Classification Systems
Uveitis is a condition that involves inflammation of the uveal tract (ie, iris, ciliary body, choroid) or adjacent ocular structures (eg, retina, optic nerve, vitreous, [1] sclera). In most cases, the etiology remains elusive and is often of an autoimmune nature. [2] In instances where the etiology is known, infectious agents or trauma are important causes. The differential diagnosis is extensive, and the epidemiology changes with the emergence of new uveitic entities.
Classification and standardization of uveitis is important, as it enhances the precision and comparability of clinical research from different centers and assists in the development of a complete picture of the course of the disorders and their response to treatment. [3]
The most widely used classification of uveitis is the one devised by the International Uveitis Study Group (IUSG) in 1987, based on the anatomical location of the inflammation. This classification includes anterior uveitis (iritis, iridocyclitis, and anterior cyclitis), intermediate uveitis (para planitis, posterior cyclitis, and hyalitis), and posterior uveitis (focal, multifocal, or diffuse choroiditis, chorioretinitis, retinitis, and neuroretinitis). An additional term, panuveitis (anterior chamber, vitreous, retina, and choroid), is also described.
The International Ocular Inflammation Society (IOIS) also published detailed clinical guidelines on anterior segment and posterior segment intraocular inflammation. [4, 5]
In 2005, the Standardization of Uveitis Nomenclature (SUN) Working Group standardized the methods for reporting clinical data (diagnostic terminology, inflammation grading schema, and outcome measures) for uveitis. There was a consensus by the group members that the anatomical classification of uveitis based on criteria defined by the International Uveitis Study Group (IUSG) should be used. A standardized grading schema for aspects of intraocular inflammation, that is, anterior chamber cells, anterior chamber flare, and vitreous haze, was developed. [6] Standardized definitions of outcomes, including reporting visual acuity outcomes, were approved. [7]
In 2008, the International Uveitis Study Group (IUSG) designed a simplified, clinical classification system for uveitis based on etiological criteria. It has 3 main categories, as follows: infectious (eg, bacterial, viral, fungal, parasitic), noninfectious (eg, known systemic associations, no known systemic associations), and masquerade (eg, neoplastic, nonneoplastic). [8]
The Standardization of Uveitis Nomenclature (SUN) Working Group met in 2009 to standardize the descriptions and terminologies necessary to develop tools such as computerized data entry forms and classification criteria. Initial terminology was developed via Web-based surveys, broadband Delphi techniques, and teleconferences. This terminology was then revised by workshop participants using nominal group techniques and supermajority voting. A total of 193 terms were identified and mapped to 28 major uveitic disease entities. [9, 10]
Classification Parameters
Uveitis may be classified according to numerous parameters, to include the following:
Patient demographics
Location of the inflammatory process
Duration, onset, and course of inflammation
Character of the inflammation, including the nature of the inflammatory cells and deposits, distribution of lesions, and the presence of nodules, fibrin, or synechiae
Etiology of the inflammation
The intellectual exercise of naming each parameter allows the clinician to focus upon those diagnoses most likely attributed to each patient's disease. Thus, a specifically tailored, cost-effective uveitis evaluation may be obtained to further process the differential for a given constellation of parameters.
The steps involved in the workup of a patient include naming, meshing, office testing, specific and nonspecific laboratory tests, specialty consultations, therapeutic tests, and diagnosis and treatment.
Naming
As with every patient, the initial source for determining the etiology of a patient's complaint involves an accurate history and a physical evaluation. The naming process creates a profile or template of the clinical case. A listing of uveitis classifications is included in Classification.
Naming example: Mrs. Jackson is a 32-year-old white schoolteacher from Virginia with a history of chronic bilateral diffuse granulomatous uveitis, headaches, hearing loss, and vitiligo. She has no known history of ocular trauma.
Naming breakdown: Patient identifier, age, race, occupation, duration, character of the inflammation, location of the inflammation, and associated symptoms.
