Background
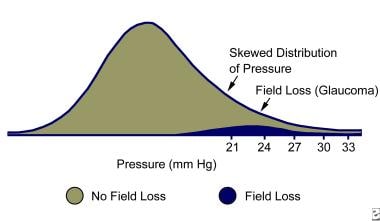
Ocular hypertension (OHT) can be used as a generic term referring to any situation in which intraocular pressure (IOP) is greater than 21 mm Hg, the widely accepted upper limit of normal intraocular pressure in the general population. [1] (See the image below.) The term makes no mention of whether or not glaucomatous nerve damage is present. It also depicts no particular time frame during which the elevated pressure has been measured.
The formal definition of ocular hypertension evolved in the latter part of the 20th century. [2] It was used as early as 1962 by Drance, but was not defined in English language publications until 1966 by Perkins and others.
Ocular hypertension is a condition in which the following criteria are met:
-
An intraocular pressure greater than 21 mm Hg in one or both eyes, as measured by applanation tonometry on 2 or more occasions
-
Absence of glaucomatous defects on visual-field testing
-
Normal appearance of the optic disc and nerve fiber layer
-
Anatomically normal, open angles on gonioscopy
-
Absence of ocular conditions contributing to the elevation of pressure, such as narrow angles, neovascular conditions, and uveitis
Despite early definitions, ocular hypertension has historically meant different things to different ophthalmologists. [2] Some glaucoma experts such as Hitchings stressed the point of not reading too much into the term. [3] Others, including Spaeth, advocated total disuse of the term secondary to its inherent ambiguity, preferring the term glaucoma suspect to more adequately convey uncertainty regarding the diagnosis and prognosis. [4] (See the image below.)
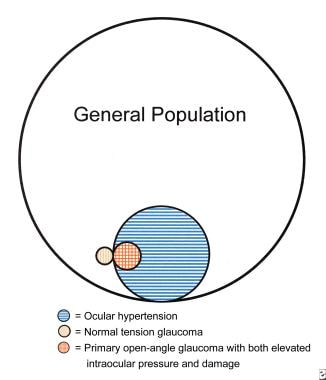 Diagram showing the relative proportion of people in the general population who have elevated pressure (horizontally shaded lines) and/or damage from glaucoma (vertically shaded lines). Notice that most have elevated pressure but no sign of damage (ie, ocular hypertensives), but there are those with normal pressures who still have damage from glaucoma (ie, normal tension glaucoma). (Diagram used by permission of M. Bruce Shields.) OHT = horizontal lines only NTG = vertical lines only POAG and other glaucomas with both elevated intraocular pressure and damage = overlapping horizontal and vertical lines
Diagram showing the relative proportion of people in the general population who have elevated pressure (horizontally shaded lines) and/or damage from glaucoma (vertically shaded lines). Notice that most have elevated pressure but no sign of damage (ie, ocular hypertensives), but there are those with normal pressures who still have damage from glaucoma (ie, normal tension glaucoma). (Diagram used by permission of M. Bruce Shields.) OHT = horizontal lines only NTG = vertical lines only POAG and other glaucomas with both elevated intraocular pressure and damage = overlapping horizontal and vertical lines
The Ocular Hypertension Treatment Study (OHTS) is a multicenter, prospective, randomized, controlled clinical trial studying more than 1800 research subjects, evaluating the safety and efficacy of medical treatment in preventing or delaying the onset of visual-field loss and/or optic nerve damage in patients with ocular hypertension who are at moderate risk for developing primary open-angle glaucoma (POAG). [5]
In this article, ocular hypertension refers to a state in which the eye(s) meet the above 5 criteria, in the absence of identifiable causes or cardinal signs of POAG. [6] Ocular hypertension is a condition requiring closer observation for the potential development of glaucomatous damage. [7, 8]
Pathophysiology
The exact pathophysiology of elevated intraocular pressure (IOP) in ocular hypertension is not known. In primary open-angle glaucoma, myocilin (MYOC) gene mutations have been found and determined to cause protein misfolding, making trabecular meshwork cells dysfunctional, with subsequent decrease in outflow facility and marked elevation of IOP. [9]
Elevated IOP is of great concern because it is the most established risk factor for the development of glaucoma. [10] Two theories of how IOP initiates glaucomatous damage include (1) onset of vascular dysfunction causing ischemia to the optic nerve and (2) mechanical dysfunction via cribriform plate compression of the neuronal axons.
