens. This patient was a 25-year-old woman whose eye was penetrated with a 27-gauge needle during an attempt to anesthetize the eyelid for chalazion removal. One week later, a marked uveitis was present. Notice perforation site and posterior synechiae.
-
Same patient as in Media file 5. Notice cortical cataract at perforation site.
-
Typical clinical picture of retained lens material following cataract surgery. White cortical material is easily visible in the pupillary space.
-
Patient with persistently elevated intraocular pressure after cataract surgery was found to have retained lens material and low-grade inflammation. Eye is white and quiet with anterior chamber lens.
-
Patient with persistently elevated intraocular pressure after cataract surgery was found to have retained lens material and low-grade inflammation. Retained lens material is visible in retroillumination on downgaze.
-
Typical appearance of retained lens fragments in posterior vitreous cavity. Lens material is a whitish substance that obscures fundus details.
-
Another view of a retained lens fragment, noted inferiorly.