Meshing
Meshing is the process of matching up the findings in the case in question with the clinical characteristics of known uveitic entities. In most cases, the list of likely uveitic entities is surprisingly small and covers 90% or more of uveitis cases seen in the general practice of ophthalmology.
By comparing patient parameters to established uveitic entities, similar profiles should be included in the preliminary differential diagnosis and then should be ranked in order of likelihood. Based on the previous clinical example, meshing would provide the following differential diagnoses: (1) Vogt-Koyanagi-Harada syndrome (VKH), (2) sarcoidosis, (3) Behcet syndrome, and (4) sympathetic ophthalmia.
Diagnosis
Based on the meshing process, a small list of differential diagnoses is generated.
Laboratory tests can be ordered to systematically evaluate each possible diagnosis. Other specialists can also be consulted to help elucidate the diagnosis by incorporating other systemic signs and symptoms. Many times, a diagnosis can be firmly established only if the patient actually responds to specific medical therapy, usually an antibiotic. The final goal of uveitic classification is a diagnosis, which, in turn, provides either specific therapeutic treatment or appropriate palliative anti-inflammatory therapy.
By using the naming-meshing system and by supplementing it with laboratory tests and consultations, 75-85% of patients with uveitis seen in general clinical practice can be diagnosed correctly. In the remaining cases, rarities and masquerade syndromes should be considered, and, if the resistance to appropriate therapy continues, the patient should be referred to a uveitis center.
The various parameters required in proper naming and classification of uveitis cases are described in the subsequent sections.
Patient Demographics
Demographic information provides essential data in formulating a differential diagnosis. Therefore, a thorough and comprehensive history is the most important component of the uveitis workup.
Age
The age of the patient often is helpful in focusing the differential diagnosis. For example, juvenile idiopathic arthritis (JIA), retinoblastoma, and toxocariasis arise predominantly in children. Fuchs heterochromic iridocyclitis, multiple sclerosis, Behcet syndrome, acute posterior multifocal placoid pigment epitheliopathy (APMPPE), and pars planitis occur most frequently in young adults. Reactive arthritis (also referred to as Reiter syndrome), ankylosing spondylitis, birdshot retinochoroidopathy, and VKH syndrome usually occur in middle-aged patients. Tuberculous and luetic uveitis may present at any age.
Sex
The sex of the patient may provide useful information. Uveitis associated with ankylosing spondylitis, Behcet syndrome, and reactive arthritis is more common in males, while uveitis associated with JIA more frequently occurs in females. Fungal endophthalmitis and sympathetic ophthalmia are more common in males due to either injury or intravenous drug use.
Race
The race of the patient may focus the differential even further. For example, human leukocyte antigen B27 (HLA-B27)–associated arthritides are more common in whites and include ankylosing spondylitis, psoriatic arthritis, and reactive arthritis. Sarcoidosis most commonly presents in blacks. VKH is seen mostly in patients of Asian and American Indian descent. Behcet syndrome is a disease of the ancient Eurasian silk route, from China to Turkey. However, most uveitic syndromes have no particular sexual or racial predilection.
Sexual habits
Sexual orientation may play a role in diagnosis, in that young, sexually active males are more likely to contract HIV and other AIDS-related infections, such as cytomegalovirus (CMV) retinitis, Kaposi sarcoma, or herpes zoster ophthalmicus. Sexually active individuals are also at increased risk of contracting a sexually transmitted disease, such as syphilis or gonorrhea, which may cause a primary uveitis, or chlamydia, which itself may trigger a HLA-B27-related uveitis.
Geographic history
When suspecting infectious etiologies of uveitis, it is wise to adequately address the geographic location and recent travel of the patient. The endemic nature of histoplasmosis within the Mississippi-Ohio-Missouri River valleys should make the ophthalmologist suspicious of this illness in patients from that area. Histoplasmosis also is relatively localized to the 45° north and 45° south latitudes worldwide. Coccidioidomycosis is found predominantly in the southwest United States.