In addition to vascular compromise and mechanically impaired axoplasmic flow, contemporary hypotheses of possible pathogenic mechanisms that underlie glaucomatous optic neuropathy include excitotoxic damage from excessive retinal glutamate, deprivation of neuronal growth factors, peroxynitrite toxicity from increased nitric oxide synthase activity, immune-mediated nerve damage, and oxidative stress. [11, 12]
The exact role that IOP plays in combination with these other factors and its significance in the initiation and progression of subsequent glaucomatous neuronal damage and cell death over time is still under debate. [13]
Epidemiology
Prevalence
Population studies such as the Framingham, Beaver Dam, Baltimore, Rotterdam, Barbados, and Egna-Neumarkt studies have estimated that 4-10% of the population older than 40 years will have IOPs of 21 mm Hg or higher without detectable signs of glaucomatous damage. [14] Ocular hypertension has a 10-15 times greater prevalence than POAG. [15]
Race-related demographics
Although Black individuals are considered to have a 3-4 times higher prevalence of POAG and larger cup-to-disc ratios compared with White individuals, the data are less clear concerning ocular hypertension. The Barbados Eye Study found the incidence of IOPs greater than 22 mm Hg to be 5 times higher in Blacks than in Whites. [14] The Baltimore Eye Survey found no difference in mean IOP between Blacks and Whites. [16] The Los Angeles Latino Eye Study found Latinos to be at higher risk of ocular hypertension than non-Latino Whites but lower than Blacks. [17]
Sex-related demographics
The Barbados Eye Study found ocular hypertension present more frequently in women. [14]
Age-related demographics
Mean IOP slowly rises with increasing age. Age older than 40 years is considered a risk factor for the development of ocular hypertension and POAG. [14]
Prognosis
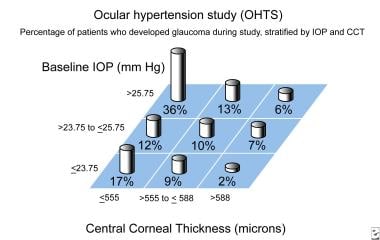
Prospective studies in the 1980s showed that among patients with elevated IOP, roughly 0.5-1% per year developed glaucoma over a period of 5-10 years. [18] The OHTS suggests that progression to glaucoma increases with higher IOPs and lower central corneal thickness (CCT) [5] (see image below) and that certain patient characteristics are associated with a greater than 2% annual risk of developing glaucoma. [19] Patient characteristics associated with this increased risk include the following:
-
Central corneal thickness of less than 555 μm - Annual risk of 3.4%
-
Vertical cup-to-disk ratio of greater than 0.30 - Annual risk of 2.5%
Morbidity and mortality
The Gutenberg Health Study found positive associations with higher IOP in an adult European cohort for systemic cardiovascular risk factors such as hypertension, diabetes, smoking, and obesity. [20]
Systemic morbidity and mortality also can result from the possible cardiopulmonary adverse effects of IOP-lowering medications.
With regard to ocular morbidity and mortality, retinal vascular occlusion may occur in approximately 3% of ocular hypertensive patients. [21]
Progression to glaucoma is the main source of ocular morbidity and mortality. Studies have shown that over a 5-year-period, the incidence of glaucomatous damage in ocular hypertensive patients increases with increasing IOP levels:
-
IOP of 21-25 mm Hg - Approximately 2.6-3%
-
IOP of 26-30 mm Hg - Range from 12-26%
-
IOP higher than 30 mm Hg - Approximately 42%
The Ocular Hypertension Treatment Study (OHTS) states that over a 5-year-period, patients with ocular hypertension and IOP levels of 24 mm Hg or more have a 10% overall risk of developing glaucoma. This risk can be cut in half by medical treatment. In 2004, more than 2 million individuals in the United States were diagnosed as having open-angle glaucoma. This number is projected to increase to more than 3 million by 2020. [22]
Patient Education
Patient education is essential to prevent possible progression to glaucoma. The patient who understands the chronic, potentially progressive nature of glaucoma is more likely to comply with therapy. [23, 24] Numerous handouts are available to patients, including the following:
-
"Understanding and Living with Glaucoma: A Reference Guide for People with Glaucoma and Their Families," Glaucoma Research Foundation, 1-800-826-6693.
Other patient resources are available from Prevent Blindness America, 1-800-331-2020.
-
Diagram of intraocular pressure distribution. Used with permission from Survey of Ophthalmology.
-
Flowchart for evaluation of a patient with suspected glaucoma. Used by permission of the American Academy of Ophthalmology.
-
Diagram showing the relative proportion of people in the general population who have elevated pressure (horizontally shaded lines) and/or damage from glaucoma (vertically shaded lines). Notice that most have elevated pressure but no sign of damage (ie, ocular hypertensives), but there are those with normal pressures who still have damage from glaucoma (ie, normal tension glaucoma). (Diagram used by permission of M. Bruce Shields.) OHT = horizontal lines only NTG = vertical lines only POAG and other glaucomas with both elevated intraocular pressure and damage = overlapping horizontal and vertical lines
-
Humphrey visual field, right eye, showing patient with advanced glaucomatous field loss. Notice both the arcuate extension from the blind spot (Bjerrum scotoma), as well as the loss nasally (nasal step), which often occurs early in the disease process. Courtesy of M. Bruce Shields.
-
Illustration of progressive optic nerve damage. Notice the deepening (saucerization) along the neural rim, along with notching and increased excavation/sloping of the optic nerve and circumlinear vessel inferiorly. Courtesy of M. Bruce Shields.
-
Example of progressive visual field loss over time (from top to bottom) in a patient with glaucoma. Notice the early appearance of an inferior nasal step and arcuate loss, with progressive enlargement and increasing density of the scotomata over time. Humphrey visual field courtesy of M. Bruce Shields.
-
Example of optic nerve asymmetry in a patient with glaucomatous damage, left eye, showing optic nerve excavation inferiorly similar to Image 5. Used by permission of M. Bruce Shields.
-
Glaucomatous optic nerve damage, with sloping and nerve fiber layer rim hemorrhage at the 7-o'clock position. Hemorrhage is indicative of progressive damage, usually due to inadequate pressure control. Further notching and pallor corresponding to the area of hemorrhage usually is seen several weeks after resorption of the blood. Courtesy of M. Bruce Shields.
-
Advanced glaucomatous damage with increased cupping and substantial pallor of the optic nerve head. Courtesy of M. Bruce Shields.
-
Correction values according to corneal thickness.
-
Ocular hypertension study (OHTS). Percentage of patients who developed glaucoma during this study, stratified by baseline intraocular pressure (IOP) and central corneal thickness (CCT).