Background
Choroidal ruptures are breaks in the choroid, the Bruch membrane, and the retinal pigment epithelium (RPE) that result from blunt ocular trauma (the most common eye injury). [1]
Choroidal rupture can be secondary to indirect or direct trauma. Cases secondary to direct trauma tend to be located more anteriorly and at the site of impact and parallel to the ora, whereas those secondary to indirect trauma occur posteriorly. These ruptures have a crescent shape and are concentric to the optic disc. Indirect choroidal ruptures are almost 4 times more common than direct ruptures. See the image below.
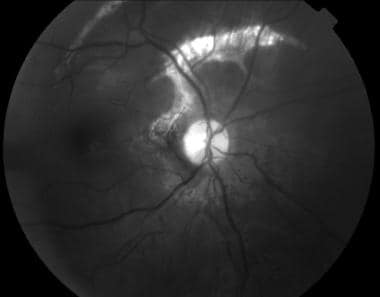 A 23-year-old man was in a motor vehicle accident 2 months before his presentation. His visual acuity is 20/400, and an afferent pupillary defect is present. Traumatic optic neuropathy and choroidal rupture are observed. This is a red-free photograph. (Courtesy of Jorge Gutierrez, MD.)
A 23-year-old man was in a motor vehicle accident 2 months before his presentation. His visual acuity is 20/400, and an afferent pupillary defect is present. Traumatic optic neuropathy and choroidal rupture are observed. This is a red-free photograph. (Courtesy of Jorge Gutierrez, MD.)
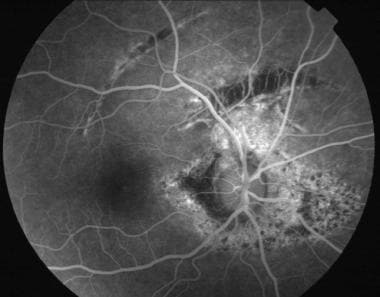 Mid-phase fluorescein angiogram in a 23-year-old man who was in a motor vehicle accident 2 months before his presentation. (Courtesy of Jorge Gutierrez, MD.)
Mid-phase fluorescein angiogram in a 23-year-old man who was in a motor vehicle accident 2 months before his presentation. (Courtesy of Jorge Gutierrez, MD.)
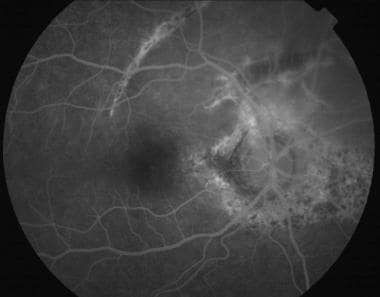 Late-phase fluorescein angiogram in a 23-year-old who man was in a motor vehicle accident 2 months before his presentation. (Courtesy of Jorge Gutierrez, MD.)
Late-phase fluorescein angiogram in a 23-year-old who man was in a motor vehicle accident 2 months before his presentation. (Courtesy of Jorge Gutierrez, MD.)
Pathophysiology
After blunt trauma, the ocular globe undergoes mechanical compression and then sudden hyperextension. Because of its tensile strength, the sclera can resist this insult; the retina is also protected because of its elasticity. The Bruch membrane does not have enough elasticity or tensile strength; therefore, it breaks.
Concurrently, the small capillaries in the choriocapillaris are damaged, leading to subretinal or sub-RPE hemorrhage. Hemorrhage in conjunction with retinal edema may obscure the choroidal rupture during the acute phases. The deep choroidal vessels are usually spared. As the blood clears, a white, curvilinear, crescent-shaped streak concentric to the optic nerve is seen.
During the healing phase, choroidal neovascularization (CNV) occurs. Vascular endothelial growth factor (VEGF) has been shown to be a key molecular player in the pathogenesis of CNV. In most cases, it involutes spontaneously.
In 15-30% of patients, CNV may arise again and lead to a hemorrhagic or serous macular detachment with concomitant visual loss. This usually occurs during the first year but can also occur decades later. If the rupture does not involve the fovea, good vision is expected.
Older age and macular rupture, the length of the rupture, and the distance of the rupture to the center of the fovea may be risk factors for CNV.
Epidemiology
Frequency
United States
Blunt ocular trauma is the most common type of eye injury. Approximately 5-10% of patients with such injury develop a choroidal rupture. Most eyes have a single rupture, but up to 25% of eyes have multiple ruptures. About 80% of ruptures occur temporal to the disc, and 66% involve the macula.
Mortality/Morbidity
Vision loss depends on whether the choroidal rupture involves the fovea and whether and where CNV occurs.
Sex
Men appear to be more prone to ocular trauma than women.
A male-to-female ratio of 5:1 is reported for choroidal ruptures. [2, 3]
Age
In most series, this condition occurs in patients aged 20-40 years. [2, 3]
-
A 23-year-old man was in a motor vehicle accident 2 months before his presentation. His visual acuity is 20/400, and an afferent pupillary defect is present. Traumatic optic neuropathy and choroidal rupture are observed. This is a red-free photograph. (Courtesy of Jorge Gutierrez, MD.)
-
Mid-phase fluorescein angiogram in a 23-year-old man who was in a motor vehicle accident 2 months before his presentation. (Courtesy of Jorge Gutierrez, MD.)
-
Late-phase fluorescein angiogram in a 23-year-old who man was in a motor vehicle accident 2 months before his presentation. (Courtesy of Jorge Gutierrez, MD.)