Family history
Family history is important, as some diseases have a genetic predisposition or there may be a greater likelihood that a particular disease will develop by direct transmission from a family member. Inflammatory diseases, such as ankylosing spondylitis, reactive arthritis, and inflammatory bowel diseases, develop in families with HLA-B27. Ocular toxoplasmosis is usually a late result of congenital transmission. A history of infectious diseases (eg, tuberculosis) in a family is helpful when such an entity is suspected.
Social habits
A history of ingestion of raw or undercooked meat is important in arousing suspicion for ocular toxoplasmosis. Contact with feline feces containing oocytes of Toxoplasma gondii may occur by handling cat litter or by playing in sand boxes. If ocular toxocariasis is suspected, a history of contact with unwormed cats or dogs is important.
Contagious disease exposure
Leptospirosis infection has an increased incidence in sewer workers and in those with exposure to rodent urine. Other cases include a history of exposure to contaminated water. A history of exposure to a patient with active tuberculosis may assist in the diagnosis when tuberculosis is being considered as a possible cause of uveitis.
When sexually transmitted diseases, such as syphilis, AIDS, and reactive arthritis, are being considered, a directed sexual history, including inquiring about previous sexually transmitted diseases, genitourinary symptoms, and sexual practices, may obviate an expensive diagnostic workup. Additionally, a history of intravenous drug abuse may be useful in arriving at a smaller differential diagnosis.
Travel history
Travel and immigration are important components of the uveitis history. Presence in areas endemic to tuberculosis or dysentery may be directly related to a recent or recurrent ocular inflammatory episode. Areas considered endemic for recently popularized viral syndromes, such as West Nile virus in Africa, which has entered into the North American population pool since the 1999 New York outbreak, should also be considered. Recent travel from Brazil may suggest Zika virus infection, with more than one million Brazilians infected in 2015. [11] Exposure to malaria, yellow fever, typhoid fever, hepatitis A, B, and C, as well as trachoma, leprosy, or onchocerciasis must be considered in rare cases.
Occupational exposure
Occupational and hobby exposure may provide useful clues to the determined diagnostician, particularly in the farming or animal husbandry environment. Brucellosis may occur in livestock workers and slaughterhouse workers, while some cases of brucellosis are caused by consumption of unpasteurized milk products. Leptospirosis previously was seen in miners or sewer workers; however, most cases today follow exposure to water contaminated by domestic animals carrying the bacteria. Chlamydia psittaci infection results from parrot exposure. Cat scratch disease caused by Bartonella henselae infection and toxoplasmosis can follow feline exposure.
Localization of the Inflammatory Process
The anatomical location of the inflammatory process is one of the most important clues to pathogenesis and treatment.
Anterior uveitis
Anterior uveitis comprises inflammation, primarily affecting the anterior segment. Anterior uveitis is the most common form of intraocular inflammation.
Uveitic syndromes associated with primarily anterior segment involvement include HLA-B27 syndromes, herpes simplex and herpes zoster disease, Fuchs heterochromic iridocyclitis, and many arthritic syndromes. Secondary iatrogenic disease often is seen postoperatively, particularly following complications of surgery, trauma, scleral or seton implants, corneal transplants, capsular disruption, or fixed haptic and iris fixated intraocular lens implantation.
Intermediate uveitis
According to the SUN classification system (2005), the term intermediate uveitis is used when the primary site of inflammation is in the middle portion of the globe, including vitreus, peripheral retina, and pars plana. Pars planitis should be used only for that subset of intermediate uveitis where there is snowbank or snowball formation occurring in the absence of an associated infection or systemic disease (ie, idiopathic).
Sometimes, middle inflammation or anterior vitreous cells (called spillover uveitis) may occur, indicating that the primary source of disease is anterior. Intermediate uveitis is commonly associated with major granulomatous diseases (eg, tuberculosis, sarcoidosis, Lyme disease, lues).
Posterior uveitis
Posterior uveitis is inflammation of the choroid and the retina and includes retinochoroiditis, retinitis, and neuroretinitis. Spillover into the adjacent choroid, creating a retinochoroiditis or a chorioretinitis, may occur. Retinitis typically manifests by toxoplasmic or herpetic infection. Choroiditis may occur with any of the granulomatous uveitides (eg, tuberculosis, sarcoidosis, Lyme disease, syphilis), histoplasmosis, or more unusual syndromes, such as birdshot or serpiginous chorioretinitis. Papillitis may occur with toxoplasmosis, viral retinitis, lymphoma, or sarcoidosis.
Panuveitis
The term panuveitis is reserved for those situations in which there is no predominant site of inflammation, but inflammation is observed in the anterior chamber, vitreous, and retina and/or choroid. Diffuse uveitis, panuveitis, or endophthalmitis generally occur with overwhelming infections, such as infantile toxocariasis, postoperative bacterial endophthalmitis, or severe toxoplasmosis. Many of the granulomatous uveitides may produce a highly disseminated pattern, especially when delayed diagnosis occurs.
Character of the Inflammatory Process
The character of an ocular inflammatory disease can be described in terms of the pathology observed, distribution of lesions documented, location and character of keratic precipitates (KP) in the anterior chamber, presence or absence of synechiae, nodules, or fibrin, and presence of known identifier systemic correlates.
Pathology
Traditional terms have used the granulomatous and nongranulomatous monikers to describe the general character of intraocular inflammation. The term granulomatous is reserved for large, globular, mutton-fat keratic precipitates, Busacca (iris stroma) and Koeppe (iris margin) nodules, choroidal granulomata, and other indicators of pronounced severe inflammation.
Histopathologic correlates have been established in the literature. The classic granulomatous uveitides (eg, tuberculosis, sarcoidosis, Lyme disease, lues) often are manifested by a classic granulomatous inflammation pattern. Nongranulomatous inflammation generally describes a more benign intraocular appearance with smaller KP, less likelihood of synechiae formation, and fewer nodules.
Anterior chamber cells and flare
In acute anterior uveitis, the aqueous contains many cells and severe flare. In chronic cases, although the number of cells is considerably smaller, flare may be conspicuous. This is because of the structural alteration in the blood vessels due to long-term inflammation that leads to leaking of proteinaceous fluid and persistent flare. The grading schema for intraocular inflammation typically uses an ordinal scale ranging from 0 to 4+.
The SUN Working Group standardized the grading of anterior chamber cells and flare to achieve better compatibility between data from different groups and different studies. [7]
For anterior chamber cells, in a field size of 1X1-mm slit beam, the following grades were described: 0 (< 1 cell), 0.5+ (1-5 cells), 1+ (6-15 cells), 2+ (16-25 cells), 3+ (26-50 cells), and 4+ (>50 cells). The presence of hypopyon was recorded separately.
The grading for anterior chamber flare was standardized as follows: 0 (none), 1+ (faint), 2+ (moderate, iris and lens details clear), 3+ (marked, iris and lens details hazy), and 4+ (intense, fibrin or plastic aqueous).
Inactive anterior uveitis was described as rare cells or less. For short-term evaluation of treatment, improvement was described as a 2-step decrease in the level of inflammation or a decrease to grade 0. Worsening activity was a 2-step increase in the level of inflammation or an increase from grade 3+ to 4+. [7]
Keratic precipitates
KPs come in several varieties. Mutton-fat KPs occur in granulomatous inflammatory diseases, and they generally fill the Arlt triangle inferiorly. Arlt distribution is caused by convection currents within the anterior chamber and the cooler temperature in the inferior cornea. These larger granulomatous KPs will pigment and then shrink as inflammation abates or is controlled by steroid therapy. They often fail to disappear completely, and they may alter the endothelium where they rest, leaving a halo on the endothelium. Granulomatous deposits also may be seen in the anterior chamber angle by gonioscopy.
Nongranulomatous KPs are small to medium in size and white in color with Arlt distribution pattern. Old KPs accumulate pigment, and, as they begin to involute, shrink and disappear.
Stellate KPs are unique, fibrillar, dendriform, microscopic lesions found throughout the endothelium. No predilection exists for the center, periphery, or Arlt inferior triangle. Stellate KPs typically are seen in Fuchs heterochromic iridocyclitis, but they commonly are noted in herpes simplex, herpes zoster, and CMV-related infections. Stellate KPs can be seen in toxoplasmosis, but granulomatous or nongranulomatous KPs also are seen.
Peripheral KPs may be seen following intraocular surgery, with peripheral corneal edema following intracapsular cataract surgery (Brown syndrome), with herpes simplex or zoster uveitis, following acute angle-closure glaucoma, or after blunt ocular trauma.
Synechiae
Posterior synechiae typically form during acute inflammatory episodes at the location of Koeppe nodules. Both granulomatous and nongranulomatous cases may develop posterior synechiae quite rapidly, but they do not appear in pars planitis. Chronic anterior uveitis also frequently develops posterior synechiae, with or without gross papillary distortion.
Anterior synechiae occur in the angle during chronic or acute inflammation. They may develop during low-grade chronic inflammation with only flare seen in the anterior chamber without cells noted. Significant anterior synechiae in the presence of a functioning ciliary body and compromised trabecular outflow may create severe angle-closure glaucoma despite a deep anterior chamber. Anterior synechiae more commonly are found in deeply pigmented eyes, granulomatous diseases, and traumatized eyes.
Fibrin
Fibrinous exudates occur when overwhelming inflammation produces significant breakdown of the blood aqueous barrier and subsequent massive protein leakage. Fibrinous exudates most characteristically are seen in HLA-B27 disease, as well as severe granulomatous uveitis, postoperative endophthalmitis, trauma, and disseminated infections (eg, fungal endophthalmitis following intravenous drug abuse). Fibrin may form a retracting clot once resolution or aggressive therapy has been instituted.
Iris atrophy
The iris also plays a role in the differential of uveitic conditions. Diffuse iris atrophy is associated with herpes simplex, while herpes zoster more commonly causes sectoral atrophy. Fuchs heterochromic iridocyclitis causes iris atrophy from chronic low-grade inflammation and leads to the characteristic heterochromia and loss of iris stromal architecture.
Nodules
Koeppe nodules occur on the iris sphincter margin and can be seen in HLA-B27 disease, Fuchs heterochromic iridocyclitis, herpetic infections, and any granulomatous uveitis. Busacca nodules occur within the iris stroma and generally are accompanied by even more severe inflammation; therefore, they are less common than Koeppe nodules. These are seen with granulomatous uveitis and never with nongranulomatous uveitis; hence, they are valuable diagnostically.
Intraocular pressure
Intraocular pressure can give insight regarding the uveitic condition. Low intraocular pressure is due to decreased aqueous production in the acute phase. High intraocular pressure is found in virus-related uveitis. Some patients may have elevated intraocular pressure because of inflammatory debris in the trabecular meshwork.
Vitreitis
Vitreitis can be graded by the absence or presence of vitreus cells and grading of vitreus haze based on standard photos. The presence of snowball vitreus opacities is associated with granulomatous diseases (tuberculosis, sarcoidosis, Lyme disease). It may be seen in idiopathic pars planitis.
Chorioretinal lesion distribution
Retinal lesions may have several distribution patterns, which may provide invaluable diagnostic clues. Diffuse lesions may be seen in syphilis, sarcoidosis, birdshot retinochoroidopathy, or VKH. Focal lesions are more characteristic of toxoplasmosis. Diffuse inflammation is seen in vasculitic or ischemic disease, and sectorial retinitis may identify herpetic infection in acute retinal necrosis (ARN) or CMV retinitis. Peripheral retinitis may be seen in pars planitis, multiple sclerosis, sarcoidosis, punctate outer toxoplasmosis, or ARN.
Duration
The terms acute and chronic have been used inconsistently in the literature and have been used variably to refer to the onset of the uveitis, the duration of an attack of uveitis, or the course of uveitis.
The SUN Working Group standardized these terminologies. The onset of uveitis should be described either as sudden or insidious. The duration of an attack of uveitis should be described as either limited, if 3 months or less in duration, or persistent, if greater than 3 months in duration.
The term acute is used to describe the course of specific uveitic syndromes characterized by sudden onset and limited duration, such as HLA-B27-associated acute anterior uveitis. The term chronic is used to describe persistent uveitis characterized by prompt relapse (< 3 mo) after discontinuation of therapy (eg, chronic uveitis of Fuchs heterochromic cyclitis, JIA-associated uveitis, tuberculous uveitis). The term recurrent should be used to describe repeated episodes of uveitis separated by periods of inactivity without treatment.
Systemic correlates
The basic history for a patient with uveitis is simple and includes questions regarding demographics outlined in Classification and a focused pertinent review of systems. This review includes arthritis (hands, fingers, heels, toes, lower back, spine, weightbearing joints), rashes, GI disease (dysentery, colitis, gastritis), oral lesions, genital lesions, sexually transmitted disease, headache, neurologic symptoms, and pulmonary disease.
These specific questions contribute to the ophthalmologist's understanding of each patient presentation. The eye care professional maintains a uniquely advantageous position to provide the most focused cost-effective evaluation of the patient with uveitis.
Herpes titers are rarely helpful. Toxoplasmosis titers are useful only in the presence of at least somewhat typical retinitis scars. Angiotensin-converting enzyme (ACE) test results are often negative in sarcoidosis cases limited to the eye. Lysozyme is difficult at best to interpret. Lyme disease testing is not applicable to patients who have not been to endemic areas. Fungal titers are rarely applicable, unless typical posterior segment findings are suggestive. Screening sacroiliac films are insensitive in the absence of typical pelvic symptoms.
Many cases of mild, first episode unilateral uveitis may be associated with either trauma or an idiopathic viral or sinus infection. Since these cases present little risk of complications and recurrence, these patients are best served by symptomatic treatment, observation, and no initial diagnostic testing.
Etiology of the Inflammatory Process
When diagnostic testing has been performed, the specific etiology of the underlying process may be identified. Sometimes, only the category but not the actual cause of the inflammation may be known. This knowledge alone may be sufficient to initiate appropriate therapy.
Etiology provides the ultimate classification system. A useful technique to classify an inflammatory process, or any process within the eye for that matter, uses the 7 "I" system. This system places every source of ocular inflammation into 1 of 7 categories, with an eighth case for the process of elimination and frustration when all diagnostic means fail to reveal a specific etiology, as follows:
Inflammatory - Primary autoimmune disease
Infectious - Due to known ocular and systemic pathogens
Infiltrative - Referring to invasive neoplastic processes
Injurious - Trauma commonly seen in general offices
Iatrogenic - Surgery, inadvertent trauma, or medication
Inherited - Metabolic or dystrophic disease
Ischemic - Impaired circulation can cause inflammation
Idiopathic
A diagnosis of idiopathic uveitis implies not only that a thorough, specific, tailored, cost-effective diagnostic workup has been performed but also that treatable infectious diseases have been acceptably ruled out.
Classification
Age
Infant
Child
Adolescent
Young adult
Elderly adult
Demographics
Sex
Race
Residence location(s)
Travel
Immigration
Occupation
Hobbies
Nutritional and eating habits
Pets
Other illnesses
Stress events and factors
Personality factors
Social history
Smoking
Alcohol use
Drug abuse
Sexual orientation
Anatomical location
Anterior - Iritis, iridocyclitis, anterior cyclitis
Intermediate - Posterior cyclitis, pars planitis, hyalitis
Posterior - Retinitis, retinochoroiditis, chorioretinitis, choroiditis, papillitis
Panuveitis - Diffuse uveitis, endophthalmitis
Chronology or duration
Acute
Chronic
Recurrent
Character
Pathology - Granulomatous, nongranulomatous
Lesions - Focal, multifocal, disseminated, diffuse
KP pattern - Focal, central, disciform, Arlt triangle, stellate or diffuse, peripheral (rare)
Associated findings - Synechiae, fibrin, nodules
Practical Diagnostic Approach to Uveitis Outline
Naming
Patient identifier based upon a repeatable classification system
Meshing
Formulation of a differential diagnosis ordered by probability
Laboratory and medical evaluation
The diagnosis may require laboratory and medical evaluation guided by the history and physical examination. There is no standard battery of tests that needs to be ordered for all the patients with uveitis. Rather, a tailored approach should be taken based on the most likely cause for each patient.
Office testing
See the list below:
-
Photostress and Amsler grid (macular edema, macular retinitis)
-
Fluorescein angiography (macular edema, vasculitis, papillitis, choroiditis, retinitis, posterior scleritis)
-
Tear function testing - Schirmer and breakup time (Sjögren syndrome, sarcoidosis, connective tissue diseases)
-
Tear lysozyme or lactoferrin (Sjögren syndrome, sarcoidosis)
-
Conjunctival biopsy (sarcoidosis)
-
Aqueous paracentesis (infection, antibody titer, tumor, lens-induced uveitis, eosinophilia)
-
Visual fields (glaucoma, optic atrophy, papillitis)
-
Contrast sensitivity, color vision (optic neuritis, papillitis)
-
Glare testing (cataract, synechiae, capsular opacification)
-
Ultrasonography (posterior scleritis, retinal detachment, vitreitis)
-
Optical coherence tomography (OCT) (cystoid macular edema)
-
Delayed hypersensitivity skin testing for tuberculosis (purified protein derivative [PPD]), anergy for sarcoidosis (Candida or mumps), and rarely histoplasmosis or coccidioidomycosis
-
Electroretinogram (chloroquine toxicity, opaque media, birdshot choroidoretinopathy, retinitis pigmentosa, nonspecific)
-
Electro-oculogram (diabetic retinopathy, siderosis retinae, vitiliginous maculopathy, shallow retinal pigment epithelial detachments)
-
Vitrectomy (tumor, infection, antibody titer)
Specific clinical laboratory tests
See the list below:
-
Bacterial antibody testing (toxocariasis, toxoplasmosis, B henselae, brucellosis)
-
Viral antibody testing (herpes simplex virus, CMV, varicella-zoster virus, Epstein-Barr virus, hepatitis, HIV, human T lymphotrophic virus)
-
Luetic serology - Treponemal tests (fluorescent treponemal antibody absorption, microhemagglutination-Treponema pallidum) and nontreponemal tests (rapid plasma reagin, Venereal Disease Research Laboratory)
-
Lyme disease testing - Serology and polymerase chain reaction
-
Leptospirosis serology
-
Fungal serology - Blastomycosis, coccidioidomycosis, histoplasmosis serum antibodies
-
Connective tissue disease - Rheumatoid factor, antinuclear antibody, lupus anticoagulant, complement, protein electrophoresis, antineutrophil cytoplasmic antibody, and specific antinuclear antibodies (single stranded DNA, double stranded DNA, Smith, ribonucleoprotein)
-
Nonspecific inflammation - Erythrocyte sedimentation rate, C-reactive protein
-
Feces for parasites (Ascaris, Entamoeba histolytica, Escherichia coli, Endolimax nana, Giardia lamblia)
-
Angiotensin-converting enzyme (sarcoidosis)
-
Lysozyme (sarcoidosis, tuberculosis)
-
Major histocompatibility antigens (HLA-B27 syndromes, HLA-A29 in birdshot chorioretinopathy, and HLA-B51 in Behcet disease)
-
Standard tests - CBC count, differential, clotting factors, chemistry, urinalysis
-
Cryoglobulins (myeloma and other myeloproliferative neoplasms, rheumatoid arthritis, Sjögren syndrome, lupus erythematosus, Waldenström macroglobulinemia, hepatitis, CMV infections, infective endocarditis, mononucleosis, leprosy)
-
Complement levels, interleukin levels, circulating immune complexes
-
Chlamydial complement-fixation test
-
AIDS tests (ELISA and Western Blot)
Diagnostic imaging
See the list below:
-
Chest x-ray and spiral thin-cut CT scan (tuberculosis, sarcoidosis, histoplasmosis, tumor)
-
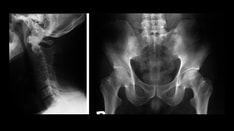
Sacroiliac films (HLA-B27, reactive arthritis, ankylosing spondylitis)
-
Orbital films, CT scan, or MRI (tumor, foreign body, thyroid, scleritis)
-
Skull films (congenital toxoplasmosis)
-
Joint films (rheumatoid arthritis, HLA-B27, JIA, lupus, gonorrhea)
-
Gallium scan (sarcoidosis)
Specialty consultations
See the list below:
-
Internal medicine and pediatrics (general evaluation, medication monitor)
-
Oncology (cytotoxic immunosuppressive medication monitor)
-
Infectious disease (diagnostic and therapeutic assistance, antibiotic medication monitor)
-
Dentistry, periodontology (diagnostic assistance with mucosal lesions)
-
Dermatology (diagnostic assistance with cutaneous lesions)
-
Rheumatology (diagnostic and therapeutic collaboration)
Therapeutic tests
See the list below:
-
Tuberculosis systemic therapy
-
Luetic systemic therapy
-
Lyme disease systemic therapy
-
Toxoplasmosis systemic therapy
-
Antiviral systemic therapy
-
Corticosteroid therapy (nonspecific)
-
Diagnostic lens removal (phacoanaphylaxis)
Invasive diagnostic testing
See the list below:
-
Diagnostic vitrectomy
-
Aqueous paracentesis
-
Vitreous tap
-
Corneal biopsy
-
Impression cytology
-
Conjunctival biopsy
-
Retinal biopsy
-
Choroidal biopsy
-
Impression cytology
Diagnosis and treatment
With a careful history, a directed physical examination, appropriate use of office diagnostic procedures, a tailored approach to laboratory testing, and selective medical consultations, the ophthalmologist can mesh a collection of useful data to obtain a diagnosis in up to 80% of referral uveitis patients and about 50% of uveitis patients in a comprehensive ophthalmology practice.
The main aim of uveitis treatment is to prevent visual loss, discomfort, and ocular morbidity. Depending upon the severity of the condition, the decision to start treatment is made. The initial treatment of uveitis is nonspecific and consists of mydriatic-cycloplegic agents, corticosteroids, immunomodulatory agents, and NSAIDs. [12] After conventional therapies, sustained-release intravitreal corticosteroid implants can be considered once noninfectious etiologies have been established. Nonbiodegradable implants recently approved by the FDA for posterior uveitis include the fluocinolone acetonide implants Retisert (Bausch and Lomb) and the recently introduced 2019 Durasert (EyePoint Pharmaceuticals), which can deliver an effective sustained release of drug over 3 years with minimal adverse effects. Popular biodegradable implants in use include the dexamethasone intravitreal implant (Ozurdex), which delivers steroids in a biphasic manner over 6 months. On the horizon are particulate drug-delivery systems into the suprachoroidal space that use small biodegradable colloidal particles (liposomes, microparticles, nanoparticles) for long-term delivery of medication. [13]
Later, as the result of laboratory investigations, special tests, and consultations ensues, specific treatment may be instituted. However, most cases that require treatment only need nonspecific treatment. Expeditious treatment based on a complete and organized diagnostic evaluation is best for the patient, the physician, and the economy.
See related CME at Advances in the Diagnosis and Treatment of Uveitis.